Executive Summary
Generic drugs are indispensable to global healthcare systems, representing the backbone of affordable and accessible treatment. In the United States, for instance, generics account for an estimated 91% of all prescriptions filled, contributing to tens of billions of dollars in annual savings and over $2.44 trillion in savings over the past decade.1 Despite their critical role, the development and market entry of generic drugs are far from simple. It is not a mere replication process but a rigorous endeavor demanding stringent adherence to complex regulatory standards to ensure safety, efficacy, and quality. In today’s hyper-competitive global market, compliance is not merely a formality; it is a fundamental “survival skill” where any misstep can lead to severe consequences, including costly delays, application rejections, market withdrawals, and significant legal and reputational repercussions.5
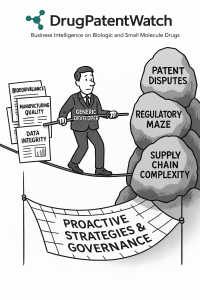
The generic drug industry confronts a multifaceted array of compliance challenges. These include the continuous adaptation to rapidly evolving regulatory landscapes, the intricate scientific demands of demonstrating bioequivalence, the complexities of maintaining manufacturing quality across global supply chains, the strategic navigation of intellectual property disputes, and the paramount need to ensure robust data integrity. Lessons gleaned from historical compliance failures consistently highlight the critical necessity for proactive strategies, the implementation of robust quality management systems, the judicious adoption of advanced technologies, and, perhaps most importantly, the cultivation of a deeply embedded organizational culture that prioritizes quality and integrity above all else.5
1. Introduction: The Imperative of Generic Drug Compliance
Defining Generic Drugs and Their Significance
Generic medicines are pharmaceutical products developed to be therapeutically equivalent to an already authorized “reference medicine,” often referred to as the innovator or brand-name drug. This equivalence mandates that the generic product contains the same active substance(s), is used at the same dose(s), and is intended to treat the same disease(s).10 While minor differences in inactive ingredients, name, appearance, and packaging are permissible, generic drugs must meet the identical high standards of quality and manufacturing as their brand-name counterparts.10 The development of a generic drug is fundamentally predicated on the expiration of exclusive rights and patent protection held by the innovator company.12 This mechanism is designed to foster market competition, leading to the availability of cost-effective alternatives that significantly enhance patient access and affordability, thereby contributing substantially to overall healthcare savings.1
The High Stakes of Compliance in a Competitive Global Market
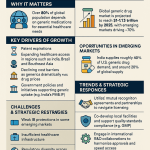
The global generic drugs market is a colossal and continuously expanding sector. Valued at an estimated USD 465.19 billion in 2023, it is projected to reach approximately USD 779.68 billion by 2033, demonstrating a robust Compound Annual Growth Rate (CAGR) of 5.3%.2 Within this hyper-competitive environment, stringent compliance with regulatory requirements is not merely a bureaucratic hurdle but a critical business imperative. Any deviation or misstep in the compliance process can trigger a cascade of severe repercussions. These include protracted and costly delays in market entry, outright rejection of marketing authorization applications, forced market withdrawals and product recalls, exposure to extensive class-action lawsuits from affected patients, and even the imposition of criminal charges.5 Such failures not only incur immense financial penalties but also severely erode public trust and can fundamentally jeopardize a company’s long-term viability and reputation.
