The process of bringing new drugs to market plays a crucial role in improving patient outcomes and advancing medical science. The United States, home to one of the world’s most rigorous regulatory systems for pharmaceuticals, has been making strides in accelerating drug approvals without compromising safety and efficacy. This article delves into the intricacies of the drug approval process in the US, exploring recent initiatives, challenges, and the potential impact on patients and the pharmaceutical industry.
The Current State of Drug Approvals
The journey from drug discovery to market availability is a long and complex one, often taking more than a decade and costing billions of dollars. The Food and Drug Administration (FDA) is the gatekeeper of this process, tasked with ensuring that new medications are safe and effective before they reach consumers.
The Traditional Approval Process
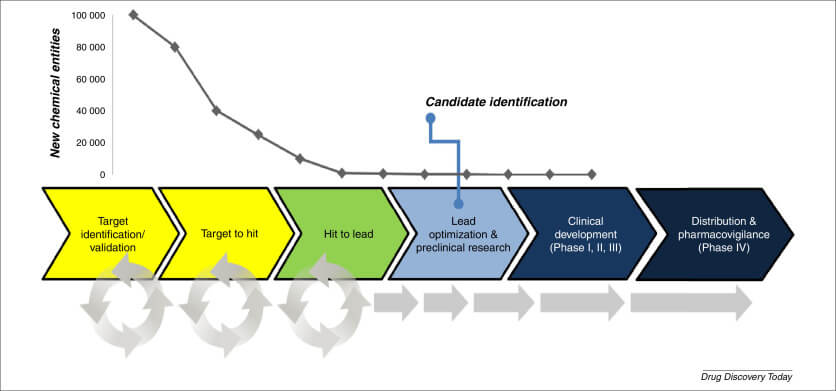
Traditionally, the drug approval process in the US has been known for its thoroughness and rigor. It typically involves several phases:
- Preclinical Testing: This phase involves laboratory and animal studies to assess the drug’s safety and potential efficacy.
- Investigational New Drug (IND) Application: Researchers submit an IND to the FDA, outlining their plans for human clinical trials.
- Clinical Trials: These are conducted in three phases, progressively increasing the number of participants and assessing safety and efficacy.
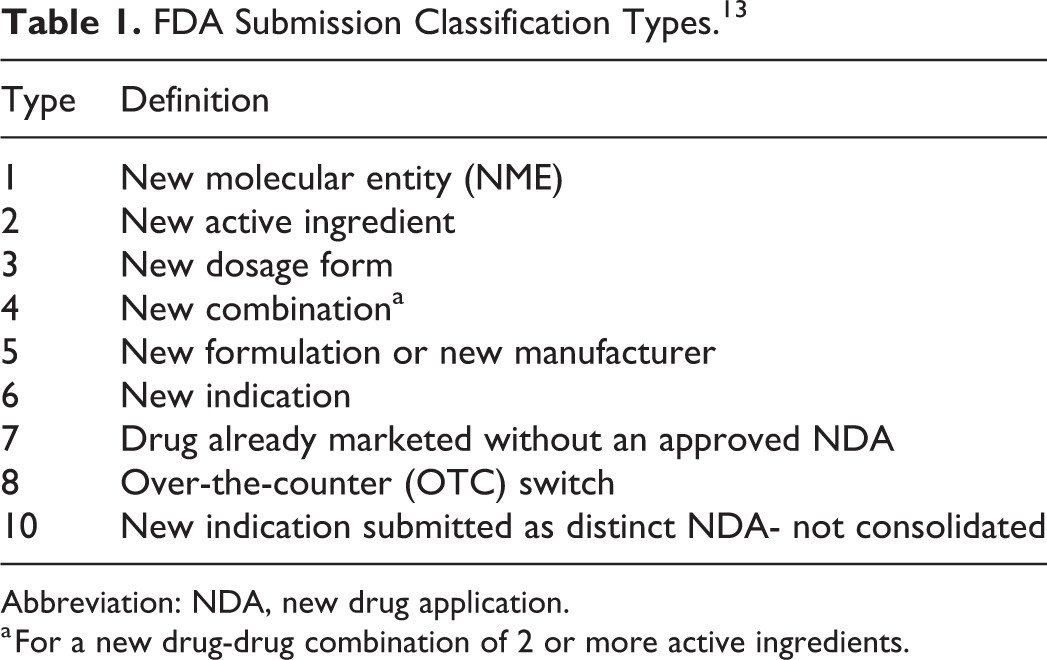
- New Drug Application (NDA): The sponsor submits comprehensive data from all studies to the FDA for review.
- FDA Review: The FDA thoroughly evaluates all submitted data before making a decision.
- Post-Market Safety Monitoring: Even after approval, the FDA continues to monitor the drug’s safety and efficacy.
