In the complex world of drug approvals and regulations, one question often lurks in the shadows: Can drug companies bribe the FDA? It’s a loaded question that touches on the very heart of public health, corporate ethics, and governmental integrity. Today, we’re going to dive deep into this controversial topic, exploring the intricacies of pharmaceutical influence and the safeguards in place to protect the public interest.
The FDA: Guardian of Public Health or Pawn in Big Pharma’s Game?
The Food and Drug Administration (FDA) stands as the gatekeeper between pharmaceutical companies and the American public. Its role is crucial: to ensure that the drugs we take are safe and effective. But with billions of dollars at stake in the pharmaceutical industry, it’s natural to wonder if this guardian can be swayed by the very entities it’s meant to regulate.
The Power of the Pharmaceutical Industry
Let’s face it: the pharmaceutical industry is a behemoth. With annual revenues that surpass the GDP of many countries, these companies wield enormous financial power. In 2020 alone, the global pharmaceutical market was valued at about $1.27 trillion. That’s a lot of zeroes, folks!
The FDA’s Crucial Role
On the other side of the equation, we have the FDA. This agency is responsible for protecting public health by regulating food, drugs, medical devices, and cosmetics. It’s a massive undertaking, and the decisions made by the FDA can make or break a drug company’s future.
The Anatomy of Influence: How Drug Companies Interact with the FDA
Now, let’s get to the meat of the matter. How exactly do drug companies interact with the FDA? Is it all above board, or are there shadowy dealings behind closed doors?
Legitimate Channels of Communication
First and foremost, it’s important to understand that there are many legitimate ways for pharmaceutical companies to communicate with the FDA. These include:
- Formal meetings during the drug development process
- Submission of clinical trial data
- Responses to FDA queries and concerns
These interactions are necessary and beneficial, ensuring that drug development aligns with regulatory requirements.
The Gray Areas: Advisory Committees and Revolving Doors
However, there are areas where the lines can blur. One such area is the FDA’s use of advisory committees, which often include experts who have financial ties to pharmaceutical companies.
“Of the more than $24 million in personal payments or research support from industry to the 16 top-earning advisers—who received more than $300,000 each—93% came from the makers of drugs those advisers previously reviewed or from competitors.”[1]
This statistic raises eyebrows and questions about potential conflicts of interest.
Another concern is the “revolving door” between the FDA and the pharmaceutical industry. It’s not uncommon for FDA officials to later work for drug companies, and vice versa. While this can bring valuable expertise to both sides, it also raises concerns about impartiality.
The Bribery Question: Fact or Fiction?
Now, let’s address the elephant in the room. Can drug companies actually bribe the FDA? The short answer is: it’s complicated.
Direct Bribery: A High-Risk, Low-Reward Strategy
Direct bribery of FDA officials is illegal and extremely risky. The consequences for both the company and the individuals involved would be severe, including criminal charges, massive fines, and irreparable damage to reputation.
Indirect Influence: The More Subtle Approach
However, influence can take more subtle forms. These might include:
- Funding research that paints their products in a favorable light
- Providing “consulting fees” to doctors who sit on FDA advisory committees
- Lobbying Congress to influence FDA policies and funding
While not technically bribery, these practices can still raise ethical concerns.
Case Studies: When Influence Goes Too Far
Let’s look at some real-world examples where pharmaceutical companies have been accused of crossing the line.
