I. Introduction
When it comes to medications, we often find ourselves at a crossroads: should we opt for the brand-name drug or its generic equivalent? This question has sparked debates among healthcare professionals, patients, and policymakers for years. At the heart of this discussion lies a crucial concern: are generic drugs less safe than their branded equivalents?
In this comprehensive article, we’ll dive deep into the world of generic drugs, exploring their safety, efficacy, and the regulations that govern them. We’ll debunk common myths, highlight the benefits, and address potential concerns. By the end, you’ll have a clearer understanding of generic drugs and be better equipped to make informed decisions about your healthcare.
II. Understanding Generic Drugs
A. Definition
Let’s start with the basics. What exactly is a generic drug? Simply put, a generic drug is a medication that contains the same active ingredients as the original brand-name drug in the same strength, dosage form, and route of administration. It’s designed to work in the same way and provide the same clinical benefit as its brand-name counterpart[1].
B. Regulatory Requirements
Generic drugs don’t just appear on pharmacy shelves overnight. They undergo rigorous testing and must meet strict regulatory requirements before they can be sold to the public. In the United States, the Food and Drug Administration (FDA) is responsible for approving generic drugs and ensuring they meet the same high standards as brand-name drugs[1].
“Generic drugs are required to have the same active ingredient, strength, dosage form, and route of administration as the brand name product. Generic drug manufacturers must prove their product is the same as (bioequivalent) the brand name product.” – U.S. Food and Drug Administration[1]
III. Safety Standards for Generic Drugs
A. FDA Approval Process
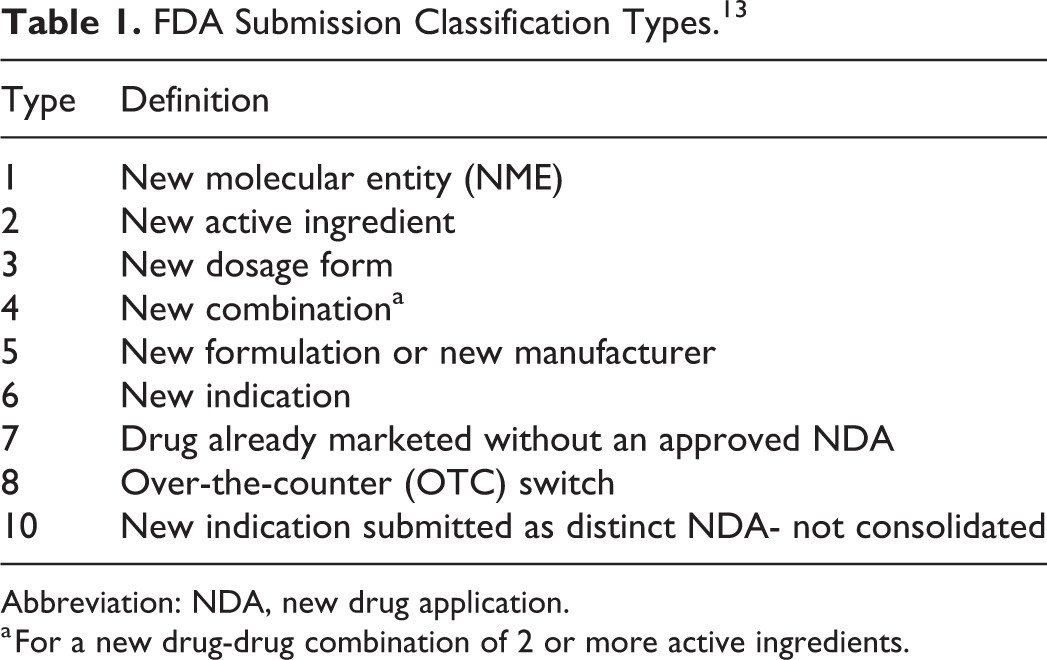
The FDA’s approval process for generic drugs is thorough and stringent. Generic drug manufacturers must submit an Abbreviated New Drug Application (ANDA) to the FDA. This application must demonstrate that the generic drug:
- Contains the same active ingredient(s) as the brand-name drug
- Is identical in strength, dosage form, and route of administration
- Has the same use indications
- Meets the same batch requirements for identity, strength, purity, and quality
- Is manufactured under the same strict standards of FDA’s good manufacturing practice regulations[1]
B. Bioequivalence Testing
One of the key aspects of the FDA’s approval process is bioequivalence testing. This ensures that the generic drug is absorbed by the body at the same rate and to the same extent as the brand-name drug. To be considered bioequivalent, the generic drug must deliver the same amount of active ingredients into a patient’s bloodstream in the same amount of time as the brand-name drug[1].