This process, while crucial for ensuring patient safety, has often been criticized for its length and complexity. According to a study published in the Journal of the American Medical Association, the median time from the start of clinical trials to FDA approval was 7.3 years for drugs approved between 2015 and 2017.
The Need for Speed
The call for faster drug approvals has grown louder in recent years, driven by several factors:
- Urgent Medical Needs: Patients with life-threatening conditions can’t afford to wait years for potentially life-saving treatments.
- Scientific Advancements: Breakthroughs in genomics and personalized medicine have opened up new possibilities for targeted therapies.
- Economic Pressures: Lengthy approval processes increase development costs, which can be reflected in higher drug prices.
As Dr. Janet Woodcock, Director of the FDA’s Center for Drug Evaluation and Research, stated:
“We must find ways to reduce the time and cost of drug development, while still providing adequate information to assess the safety and efficacy of new drugs.”
FDA Initiatives to Accelerate Approvals
Recognizing the need for change, the FDA has implemented several initiatives aimed at speeding up the drug approval process without compromising on safety.
Breakthrough Therapy Designation
Introduced in 2012, the Breakthrough Therapy Designation is designed to expedite the development and review of drugs for serious or life-threatening conditions. To qualify, a drug must show preliminary clinical evidence of substantial improvement over existing therapies.
Key Benefits:
- Intensive FDA guidance on efficient drug development
- Rolling review of the marketing application
- Potential for priority review
Since its inception, the Breakthrough Therapy Designation has significantly impacted approval timelines. A study published in the New England Journal of Medicine found that drugs with this designation were approved an average of 3.2 years faster than those without it.
Fast Track Designation
The Fast Track program, designed to facilitate the development and expedite the review of drugs to treat serious conditions and fill unmet medical needs, offers several benefits:
- More frequent meetings and written communication with the FDA
- Eligibility for Accelerated Approval and Priority Review
- Rolling Review of the NDA
Accelerated Approval Pathway
This pathway allows for earlier approval of drugs that treat serious conditions and fill an unmet medical need based on a surrogate endpoint. A surrogate endpoint is a marker, such as a laboratory measurement or physical sign, that is thought to predict clinical benefit but is not itself a measure of clinical benefit.
Example: In oncology, tumor shrinkage might be used as a surrogate endpoint for overall survival.
Priority Review
Under Priority Review, the FDA aims to take action on an application within 6 months, compared to the standard 10 months. This designation is given to drugs that would provide significant improvements in the safety or effectiveness of treating, diagnosing, or preventing serious conditions.
The Impact of Accelerated Approvals
The FDA’s efforts to speed up drug approvals have had a significant impact on the pharmaceutical landscape and patient access to new treatments.
Faster Access to Innovative Therapies
According to FDA data, the median time from application to approval for novel drugs has decreased from 13.0 months in 2005 to 7.6 months in 2020. This reduction in approval time means that patients with serious conditions can access potentially life-saving treatments sooner.