A critical observation within the generic drug sector is what can be described as the Economic and Public Health Paradox of Generic Drugs. While generics are celebrated for their role in making healthcare affordable and accessible, accounting for a vast majority of prescriptions and generating substantial cost savings 2, the industry itself operates on exceptionally narrow profit margins.19 This intense price competition creates a relentless pressure on manufacturers to minimize costs. One common consequence is the strategic selection of lower-cost geographies for sourcing active pharmaceutical ingredients (APIs) and for manufacturing operations.19 This, in turn, contributes to the development of highly complex and geographically dispersed global supply chains.5 The inherent tension here is profound: the very economic model that delivers affordability to patients simultaneously creates significant financial constraints for manufacturers. If these financial pressures are not meticulously managed with robust compliance strategies and adequate investment in quality infrastructure, they can inadvertently lead to compromises in quality 24 and an increased propensity for compliance failures. Ultimately, such compromises undermine the very trust and access that generics are designed to provide. This dynamic illustrates a paradox where the economic success of the generic drug industry is intricately linked with significant compliance vulnerabilities, necessitating vigilant regulatory oversight and proactive internal quality measures to prevent cost-cutting from jeopardizing patient safety. The imperative to reduce healthcare costs through generics inadvertently creates an environment where manufacturers operate with minimal financial buffer, making investment in robust quality systems and compliance infrastructure a significant challenge, especially for smaller companies.7
2. Global Regulatory Frameworks for Generic Drugs
2.1. The FDA’s Abbreviated New Drug Application (ANDA) Pathway
In the United States, the primary pathway for generic drug approval is through the Abbreviated New Drug Application (ANDA) process, overseen by the Food and Drug Administration (FDA). This pathway offers a streamlined route, significantly reducing the development burden on manufacturers by allowing them to rely on the established safety and efficacy data of an already approved Reference Listed Drug (RLD), thereby obviating the need for duplicative preclinical and Phase III clinical trials.12
To obtain ANDA approval, a generic drug must demonstrate therapeutic equivalence to its RLD. This encompasses matching the RLD in several critical aspects: active ingredients, conditions of use, method of administration, dosage form and strength, and labeling (with only minor permissible differences). Crucially, the generic product must also demonstrate bioavailability and bioequivalence to the RLD, ensuring it delivers the same therapeutic effect in the body.11 Furthermore, compliance with Current Good Manufacturing Practices (cGMP) throughout the manufacturing process is a non-negotiable requirement.11
The ANDA submission and review process is systematic. It begins with comprehensive pre-ANDA preparation, which involves meticulous analysis of the RLD’s chemical composition, formulation, labeling, and regulatory history. This phase also includes conducting preliminary bioequivalence studies and ensuring adherence to cGMP standards, along with a thorough understanding of FDA guidance documents.14 Once compiled, the complete ANDA dossier—including detailed drug formulation, manufacturing processes, quality control measures, labeling information, bioequivalence study results, and stability testing reports—is submitted electronically via the FDA Electronic Submissions Gateway (ESG).14 Upon receipt, the FDA initiates a multi-phase review to assess the submitted bioequivalence and safety data, verify labeling compliance with the RLD, and conduct manufacturing site inspections to ensure quality assurance.14 While the review process typically spans around 30 months, applications for priority generics (e.g., those addressing drug shortages or unmet medical needs) may be expedited.14 During the review, the FDA may issue Information Requests (IRs) or Discipline Review Letters (DRLs) to address deficiencies. If these issues remain unresolved, the agency may issue a Complete Response Letter (CRL), indicating that the application cannot be approved in its current form.27 Final approval of an ANDA is contingent upon all reviewing disciplines deeming the submission adequate, all manufacturing facilities being deemed adequate, and the absence of any legal barriers, such as unexpired patents or exclusivities.27
2.2. The EMA’s Centralised and National Procedures for Generic Marketing Authorisation
In Europe, the European Medicines Agency (EMA) plays a central role in overseeing the approval processes for generic drugs, ensuring they meet the same rigorous standards as their brand-name counterparts.12 A marketing authorization application for a generic medicine can generally only be submitted once the period of data exclusivity of the reference medicine has expired, which typically occurs 10 or 11 years from the date of the reference product’s initial authorization.10
The eligibility for the EMA’s Centralised procedure for generic and hybrid medicinal products can be granted in two primary ways. First, generic or hybrid medicinal products of centrally authorized products automatically gain access to the Centralised procedure under Article 3(3) of Regulation (EC) No 726/2004. Applicants are advised to notify the EMA of their intention to submit 6-18 months in advance.29 Second, for generics of nationally authorized, Mutual Recognition Procedure (MRP), or Decentralised Procedure (DCP) products, consideration under the Centralised procedure can be requested if the applicant demonstrates that the medicinal product constitutes a “significant therapeutic, scientific or technical innovation” or that its Union-level authorization is in the “interest of patients at Union level”.29