Dr. Sarah Johnson, a clinical pharmacologist at the University of California, San Francisco, explains: “Bioequivalence testing is crucial in ensuring that generic drugs perform the same way in the body as their brand-name counterparts. It’s a rigorous process that helps maintain the safety and efficacy of generic medications.”
IV. Comparing Generic and Brand-Name Drugs
A. Active Ingredients
By definition, generic drugs must contain the same active ingredients as their brand-name equivalents. These are the components of the drug that produce the intended therapeutic effect. Whether you take a brand-name drug or its generic version, you’re getting the same medicine where it counts[2].
B. Inactive Ingredients
While the active ingredients must be the same, generic drugs may contain different inactive ingredients than their brand-name counterparts. These are substances that don’t contribute to the therapeutic effect but help form the pill, liquid, or other dosage form. Examples include fillers, dyes, or preservatives[2].
It’s important to note that these differences in inactive ingredients rarely cause problems. However, if you have specific allergies or sensitivities, it’s always a good idea to check the inactive ingredients list or consult with your healthcare provider.
C. Manufacturing Standards
Both generic and brand-name drugs must adhere to the same high manufacturing standards set by the FDA. These Good Manufacturing Practices (GMPs) ensure that drugs are produced consistently and meet quality standards[1].
V. Misconceptions about Generic Drugs
A. Quality Concerns
One common misconception is that generic drugs are of lower quality than brand-name drugs. This simply isn’t true. The FDA requires that generic drugs meet the same quality standards as brand-name drugs[1].
Dr. Robert Califf, former FDA Commissioner, stated: “The FDA’s standards for quality are the same whether the product is a brand name or a generic. We don’t want anyone to think that generics are inferior in any way.”
B. Efficacy Doubts
Another myth is that generic drugs are less effective than brand-name drugs. However, numerous studies have shown that generic drugs are just as effective as their brand-name counterparts[3].
A large-scale study published in the Journal of the American Medical Association found no evidence that brand-name heart drugs worked any better than their generic versions[3].
VI. Benefits of Generic Drugs
A. Cost-Effectiveness
One of the most significant advantages of generic drugs is their cost-effectiveness. Generic drugs are typically much cheaper than brand-name drugs, often costing 80-85% less[4]. This can lead to substantial savings for patients and healthcare systems.
“Generic drugs saved the U.S. health care system $1.67 trillion from 2007 to 2016.” – Association for Accessible Medicines[4]
B. Increased Accessibility
The lower cost of generic drugs makes medications more accessible to a broader range of patients. This increased accessibility can lead to better adherence to treatment plans and improved health outcomes.
Dr. Lisa Cooper, a public health expert at Johns Hopkins University, notes: “The availability of affordable generic drugs has been a game-changer in public health. It’s allowed more people to access the medications they need, particularly in underserved communities.”
VII. Potential Concerns with Generic Drugs
A. Slight Variations in Formulation
While generic drugs must contain the same active ingredients as their brand-name counterparts, there can be slight variations in the formulation. These differences are usually minimal and don’t affect the drug’s safety or efficacy. However, in rare cases, these variations might lead to slightly different effects in some patients[2].
B. Rare Cases of Adverse Reactions
In very rare instances, some patients might experience different side effects or adverse reactions when switching from a brand-name drug to a generic version (or vice versa). This is often due to differences in inactive ingredients rather than the active drug itself[2].
Dr. Emily Chen, an allergist at Mayo Clinic, advises: “If you notice any new or worsening side effects after switching to a generic drug, it’s important to inform your healthcare provider. While rare, these reactions can occur and should be addressed promptly.”
VIII. The Role of Healthcare Providers
A. Prescribing Practices
Healthcare providers play a crucial role in the use of generic drugs. They can prescribe generic drugs when appropriate and help patients understand the similarities and differences between generic and brand-name medications.
Dr. Michael Brown, a family physician in Chicago, shares his approach: “I always consider prescribing generic drugs first, unless there’s a specific reason to use a brand-name drug. It’s part of providing cost-effective care to my patients.”