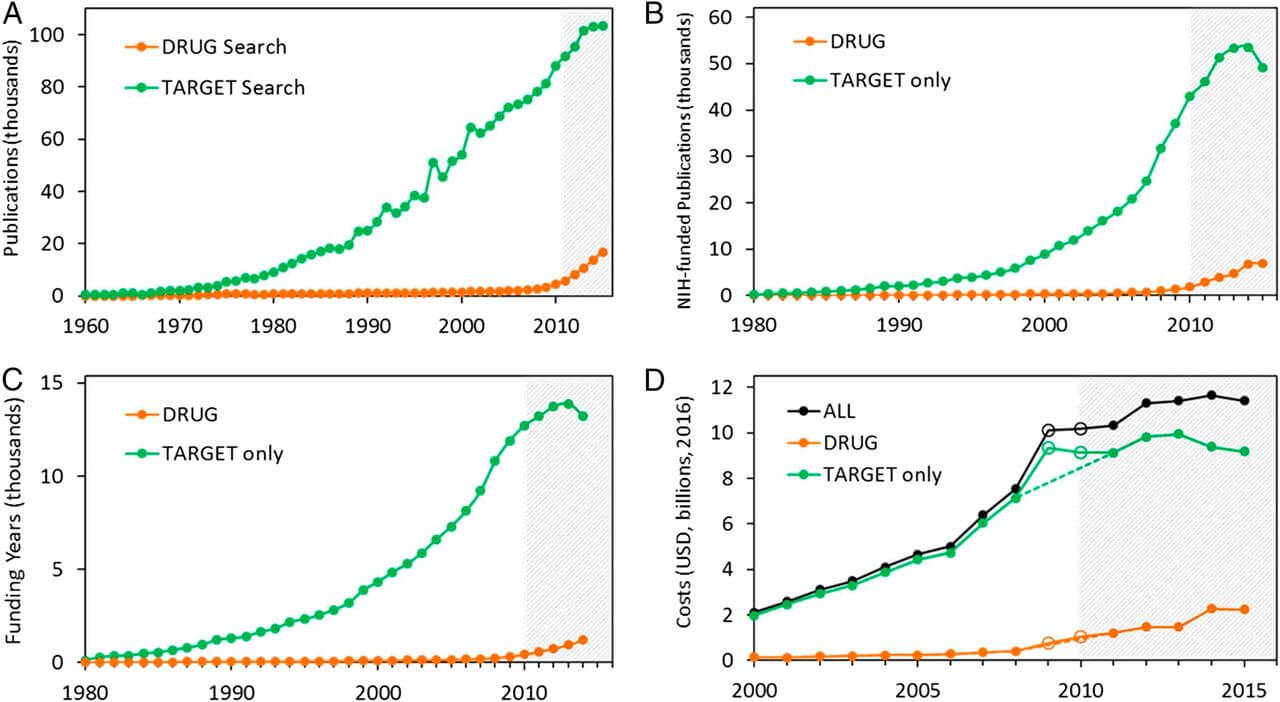
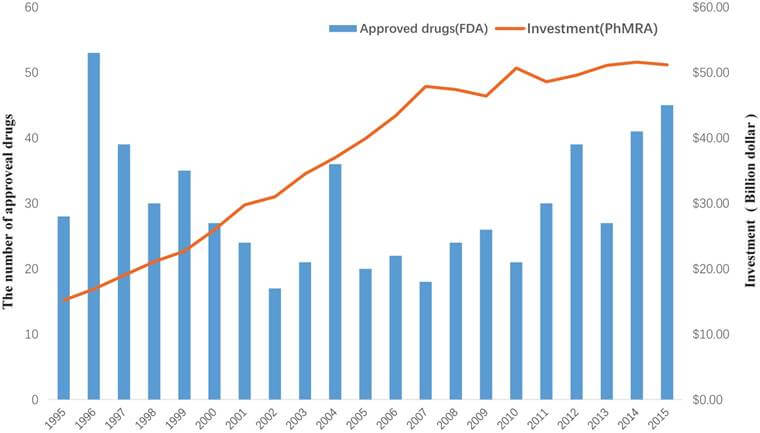
Increased Investment in Research and Development
The promise of faster approvals has encouraged pharmaceutical companies to invest more in research and development, particularly in areas of high unmet medical need. A report by the Pharmaceutical Research and Manufacturers of America (PhRMA) showed that R&D spending by member companies increased from $50.7 billion in 2010 to $91.1 billion in 2020.
Economic Benefits
Faster approvals can lead to significant economic benefits. A study by the Manhattan Institute estimated that accelerating drug approvals by just one year would create $4 trillion in value for patients and drug companies over a decade.
Challenges and Concerns
While the acceleration of drug approvals has brought many benefits, it has also raised some concerns among healthcare professionals and patient advocacy groups.
Safety Concerns
Critics argue that faster approvals might compromise patient safety by reducing the time available for thorough safety assessments. A study published in JAMA Internal Medicine found that drugs approved through accelerated pathways were more likely to receive safety-related label changes post-approval.
Limited Long-Term Data
Accelerated approval pathways often rely on surrogate endpoints rather than long-term clinical outcomes. This can lead to uncertainty about a drug’s long-term efficacy and safety profile.
Post-Market Surveillance
With drugs reaching the market faster, there’s an increased emphasis on post-market surveillance to detect any safety issues that may not have been apparent during clinical trials. The FDA’s Sentinel Initiative, launched in 2008, aims to proactively monitor the safety of medical products using electronic health data from multiple sources.
The Role of Technology in Accelerating Approvals
Advancements in technology are playing a crucial role in speeding up the drug approval process while maintaining rigorous safety standards.
Artificial Intelligence and Machine Learning
AI and machine learning algorithms are being used to:
- Analyze vast amounts of clinical trial data more quickly and accurately
- Predict potential drug interactions and side effects
- Identify suitable candidates for clinical trials
A report by Deloitte estimates that AI could reduce drug discovery times by up to 50% and cut costs by as much as 70%.
Real-World Evidence
The FDA is increasingly considering real-world evidence (RWE) in its decision-making process. RWE includes data collected from sources outside of traditional clinical trials, such as electronic health records and wearable devices.
Benefits of RWE:
- Provides insights into how drugs perform in diverse populations
- Helps identify rare side effects that may not be apparent in clinical trials
- Can support label expansions for existing drugs
Adaptive Clinical Trial Designs
Adaptive clinical trials allow for modifications to the trial design based on interim data analysis. This approach can:
- Reduce the overall time and cost of clinical trials
- Increase the likelihood of demonstrating a drug’s efficacy
- Minimize the number of patients exposed to ineffective treatments
The Global Perspective
While this article focuses on accelerating drug approvals in the US, it’s important to consider the global context.
