In the ever-evolving landscape of pharmaceuticals, biosimilars have emerged as game-changers. But with their rise comes a unique challenge: how do we name these biological copycats? Let’s dive into the fascinating world of biosimilar naming and uncover why it’s more than just a matter of semantics.
What Are Biosimilars, Anyway?
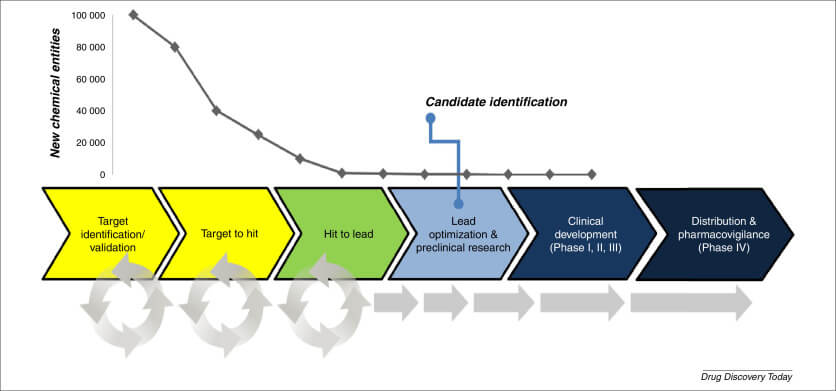
Before we jump into the naming conundrum, let’s get our basics straight. Biosimilars are like the cover bands of the pharmaceutical world – they’re not quite the original, but they’re pretty darn close. These biological products are highly similar to already-approved biological medicines, known as reference products[1].
The Biosimilar Boom
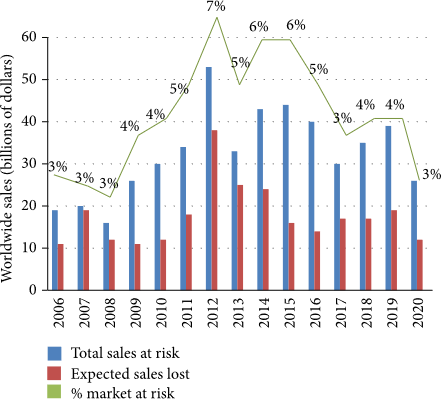
Biosimilars have been making waves in the healthcare industry, and for good reason. They offer a more affordable alternative to expensive biological drugs, potentially saving billions in healthcare costs. But with great power comes great responsibility – and in this case, that responsibility is proper naming.
The Naming Game: Why It Matters
You might be wondering, “What’s in a name?” Well, when it comes to biosimilars, quite a lot actually. The naming of biosimilars isn’t just a bureaucratic exercise – it has real-world implications for patient safety, pharmacovigilance, and market competition.
Safety First: Traceability and Pharmacovigilance
Imagine you’re a doctor trying to track a patient’s reaction to a specific biosimilar. If the naming system is unclear, it could be like trying to find a needle in a haystack. Clear, distinct names help healthcare professionals accurately identify and track biosimilars, ensuring patient safety and effective pharmacovigilance[2].
Market Dynamics: Competition and Confusion
The naming system also plays a crucial role in shaping market dynamics. A well-designed naming convention can foster healthy competition, while a confusing one might lead to market distortions. It’s like trying to choose between different brands of cereal – if the names are too similar, you might end up with bran flakes instead of frosted flakes!
The Global Naming Debate: A Tale of Two Approaches
When it comes to biosimilar naming, the world is divided. It’s like the great “gif” pronunciation debate, but with higher stakes.
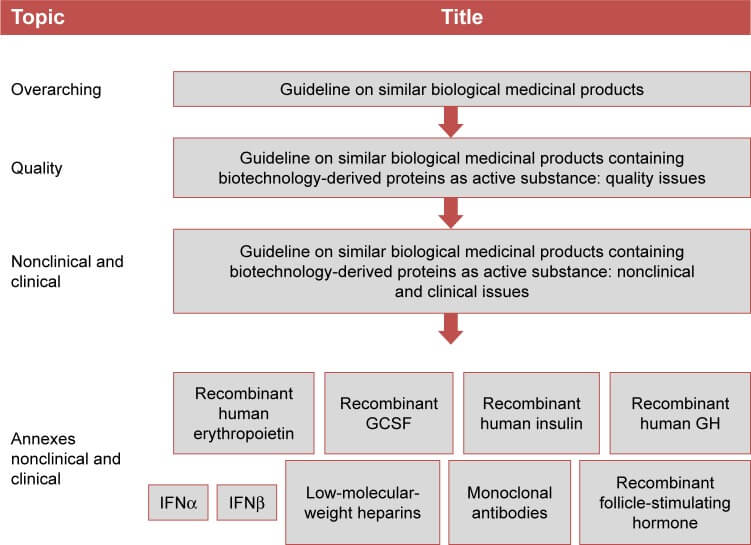
The WHO’s International Nonproprietary Name (INN) System
The World Health Organization (WHO) has proposed a system where biosimilars share the same International Nonproprietary Name (INN) as their reference product, with an added four-letter suffix to distinguish them[3]. It’s like adding a unique hashtag to differentiate between similar posts on social media.
