The Drug Development Dilemma
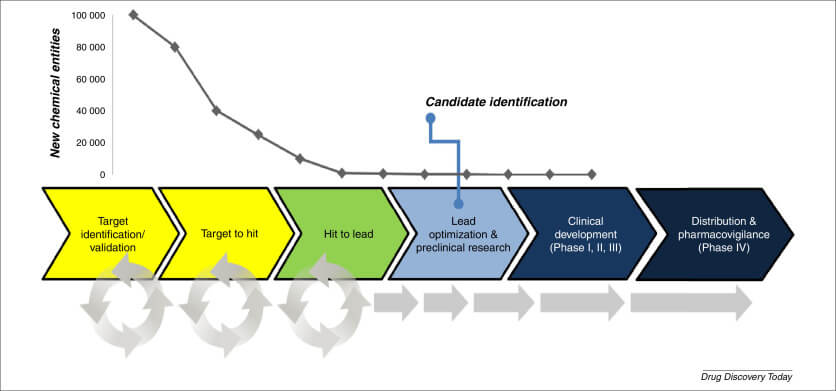
Picture this: You’re a scientist who’s just discovered a molecule with incredible potential to treat a devastating disease. You’re ecstatic, thinking you’ve hit the jackpot. But hold your horses! The road from lab to pharmacy shelf is long and treacherous. In fact, it’s estimated that only about 1 in 10,000 compounds make it through the entire drug development process. That’s a sobering statistic, isn’t it?
The Attrition Problem
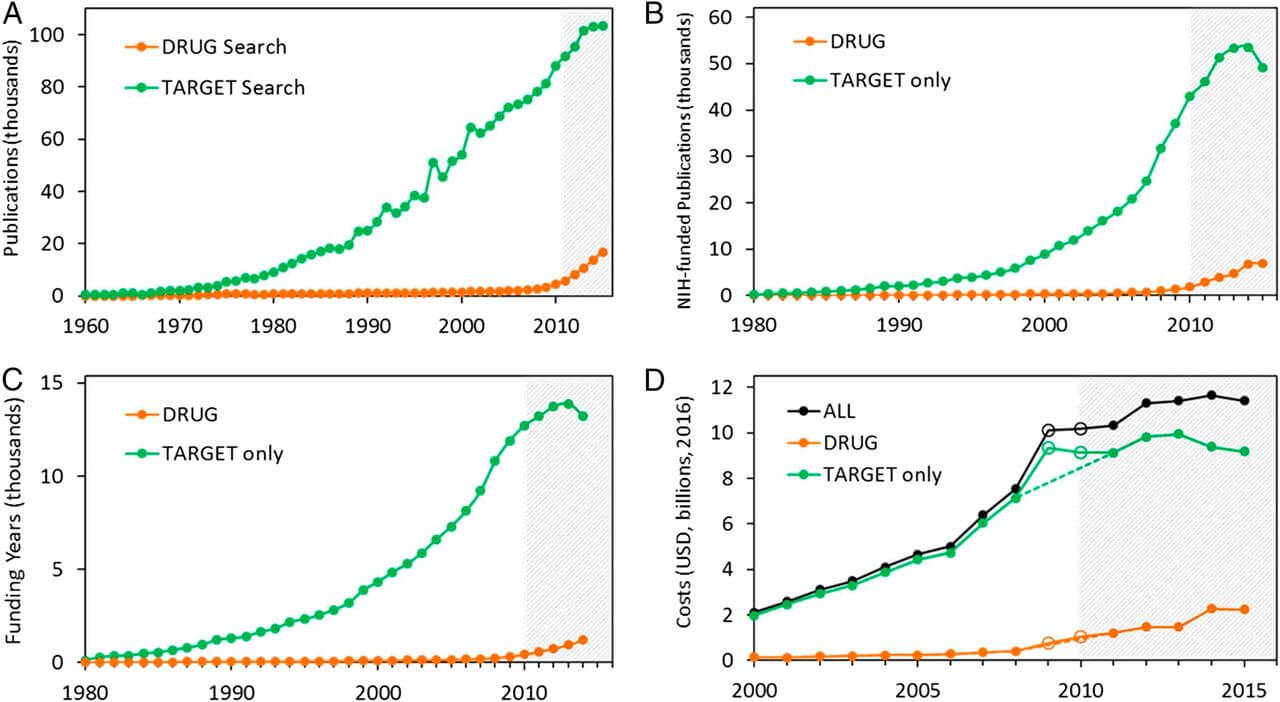
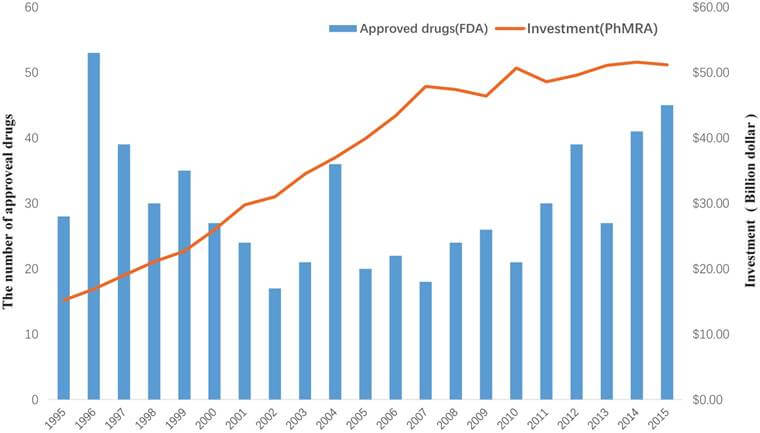
Attrition in drug development is like a leaky pipeline. At each stage of the process, promising candidates drop out for various reasons. Poor efficacy, safety concerns, and inadequate pharmacokinetics are just a few of the culprits. It’s not just a scientific setback; it’s a financial nightmare. The cost of bringing a single drug to market can exceed $2.6 billion. With stakes this high, reducing attrition isn’t just desirable – it’s essential.
Formulation: The Alchemist’s Art
What is Formulation?
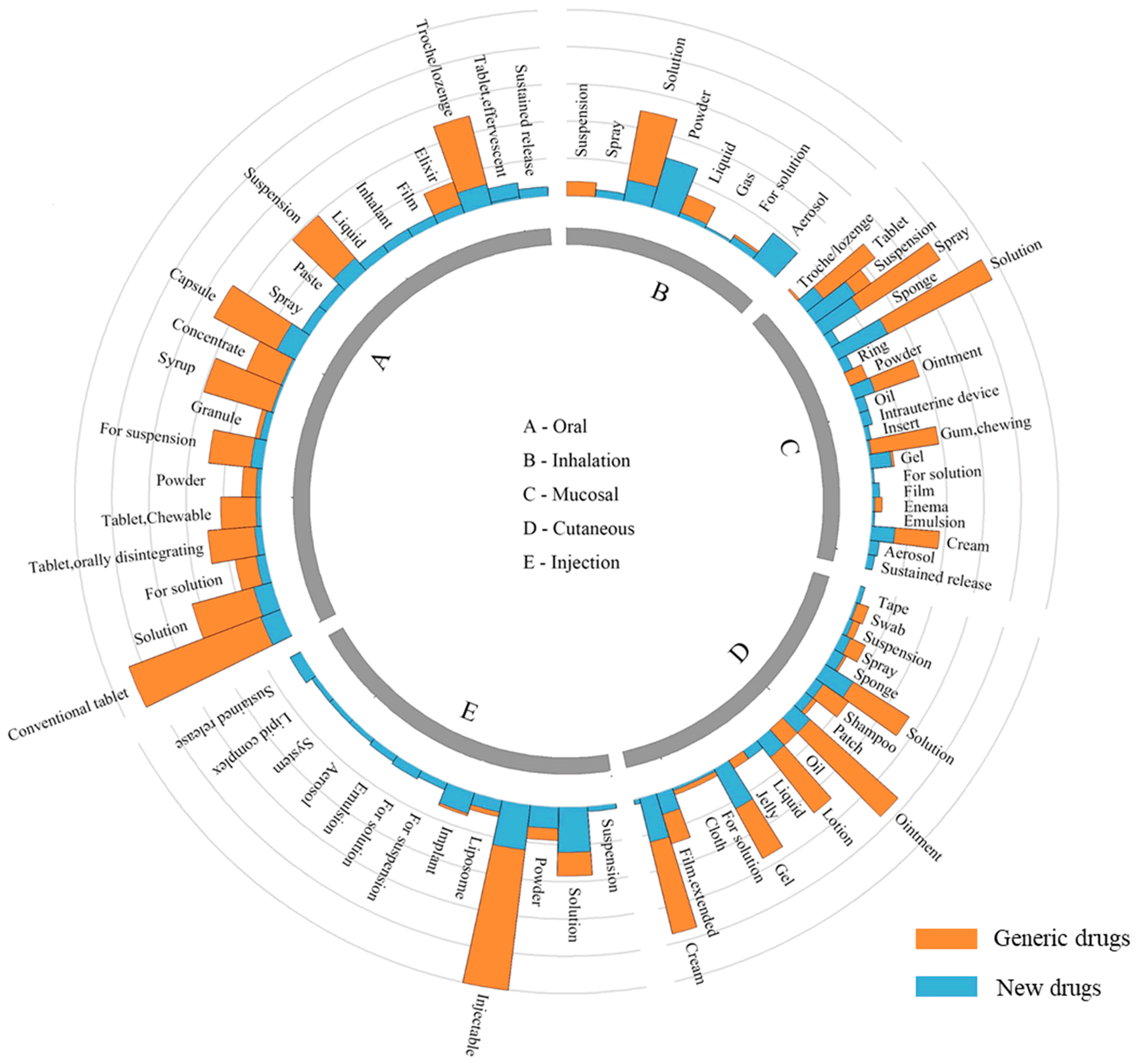
Formulation is the art and science of transforming a raw drug substance into a form that can be effectively delivered to the body. It’s like being a culinary wizard, but instead of creating delectable dishes, you’re crafting life-saving medicines.
The Power of Proper Formulation