International Harmonization Efforts
Initiatives like the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) aim to achieve greater harmonization in the interpretation and application of technical guidelines and requirements for pharmaceutical product registration.
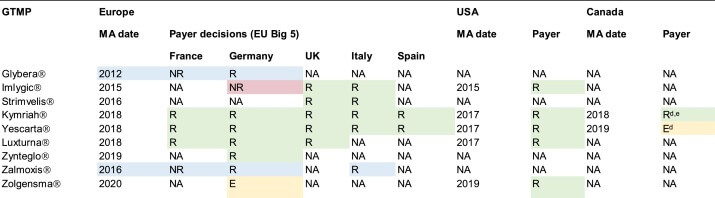
Comparison with Other Regulatory Agencies
The European Medicines Agency (EMA) and Japan’s Pharmaceuticals and Medical Devices Agency (PMDA) have also implemented programs to accelerate drug approvals. A comparative study published in the New England Journal of Medicine found that while the FDA approved more new drugs than the EMA or PMDA between 2011 and 2015, the median review times were similar across all three agencies.
The Future of Drug Approvals
As we look to the future, several trends are likely to shape the landscape of drug approvals in the US.
Personalized Medicine
Advances in genomics and biomarker research are paving the way for more targeted therapies. This shift towards personalized medicine may require new approaches to clinical trials and regulatory review.
Patient-Centered Drug Development
There’s a growing emphasis on incorporating patient perspectives throughout the drug development process. The FDA’s Patient-Focused Drug Development initiative aims to systematically gather patients’ perspectives on their conditions and available therapies.
Continuous Manufacturing
The FDA is encouraging the adoption of continuous manufacturing processes in pharmaceutical production. This approach could lead to more consistent product quality and faster scale-up of production, potentially reducing the time from approval to market availability.
Global Regulatory Convergence
As the pharmaceutical market becomes increasingly global, there’s a push for greater alignment of regulatory requirements across different countries. This could streamline the approval process for drugs intended for multiple markets.
Key Takeaways
- The FDA has implemented several initiatives to accelerate drug approvals, including Breakthrough Therapy Designation, Fast Track Designation, and the Accelerated Approval Pathway.
- These initiatives have significantly reduced approval times, with the median time from application to approval for novel drugs decreasing from 13.0 months in 2005 to 7.6 months in 2020.
- Faster approvals have led to quicker patient access to innovative therapies and increased investment in pharmaceutical R&D.
- Challenges include safety concerns, limited long-term data, and the need for robust post-market surveillance.
- Technology, including AI and machine learning, is playing a crucial role in accelerating drug approvals while maintaining safety standards.
- The future of drug approvals is likely to be shaped by personalized medicine, patient-centered drug development, and global regulatory convergence.
- Balancing speed with safety remains a critical challenge in the ongoing efforts to accelerate drug approvals.
FAQs
- Q: How long does the traditional drug approval process typically take?
A: The traditional drug approval process can take more than a decade from initial discovery to market availability, with the clinical trial phases alone often lasting 6-7 years. - Q: What is the difference between Fast Track and Breakthrough Therapy designations?
A: While both aim to expedite drug development and review, Breakthrough Therapy designation requires preliminary clinical evidence of substantial improvement over existing therapies, whereas Fast Track designation is based on nonclinical or clinical data demonstrating potential to address unmet medical needs. - Q: Does accelerated approval mean a drug is less safe?
A: Not necessarily. Accelerated approval pathways still require demonstration of safety and efficacy, but may rely on surrogate endpoints. These drugs are subject to rigorous post-market surveillance to ensure their safety and efficacy in real-world use. - Q: How is artificial intelligence being used in drug approvals?
A: AI is being used to analyze clinical trial data, predict potential drug interactions and side effects, identify suitable candidates for clinical trials, and potentially design more efficient clinical trials. - Q: What role do patients play in accelerating drug approvals?
A: Patients are increasingly involved in the drug development process through initiatives like the FDA’s Patient-Focused Drug Development program. Their perspectives help inform clinical trial design, endpoint selection, and benefit-risk assessments.
References
- https://jamanetwork.com/journals/jama/fullarticle/2762308
- https://www.fda.gov/news-events/speeches-fda-officials/remarks-janet-woodcock-md-fdas-efforts-speed-development-safe-and-effective-covid-19-vaccines-06302020
- https://www.nejm.org/doi/full/10.1056/NEJMoa1806651
- https://www.fda.gov/media/151146/download
- https://www.phrma.org/report/2021-phrma-annual-membership-survey
- https://www.manhattan-institute.org/html/accelerating-fda-approval-process-economic-benefits-and-clinical-risks-11245.html
- https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2758832
- https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-lshc-ai-in-drug-discovery.pdf
- https://www.nejm.org/doi/full/10.1056/NEJMsa1610625