The FDA’s Approach: Similar, But Different
The U.S. Food and Drug Administration (FDA) has taken a slightly different route. They require biosimilars to have the same core name as the reference product, followed by a four-letter suffix. However, unlike the WHO system, this suffix is devoid of meaning[1]. It’s like giving twins the same first name but different middle names – similar, but distinct.
“The naming and naming conventions for biosimilars are critical for their appropriate use and for pharmacovigilance.” – Dr. Janet Woodcock, Director of the Center for Drug Evaluation and Research at the FDA[4].
The Naming Convention Showdown: Pros and Cons
Like any good debate, the biosimilar naming convention has its supporters and detractors. Let’s break down the arguments for and against different naming approaches.
The Case for Shared INNs
Proponents of shared INNs argue that this approach:
- Emphasizes the similarity between biosimilars and their reference products
- Facilitates substitution and promotes competition
- Aligns with the naming of small-molecule generic drugs
The Argument for Distinct Names
On the other hand, advocates for distinct names contend that:
- Unique names enhance pharmacovigilance and traceability
- Distinct identifiers reduce the risk of inadvertent substitution
- Separate names acknowledge the complex nature of biological products
The Stakeholder Perspective: Who Wants What?
The biosimilar naming debate isn’t just an academic exercise – it has real-world stakeholders with vested interests. Let’s take a look at who’s rooting for what.
Innovator Companies: Distinction is Key
Unsurprisingly, companies that produce original biologics often advocate for distinct names. They argue that biosimilars, while similar, are not identical to reference products and should be clearly differentiated[5].
Biosimilar Manufacturers: Similarity Sells
On the flip side, biosimilar manufacturers generally prefer shared INNs. They believe that emphasizing similarity will promote acceptance and uptake of biosimilars[5].
Healthcare Providers: Clarity is Crucial
Doctors and pharmacists are caught in the middle. They need a system that’s clear enough to prevent confusion but doesn’t unnecessarily complicate prescribing and dispensing[2].
Patients: Safety and Affordability
Patients have a dual interest: they want assurance of safety through clear identification, but also hope for increased access to affordable treatments through biosimilar competition[2].
Global Harmonization: A Pipe Dream?
With different countries adopting different approaches, the dream of a globally harmonized naming system seems as elusive as a unicorn. But is it really impossible?
The Benefits of Harmonization
A globally harmonized naming system could:
- Enhance global pharmacovigilance
- Facilitate international trade in biosimilars
- Reduce confusion for healthcare providers and patients
The Challenges of Alignment
However, achieving harmonization faces several hurdles:
- Different regulatory frameworks across countries
- Varying priorities and concerns among stakeholders
- Existing investments in country-specific systems
The Future of Biosimilar Naming: Crystal Ball Gazing
As we peer into the future of biosimilar naming, what can we expect? While I don’t have a crystal ball, we can make some educated guesses based on current trends and expert opinions.
Increased Standardization
As the biosimilar market matures, we’re likely to see increased pressure for standardization. This could lead to more countries aligning their naming conventions, if not globally, then at least regionally.
Technology to the Rescue
Advancements in health information technology could potentially resolve some of the current naming challenges. For instance, electronic health records could incorporate both shared INNs and unique identifiers, providing the best of both worlds.
Evolving Regulatory Landscape
As regulators gain more experience with biosimilars, we might see further refinements to naming conventions. This could involve tweaks to existing systems or potentially entirely new approaches.
The Impact on Market Access and Uptake
The naming convention doesn’t just affect how we identify biosimilars – it can have far-reaching implications for market access and uptake.
Physician Perception and Prescribing Habits
The naming system can influence how physicians perceive biosimilars. A system that emphasizes similarity might increase confidence in prescribing biosimilars, while one that stresses distinction could reinforce the idea that biosimilars are fundamentally different from reference products[5].
Patient Acceptance and Adherence
For patients, the naming system can affect their understanding and acceptance of biosimilars. Clear, intuitive names could enhance patient confidence and potentially improve medication adherence.
Payer Policies and Formulary Decisions
The naming convention can also impact how payers view and categorize biosimilars. This, in turn, can influence formulary decisions and reimbursement policies, ultimately affecting patient access to these medications[5].
Biosimilar Naming in Practice: Real-World Examples
Let’s look at some real-world examples to see how biosimilar naming plays out in practice.
Filgrastim: A Tale of Two Names
In the U.S., the biosimilar for filgrastim is called “filgrastim-sndz” (brand name Zarxio), while in Europe, it shares the INN “filgrastim” with its reference product[1]. This illustrates the divergence in naming approaches between regions.