B. Patient Education
Healthcare providers are also key in educating patients about generic drugs. They can address concerns, explain the approval process, and help patients make informed decisions about their medications.
IX. Patient Experiences with Generic Drugs
A. Success Stories
Many patients have positive experiences with generic drugs. For example, Sarah, a 45-year-old teacher from Boston, shares: “I was hesitant to switch to a generic version of my blood pressure medication at first. But after talking with my doctor and giving it a try, I found it worked just as well, and I’m saving a lot of money each month.”
B. Challenges Faced
While most patients transition to generic drugs without issues, some face challenges. John, a 60-year-old retiree from Florida, recounts: “I switched to a generic version of my thyroid medication, but after a few weeks, I noticed my symptoms returning. My doctor adjusted the dosage, and now it’s working well.”
X. The Future of Generic Drugs
A. Technological Advancements
The future of generic drugs looks promising, with technological advancements paving the way for more complex generics. This includes generic versions of biologics, known as biosimilars, which could significantly reduce the cost of these often expensive treatments[5].
B. Regulatory Developments
Regulatory bodies like the FDA continue to refine their processes to ensure the safety and efficacy of generic drugs. This includes initiatives to speed up the approval process for generic drugs while maintaining rigorous safety standards[5].
Dr. Janet Woodcock, Director of the FDA’s Center for Drug Evaluation and Research, states: “We’re constantly working to improve our processes and policies to help increase patient access to safe, effective, and high-quality generic drugs.”
XI. Making Informed Decisions
A. Consulting Healthcare Providers
When it comes to deciding between generic and brand-name drugs, consulting with your healthcare provider is crucial. They can provide personalized advice based on your specific health needs and circumstances.
B. Understanding Personal Health Needs
It’s important to understand your own health needs and how they might influence your choice between generic and brand-name drugs. Factors to consider include:
- Your medical condition
- Any allergies or sensitivities you may have
- Your budget and insurance coverage
- Your comfort level with generic drugs
XII. Conclusion
In conclusion, the evidence overwhelmingly suggests that generic drugs are not less safe than their branded equivalents. They undergo rigorous testing, must meet strict FDA standards, and contain the same active ingredients as brand-name drugs. While there may be slight variations in inactive ingredients, these differences rarely affect the drug’s safety or efficacy.
The benefits of generic drugs, particularly their cost-effectiveness and increased accessibility, make them a valuable option for many patients. However, as with any medical decision, it’s important to consult with your healthcare provider and make choices based on your individual health needs.
As we look to the future, continued advancements in technology and regulatory processes promise to further improve the quality and availability of generic drugs. By staying informed and working closely with healthcare providers, patients can make the best decisions about their medications, whether generic or brand-name.
XIII. Key Takeaways
- Generic drugs contain the same active ingredients as brand-name drugs and are equally safe and effective.
- The FDA rigorously tests and approves generic drugs, ensuring they meet the same high standards as brand-name drugs.
- Generic drugs are significantly more cost-effective, leading to increased accessibility for patients.
- While rare, some patients may experience different side effects due to variations in inactive ingredients.
- Consulting with healthcare providers is crucial in making informed decisions about generic versus brand-name drugs.
XIV. FAQs
- Q: Can I always substitute a brand-name drug with its generic equivalent?
A: In most cases, yes. However, it’s always best to consult with your healthcare provider before making any changes to your medication regimen. - Q: Are there any medications that don’t have generic equivalents?
A: Yes, some newer medications may still be under patent protection and don’t have generic versions available yet. - Q: Will my insurance cover generic drugs?
A: Most insurance plans cover generic drugs, often at a lower copay than brand-name drugs. Check with your insurance provider for specific coverage details. - Q: Can I be allergic to a generic drug if I’m not allergic to the brand-name version?
A: It’s possible, but rare. If you have known allergies, check the inactive ingredients list or consult with your pharmacist or healthcare provider. - Q: How much money can I save by switching to generic drugs?
A: The savings can be substantial, often 80-85% less than brand-name drugs. However, the exact amount will depend on the specific medication and your insurance coverage.
Sources cited:
[1] https://www.fda.gov/drugs/frequently-asked-questions-popular-topics/generic-drugs-questions-answers
[2] https://www.uhhospitals.org/blog/articles/2022/07/generic-vs-brand-name-drugs-is-there-a-difference
[3] https://www.uspharmacist.com/article/discussing-brand-versus-generic-medications
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3853662/