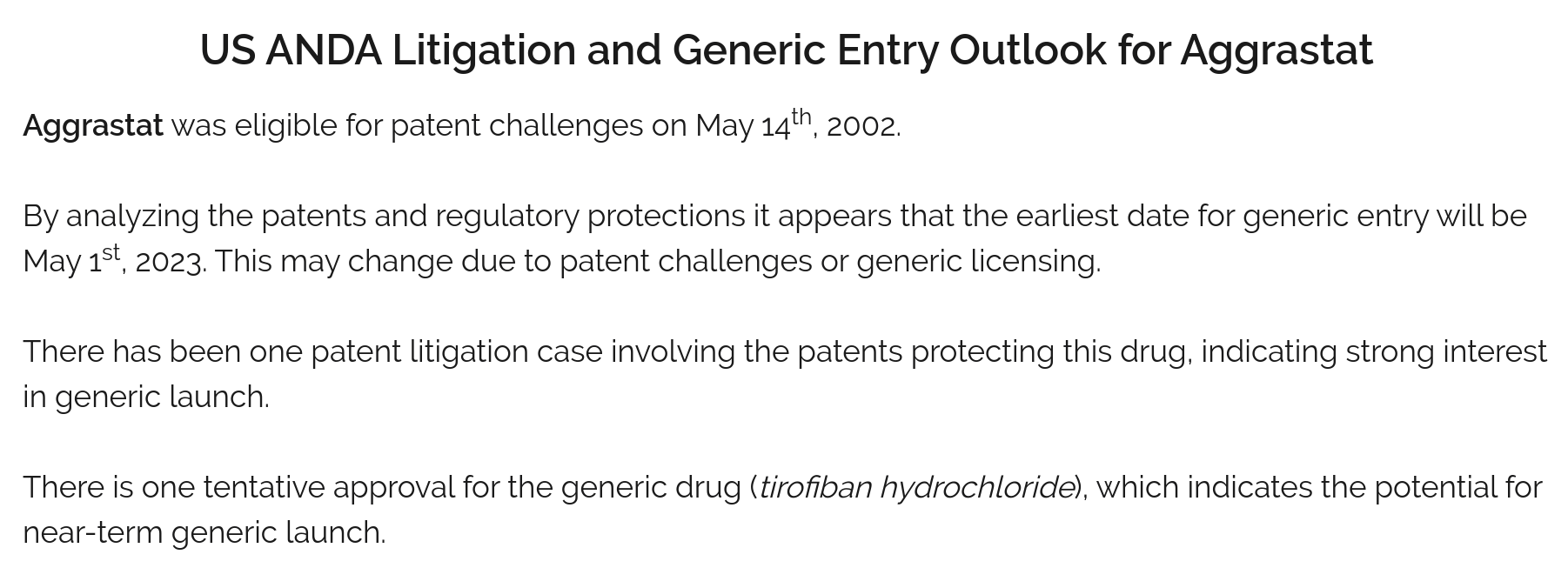
The AstraZeneca Saga
In 2010, AstraZeneca faced scrutiny over its anticlotting drug Brilinta. The company was accused of manipulating clinical trial data and providing financial incentives to doctors who prescribed the drug.
“From 2013 to 2016, the period recorded by Open Payments, he or Duke on his behalf received more than $63,000 from AstraZeneca and $1.3 million from competitors.”[1]
This case highlights the complex web of financial relationships between drug companies, researchers, and prescribing doctors.
The Generic Drug Scandal of the 1980s
In a more direct example of corruption, the generic drug industry was rocked by scandal in the late 1980s. Several FDA officials were found to have accepted bribes from generic drug manufacturers in exchange for expedited approvals.
“As a result of those investigations and investigations conducted by FDA, four FDA employees were found to have accepted illegal gratuities from generic drug manufacturers.”[5]
This scandal led to significant reforms in FDA procedures and oversight.
The Watchdogs: Safeguards Against Corruption
Given these concerns, what safeguards are in place to prevent undue influence on the FDA?
Conflict of Interest Regulations
The FDA has strict rules about conflicts of interest for its employees and advisory committee members. These include:
- Financial disclosure requirements
- Recusal from decisions involving companies where conflicts exist
- Limits on post-employment activities in the private sector
Transparency Initiatives
In recent years, there’s been a push for greater transparency in the relationships between pharmaceutical companies and healthcare professionals. The Physician Payments Sunshine Act, part of the Affordable Care Act, requires drug and device companies to publicly report payments made to doctors and teaching hospitals.
Whistleblower Protections
Whistleblower laws provide protection and incentives for individuals who report wrongdoing. These have been crucial in uncovering instances of fraud and corruption in the pharmaceutical industry.
The Role of Public Scrutiny and Media Oversight
Never underestimate the power of public scrutiny and media oversight. Investigative journalism has played a crucial role in exposing potential conflicts of interest and questionable practices in the pharmaceutical industry.
The Impact of Investigative Reporting
Journalists and researchers have uncovered numerous instances of potential conflicts of interest and questionable practices. For example, a 2018 investigation by Science magazine revealed widespread financial ties between pharmaceutical companies and FDA advisers after drug approvals[1].
The Power of Public Opinion
Public opinion can be a powerful force in shaping policy and corporate behavior. When questionable practices come to light, the resulting public outcry can lead to significant changes in how both the FDA and pharmaceutical companies operate.
The Global Perspective: How Other Countries Handle Pharmaceutical Regulation
To put the U.S. system in context, it’s worth looking at how other countries handle pharmaceutical regulation.
The European Medicines Agency (EMA)
The EMA, Europe’s equivalent to the FDA, has its own set of regulations and safeguards. While similar in many ways to the FDA, there are some key differences in how it interacts with pharmaceutical companies.
Lessons from Abroad
Some countries have implemented innovative approaches to prevent undue influence. For example, in some Nordic countries, pharmaceutical companies are prohibited from direct-to-consumer advertising, which reduces their ability to create demand for specific drugs.