The EMA defines a generic medicinal product as one that possesses the same qualitative and quantitative composition in active substance(s) as the reference product, the same pharmaceutical form, and has demonstrated bioequivalence with the reference medicinal product through appropriate bioavailability studies.29 The application process involves the EMA providing guidance to developers to ensure compliance with legal and regulatory requirements, thereby minimizing unnecessary delays.30 During the assessment phase, the EMA evaluates whether the benefits of the medicine outweigh its risks. For generic applications, typically only one rapporteur (a committee member from a different country) is appointed to lead the assessment.30 Following its assessment, the EMA issues a recommendation to the European Commission, which then takes the final, legally binding decision on whether the medicine can be marketed in the EU. This decision is typically issued within 67 days of receiving the EMA’s recommendation.30
A significant aspect for manufacturers is understanding the Strategic Interplay of Regulatory Pathways and Market Entry Timelines. Both the FDA’s ANDA and the EMA’s Centralised pathways are designed to streamline generic drug approval by allowing reliance on the established safety and efficacy data of the reference product.10 However, their specific procedural timelines and exclusivity rules create distinct strategic considerations for manufacturers. The FDA’s ANDA review process, while aiming for efficiency, typically extends to around 30 months for approval.14 In contrast, the EMA’s final decision by the European Commission is issued relatively quickly (within 67 days)
after the EMA’s recommendation.30 The “race to file” in the U.S. generic market is heavily influenced by the incentive of a 180-day market exclusivity period granted to the first generic company to file an ANDA with a Paragraph IV certification and prevail in a patent infringement lawsuit.20 Conversely, in Europe, the strict patent and data exclusivity periods (typically 10-11 years) dictate the earliest possible time an application can even be submitted.10 This means that while both agencies aim to expedite generic entry, the actual market entry timelines are profoundly influenced by the complex interplay of regulatory review periods, the nuances of patent litigation, and the specific exclusivity provisions in each jurisdiction. Manufacturers must therefore meticulously plan their market entry strategies, including their research and development investments and potential legal challenges, years in advance. Competitive intelligence becomes paramount for accurately forecasting “patent cliffs” and identifying optimal market opportunities.20 This complex environment underscores that the “streamlined” nature of generic approval pathways is relative; achieving market access requires sophisticated legal and strategic foresight.
2.3. Harmonization Efforts and International Collaboration
Recognizing the global nature of pharmaceutical development and supply, regulatory agencies worldwide, including the FDA and EMA, actively engage in harmonization efforts and international collaboration. They participate in key international forums such as the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH), which aims to establish unified standards and facilitate the mutual acceptance of clinical data across different jurisdictions.33
A notable example of this collaboration is the FDA’s Generic Drug Cluster, which serves as an essential forum for international regulatory dialogue. This initiative brings together agencies from various countries to share knowledge, address common challenges, and align on best practices for the oversight of generic drugs.35 These discussions are instrumental in clarifying technical standards, such as those for in-vitro release testing (IVRT) and in-vivo pharmacokinetic (PK) evaluations, particularly for complex generic products like topical formulations or protein-bound paclitaxel.35 Furthermore, Mutual Recognition Agreements (MRAs) between the FDA and EMA and several other countries play a crucial role in streamlining the regulatory process. These agreements reduce the regulatory burden on pharmaceutical companies by allowing agencies to rely on each other’s Good Manufacturing Practice (GMP) inspections, waive redundant batch testing, and facilitate the exchange of inspection-related information.34
However, a critical observation regarding these efforts reveals what can be termed the Double-Edged Sword of Global Harmonization. While initiatives like ICH, the Generic Drug Cluster, and MRAs are undeniably crucial for fostering efficiency and promoting consistent global thinking and approaches in drug regulation 34, they are not a complete solution. Despite these concerted efforts, persistent “differences in requirements between jurisdictions can impede submissions on an international level”.37 For instance, the EMA’s decentralized inspection process, while coordinated across member states, can still result in variations in inspection practices among individual national competent authorities.34 This becomes particularly salient given the heavy reliance of the global generic drug supply chain on active pharmaceutical ingredients (APIs) sourced from diverse countries.23 While the FDA does oversee foreign suppliers, the sheer volume and number of manufacturing facilities worldwide make it practically impossible for any single agency to comprehensively police all global facilities.23 This means that manufacturers cannot solely rely on a “one-size-fits-all” compliance strategy. Instead, they must maintain deep local regulatory intelligence and adaptability, as even subtle inconsistencies in regulatory interpretation or enforcement can lead to significant delays or non-compliance. The aspiration for global convergence is therefore a continuous journey, not a fixed destination, requiring ongoing vigilance and flexible compliance strategies from generic drug manufacturers.