Proper formulation can be the difference between a drug that works wonders and one that falls flat. It can enhance solubility, improve stability, and boost bioavailability. These aren’t just fancy scientific terms – they’re the keys to unlocking a drug’s full potential.
“Formulation is not just about making a drug palatable; it’s about maximizing its therapeutic potential while minimizing side effects. It’s the bridge between a promising molecule and a successful medicine.” – Dr. Sarah Johnson, Lead Formulation Scientist at PharmaTech Innovations
Innovative Formulation Techniques
Nanotechnology in Formulation
Nanotechnology is revolutionizing drug formulation. By shrinking particles to nanoscale, we can dramatically improve a drug’s solubility and absorption. Imagine turning a stubborn, insoluble compound into a superstar that readily enters the bloodstream. That’s the magic of nanoformulation.
Lipid-Based Formulations
Lipid-based formulations are like trojan horses for drugs. They can smuggle poorly soluble compounds past the body’s defenses, enhancing bioavailability. This approach has breathed new life into many compounds that were once considered “undruggable”.
Amorphous Solid Dispersions
Amorphous solid dispersions are a bit like mixing sugar into your coffee. By dispersing the drug in a polymer matrix, we can keep it in a high-energy state, improving solubility and absorption. It’s a game-changer for drugs that typically have poor oral bioavailability.
Drug Delivery: The Strategic Courier
The Importance of Drug Delivery