The Future of Pharmaceutical Regulation: Challenges and Opportunities
As we look to the future, what challenges and opportunities lie ahead in the realm of pharmaceutical regulation?
The Promise of Technology
Advancements in technology, such as artificial intelligence and blockchain, could potentially revolutionize drug approval processes and increase transparency in clinical trials.
The Challenge of Globalization
In an increasingly globalized world, regulatory agencies must grapple with the challenges of overseeing drug development and manufacturing that spans multiple countries and jurisdictions.
The Ethical Imperative: Balancing Innovation and Integrity
At the heart of this issue lies a fundamental ethical question: How do we balance the need for pharmaceutical innovation with the imperative to maintain integrity in the drug approval process?
The Cost of Integrity
Stringent regulations and oversight can be costly and time-consuming. Some argue that excessive regulation stifles innovation and delays potentially life-saving drugs from reaching the market.
The Price of Corruption
On the other hand, the cost of corruption in the pharmaceutical industry can be measured in human lives. Unsafe or ineffective drugs that make it to market due to undue influence can have devastating consequences.
The Role of Healthcare Professionals
Healthcare professionals play a crucial role in this ecosystem. They’re often caught in the middle, balancing their relationships with pharmaceutical companies, their duty to patients, and their ethical obligations.
Navigating Ethical Waters
Doctors and other healthcare professionals must navigate complex ethical waters when interacting with pharmaceutical companies. This includes deciding whether to accept speaking fees, participate in industry-sponsored research, or attend company-funded conferences.
The Importance of Continuing Education
Ongoing education about ethical guidelines and potential conflicts of interest is crucial for healthcare professionals. Many medical schools and professional organizations are now placing greater emphasis on these topics.
The Patient Perspective: Trust in the System
Ultimately, it’s the patients who have the most at stake in this issue. Their trust in the drug approval process and the healthcare system as a whole is paramount.
Informed Consumers
In today’s information age, patients have more access to information about drugs and their approval processes than ever before. This can be both empowering and overwhelming.
The Trust Deficit
Scandals and controversies in the pharmaceutical industry can erode public trust. Rebuilding and maintaining this trust is crucial for the effective functioning of the healthcare system.
Key Takeaways
As we wrap up our deep dive into this complex issue, let’s summarize the key points:
- Direct bribery of FDA officials is illegal and extremely risky for pharmaceutical companies.
- However, more subtle forms of influence, such as funding research and providing consulting fees, can raise ethical concerns.
- There have been instances of corruption in the past, leading to reforms and increased scrutiny.
- Safeguards exist, including conflict of interest regulations, transparency initiatives, and whistleblower protections.
- Public scrutiny and media oversight play crucial roles in maintaining integrity in the system.
- The challenge lies in balancing the need for pharmaceutical innovation with maintaining integrity in the drug approval process.
- Healthcare professionals and patients play important roles in navigating and shaping this complex landscape.
In conclusion, while the system isn’t perfect, there are significant safeguards in place to prevent outright bribery of the FDA. However, the influence of the pharmaceutical industry on drug regulation remains a complex and contentious issue that requires ongoing vigilance, transparency, and ethical consideration from all stakeholders involved.
FAQs
- Q: Can pharmaceutical companies directly pay FDA officials for drug approvals?
A: No, direct payments to FDA officials for drug approvals would be considered bribery and are illegal. Such actions would result in severe legal consequences for both the company and the individuals involved. - Q: How do pharmaceutical companies influence the FDA legally?
A: Pharmaceutical companies can influence the FDA through legal channels such as formal meetings during the drug development process, submission of clinical trial data, and responses to FDA queries. They may also engage in lobbying activities and fund research that supports their products. - Q: What is the “revolving door” between the FDA and pharmaceutical companies?
A: The “revolving door” refers to the practice of individuals moving between positions in the FDA and the pharmaceutical industry. While this can bring valuable expertise to both sides, it also raises concerns about potential conflicts of interest. - Q: Are there any safeguards to prevent undue influence on the FDA?
A: Yes, there are several safeguards in place, including strict conflict of interest regulations for FDA employees and advisory committee members, transparency initiatives like the Physician Payments Sunshine Act, and whistleblower protection laws. - Q: How can patients ensure they’re getting unbiased information about drugs?
A: Patients can seek information from multiple sources, including independent medical journals, consumer health organizations, and government health websites. They should also discuss any concerns with their healthcare providers and be aware of potential conflicts of interest in the information they receive.
Sources cited:
[1] https://www.science.org/content/article/hidden-conflicts-pharma-payments-fda-advisers-after-drug-approvals-spark-ethical
[5] https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/application-integrity-policy/fr-fda-091091-notice-56-fr-46191-fraud-untrue-statements-material-facts-bribery-and-illegal