3. Core Pillars of Generic Drug Compliance
3.1. Good Manufacturing Practices (GMP/cGMP)
Good Manufacturing Practices (GMP), often referred to as Current Good Manufacturing Practices (cGMP) to emphasize the necessity of employing up-to-date systems and technologies, represent a foundational set of guidelines and regulations established by regulatory agencies such as the FDA and EMA.39 These practices are designed to ensure the consistent production of safe, effective, and high-quality pharmaceuticals. At its core, GMP is paramount for patient safety, serving as a critical safeguard against contamination, inconsistencies, and defects in drug formulations.39 The underlying philosophy is that quality must be “built into” products through robust design and manufacturing processes, rather than merely “tested into” them at the end.43
Key components and requirements for GMP compliance are extensive and cover virtually every aspect of the manufacturing process. This includes the implementation of robust Quality Management Systems (QMS) to oversee personnel training, facility management, comprehensive documentation, and stringent quality control.39 Manufacturing facilities and equipment must be designed, constructed, and maintained to meet rigorous quality and safety standards, encompassing considerations for cleanliness, environmental controls (such as temperature and humidity), and proper calibration and maintenance of all equipment.39 Adequate training and qualification of all personnel involved in manufacturing, testing, and quality assurance are essential to ensure competency and adherence to GMP requirements.39 Comprehensive documentation and meticulous record-keeping of manufacturing processes, quality control tests, batch records, and stability testing are mandated to ensure traceability and accountability.12 This includes written procedures for production and process control.41 Rigorous quality control testing of raw materials, intermediate products, and finished products is required to verify their identity, strength, purity, and quality.39 Furthermore, process validation studies are crucial to ensure the consistency, reliability, and reproducibility of product quality.39 Finally, packaging and labeling must comply with regulatory requirements and accurately convey product information to healthcare professionals and patients.39
Regulatory frameworks for GMP are well-defined by leading agencies. In the United States, the FDA enforces cGMP through 21 CFR Parts 210 (General Current Good Manufacturing Practice in Manufacturing, Processing, Packing, or Holding of Drugs) and 211 (Current Good Manufacturing Practice for Finished Pharmaceuticals). These regulations cover minimum requirements across personnel, facilities, equipment, production processes, laboratory controls, stability testing, and labeling.41 In Europe, the EMA coordinates inspections to verify GMP compliance and plays a pivotal role in harmonizing GMP activities across the European Union.36 The legal instruments underpinning EU GMP include Regulation No. 1252/2014 and Directive 2001/83/EC.36 The EU GMP guide is further elaborated through 4 parts and 21 Annexes, providing detailed guidance on specific topics such as sterile manufacturing (Annex 1) and computerized systems (Annex 11).44
3.2. Good Laboratory Practices (GLP)
Good Laboratory Practices (GLP) constitute a set of principles specifically designed to ensure the quality and integrity of non-clinical laboratory studies, particularly those involving safety testing for pharmaceuticals, pesticides, and chemicals.45 Adherence to GLP is critical because it ensures that the data generated from these studies are reliable, reproducible, and accurate, forming a trustworthy basis for regulatory decisions regarding the safety and efficacy of new drugs.45
The core principles of GLP encompass several key areas. A well-defined organizational structure and clear responsibilities for personnel are fundamental.45 All equipment, from scientific instruments to support equipment, must be properly calibrated, maintained, and tested regularly.45 Test systems (e.g., animals, cell cultures) must be appropriately characterized, and test and reference substances require proper characterization, documentation of identity, purity, stability, and storage conditions, along with a clear chain of custody.45 Detailed, written Standard Operating Procedures (SOPs) are a cornerstone, ensuring consistent methods are followed by all personnel.45 Accurate and reliable data collection and reporting are paramount, with all data recorded promptly, accurately, and legibly, and original data securely retained.45 Finally, comprehensive archiving of all records, samples, and specimens for specified periods is mandated for future review or reanalysis.45