If formulation is about preparing the drug, drug delivery is about getting it to the right place at the right time. It’s like being a strategic courier in the body’s complex network of systems.
Targeted Drug Delivery
Targeted drug delivery is the sniper rifle of the pharmaceutical world. Instead of carpet-bombing the entire body with medication, it delivers the drug precisely where it’s needed. This approach can dramatically improve efficacy while reducing side effects.
Novel Drug Delivery Systems
Transdermal Patches
Remember when taking medicine always meant swallowing a pill? Transdermal patches have changed that narrative. They offer a steady, controlled release of medication through the skin, improving patient compliance and reducing dosing frequency.
Inhalation Devices
Inhalation devices are breathing new life into drug delivery (pun intended). They can deliver medication directly to the lungs, making them ideal for respiratory conditions. But their potential doesn’t stop there – they’re also being explored for systemic drug delivery.
Implantable Drug Delivery Systems
Implantable drug delivery systems are like having a personal, round-the-clock pharmacist in your body. They can provide long-term, controlled release of medication, which is particularly valuable for chronic conditions.
The Synergy of Formulation and Drug Delivery
A Dynamic Duo
Formulation and drug delivery are like peanut butter and jelly – good on their own, but truly magical when combined. By considering both aspects early in the drug development process, we can create more effective, patient-friendly treatments.