Infliximab: Same Name, Different Suffixes
In the U.S., biosimilars of infliximab include “infliximab-dyyb” (Inflectra) and “infliximab-abda” (Renflexis)[1]. These examples show how the FDA’s suffix system works in practice.
The Role of Education in Biosimilar Naming
With all the complexity surrounding biosimilar naming, education plays a crucial role in ensuring proper understanding and use.
Healthcare Provider Education
Healthcare providers need to be educated about the naming conventions and their implications. This includes understanding how to interpret different naming systems and how to accurately report adverse events.
Patient Education
Patients also need to be informed about biosimilars and their naming. This can help prevent confusion and ensure that patients can accurately identify and discuss their medications with healthcare providers.
Pharmacist Training
Pharmacists play a key role in dispensing biosimilars and need to be well-versed in the naming conventions. This is crucial for ensuring accurate dispensing and effective communication with both healthcare providers and patients.
The Economic Implications of Biosimilar Naming
The naming convention for biosimilars isn’t just a matter of semantics – it can have significant economic implications.
Impact on Competition
The naming system can influence the level of competition in the biosimilar market. A system that emphasizes similarity might foster more robust competition, potentially leading to lower prices[5].
Effects on Marketing and Branding
The naming convention also affects how companies can market and brand their biosimilars. This, in turn, can impact market share and profitability.
Implications for Healthcare Costs
Ultimately, the naming system’s effects on competition and market dynamics can influence overall healthcare costs. A system that promotes biosimilar uptake could lead to significant cost savings for healthcare systems[5].
Biosimilar Naming and Intellectual Property
The intersection of biosimilar naming and intellectual property law adds another layer of complexity to this issue.
Trademark Considerations
The naming convention can impact trademark strategies for both innovator and biosimilar companies. Companies need to navigate the delicate balance between distinguishing their products and adhering to naming regulations.
Patent Implications
While the name itself isn’t patentable, the naming system can indirectly affect patent strategies and litigation in the biosimilar space.
The Role of International Organizations in Biosimilar Naming
International organizations play a crucial role in shaping the global landscape of biosimilar naming.
World Health Organization (WHO)
The WHO’s Biological Qualifier (BQ) proposal has been influential in the global debate on biosimilar naming[3]. While not universally adopted, it has shaped many countries’ approaches.
International Conference on Harmonisation (ICH)
The ICH, which brings together regulatory authorities and pharmaceutical industry representatives, has also been involved in discussions about harmonizing biosimilar naming practices globally.
Biosimilar Naming: A Balancing Act
At its core, the biosimilar naming debate is about striking the right balance between various competing interests.
Safety vs. Access
The naming system needs to ensure patient safety through clear identification and traceability, while also promoting access to affordable biosimilars.
Distinction vs. Similarity
The naming convention must acknowledge the distinct nature of biosimilars while also emphasizing their similarity to reference products.
Global Harmony vs. Local Needs
There’s a tension between the desire for global harmonization and the need to accommodate local regulatory and market conditions.
Key Takeaways
- Biosimilar naming is more than just a bureaucratic exercise – it has significant implications for patient safety, market dynamics, and healthcare costs.
- There are two main approaches to biosimilar naming: shared INNs with distinguishing suffixes (WHO approach) and distinct names with meaningless suffixes (FDA approach).
- Different stakeholders have varying preferences for naming conventions, reflecting their diverse interests and concerns.
- Global harmonization of biosimilar naming remains a challenge due to differing regulatory frameworks and priorities across countries.
- The naming convention can significantly impact market access, uptake, and competition in the biosimilar space.
- Education plays a crucial role in ensuring proper understanding and use of biosimilar naming conventions among healthcare providers, patients, and pharmacists.
- The biosimilar naming debate ultimately requires balancing various competing interests, including safety, access, distinction, and similarity.
FAQs
- Q: Why can’t we just use the same names for biosimilars as their reference products?
A: While biosimilars are highly similar to their reference products, they are not identical. Using distinct names helps ensure accurate identification, traceability, and pharmacovigilance. - Q: How does the biosimilar naming system affect patient safety?
A: A clear naming system allows healthcare providers to accurately track which specific product a patient received. This is crucial for monitoring adverse events and ensuring patient safety. - Q: Does the naming system affect the interchangeability of biosimilars?
A: The naming system itself doesn’t determine interchangeability, which is a regulatory designation. However, it can influence perceptions of similarity and potentially impact substitution practices. - Q: How do biosimilar names differ between the U.S. and Europe?
A: In the U.S., biosimilars have a core name shared with the reference product plus a unique four-letter suffix. In Europe, biosimilars generally share the same INN as their reference product without a suffix. - Q: Could the biosimilar naming system change in the future?
A: Yes, it’s possible. As regulators gain more experience with biosimilars and as the market evolves, we might see further refinements or changes to naming conventions.