Case Studies: Success Stories
Case Study 1: Liposomal Doxorubicin
Doxorubicin is a powerful anticancer drug, but its use was limited by serious side effects. By encapsulating it in liposomes (a type of lipid-based formulation), researchers created a new formulation that reduced toxicity while maintaining efficacy. This innovative approach breathed new life into an established drug.
Case Study 2: Inhaled Insulin
The development of inhaled insulin showcases the power of innovative drug delivery. By formulating insulin for inhalation, researchers created a needle-free option for diabetics, potentially improving quality of life and treatment adherence.
Reducing Attrition: The Impact of Formulation and Drug Delivery
Early Integration in Drug Discovery
Integrating formulation and drug delivery considerations early in the drug discovery process can help identify and address potential issues before they become deal-breakers. It’s like having a GPS for drug development, helping navigate around potential roadblocks.
Rescuing “Failed” Drugs
Sometimes, a drug fails not because it’s ineffective, but because it can’t reach its target effectively. Advanced formulation and delivery techniques can sometimes rescue these “failed” drugs, giving them a second chance at success.
Improving Safety Profiles
By enabling more precise dosing and targeted delivery, formulation and drug delivery techniques can improve the safety profiles of many drugs. This can help reduce attrition due to safety concerns in later stages of development.
The Future of Formulation and Drug Delivery
Personalized Medicine
The future of formulation and drug delivery is personalized. Imagine treatments tailored not just to your condition, but to your specific genetic makeup, lifestyle, and preferences. We’re not there yet, but that’s the direction we’re heading.
3D Printing in Pharmaceuticals
3D printing is set to revolutionize drug formulation and delivery. It could enable on-demand production of personalized dosage forms, opening up new possibilities for tailored treatments.
AI and Machine Learning
Artificial intelligence and machine learning are becoming powerful tools in formulation and drug delivery. These technologies can help predict how a drug will behave in different formulations, potentially streamlining the development process.
Challenges and Considerations
Regulatory Hurdles
While innovative formulation and delivery techniques offer exciting possibilities, they also present regulatory challenges. Ensuring the safety and efficacy of these new approaches requires rigorous testing and validation.
Cost Considerations
Advanced formulation and delivery techniques can be expensive. Balancing the potential benefits against the increased costs is a crucial consideration in drug development.
Patient Acceptance
Even the most innovative delivery system won’t be effective if patients don’t accept it. Ensuring that new formulations and delivery methods are patient-friendly is crucial for their success.
Key Takeaways
- Formulation and drug delivery play crucial roles in reducing attrition during drug discovery and development.
- Early integration of formulation and delivery considerations can help identify and address potential issues before they become deal-breakers.
- Innovative techniques like nanotechnology, lipid-based formulations, and targeted delivery systems are revolutionizing drug development.
- The synergy between formulation and drug delivery can breathe new life into “failed” drugs and improve the safety profiles of existing ones.
- The future of formulation and drug delivery lies in personalized medicine, 3D printing, and AI-driven approaches.
- While challenges exist, the potential benefits of advanced formulation and delivery techniques in reducing attrition rates make them a vital area of focus in pharmaceutical research.
FAQs
- Q: How early in the drug discovery process should formulation and delivery be considered?
A: Ideally, formulation and delivery considerations should be integrated as early as the lead optimization stage. This early integration can help identify potential issues and guide the selection of candidates with the best chances of success. - Q: Can improved formulation and delivery techniques completely eliminate drug attrition?
A: While they can significantly reduce attrition rates, they can’t eliminate it entirely. Other factors, such as unexpected side effects or changes in the competitive landscape, can still lead to attrition. - Q: Are there any downsides to using advanced formulation and delivery techniques?
A: While these techniques offer many benefits, they can also increase complexity and cost in drug development. Additionally, novel formulations or delivery systems may face additional regulatory scrutiny. - Q: How does personalized medicine relate to formulation and drug delivery?
A: Personalized medicine aims to tailor treatments to individual patients. Advanced formulation and delivery techniques can enable more precise dosing and targeted delivery, supporting the goals of personalized medicine. - Q: What role does patient compliance play in formulation and drug delivery?
A: Patient compliance is a crucial consideration. Even the most effective drug won’t work if patients don’t take it as prescribed. Innovative formulations and delivery systems that improve ease of use or reduce dosing frequency can significantly enhance patient compliance.