The regulatory requirement for GLP emerged in response to observed deficiencies. The FDA issued its GLP regulations in 1978 due to a perceived lack of quality and scientific integrity in nonclinical toxicology studies.48 Generally, GLP compliance is required for most nonclinical studies that support regulatory submissions, such as Investigational New Drug (IND) applications, though some early exploratory studies (e.g., for preliminary absorption, distribution, metabolism, and excretion (ADME) properties) may be exempt.48 A vital aspect of GLP is the requirement for an independent Quality Assurance Unit (QAU). The QAU’s role is to monitor study compliance with GLP principles, conduct audits (reviewing source data, quality control steps, and reports), and assure management that all facilities, equipment, personnel, methods, practices, records, and controls conform to regulations. This independence is crucial for ensuring the validity and integrity of nonclinical safety data.46
3.3. Good Clinical Practices (GCP)
Good Clinical Practice (GCP) is an internationally recognized ethical and scientific quality standard for the design, conduct, recording, and reporting of clinical trials that involve the participation of human subjects.33 Adherence to GCP provides public assurance that the rights, safety, and well-being of trial participants are protected, consistent with the ethical principles originating from the Declaration of Helsinki. It also ensures the credibility and accuracy of the clinical trial data generated.33
While generic drug approval pathways (ANDA in the US, Centralised procedure in Europe) typically rely on the established safety and efficacy of the reference listed drug, bioequivalence studies are a mandatory component of generic drug development and involve human participants. Consequently, these studies must strictly adhere to GCP principles.12
Key requirements under GCP include the timely review of safety information as it becomes available, a careful weighing of foreseeable risks and inconveniences against the anticipated benefits for individual participants and society, and appropriate participant selection. While some early-phase trials or bioequivalence studies may not require a highly heterogeneous population, the overall principle is to select participants representative of the intended patient population.49 A qualified physician or other appropriate healthcare professional must have overall responsibility for the trial-related medical care and decisions made on behalf of participants.49 Furthermore, meticulous documentation of all operations, including controls, product administration to subjects, and the identity of personnel performing tasks, is essential. Adherence to the study protocol is fundamental, and any significant changes must be submitted as amendments to the competent regulatory authority and ethics committee.50 Deviations from inclusion/exclusion criteria are generally not permitted unless necessary to eliminate immediate hazards to subjects, emphasizing the scientific and ethical value of the protocol.50
3.4. Bioequivalence (BE) and Bioavailability Studies
Bioequivalence (BE) and bioavailability studies are the cornerstone of generic drug approval, serving as the scientific proof that a generic product performs comparably to its brand-name counterpart in the human body. Bioequivalence is precisely defined as the absence of a significant difference in the rate and extent of absorption of the active ingredient when administered at the same molar dose under similar conditions.51 These studies quantify key pharmacokinetic (PK) parameters, primarily the maximum concentration (Cmax) of the drug in the bloodstream, the area under the curve (AUC) representing total drug exposure over time, and the time to reach peak concentration (Tmax).12
The widely accepted regulatory standard for establishing bioequivalence is the “80-125% Rule.” This rule dictates that the 90% confidence interval for the ratio of the geometric means of Cmax and AUC for the generic (test) product versus the reference product must fall within the range of 80% to 125%.12 Bioequivalence studies typically employ crossover designs in healthy volunteers, where each participant receives both the generic and reference product at different times, minimizing inter-subject variability. The FDA generally recommends specific study designs, including two-period, two-sequence, two-treatment, single-dose crossover studies, parallel designs, or partial/fully replicated crossover designs for drugs with high variability.12 The test product used in these studies must come from a batch that accurately represents the final marketed product, typically at least 1/10th of the full production scale or a minimum of 100,000 units.51
While the principles of bioequivalence are clear, significant complexities arise, particularly for “complex generics.” Unlike simple oral tablets, products such as injectables, inhalers, topical creams, nanomedicines, or modified-release formulations introduce “layers of difficulty” due to their intricate delivery systems or unique formulations that often defy standard BE testing methodologies.5 For these products, traditional bioequivalence and bioavailability studies may not be entirely adequate, often requiring additional demonstrations of local effects or addressing differences in device design, which can be protected by innovator intellectual property.17
A critical observation regarding bioequivalence is what can be termed the Nuance of “Sameness” in Bioequivalence and its Regulatory Interpretation. Generic drugs are mandated to be “the same” as brand-name drugs in their active ingredient, strength, dosage form, and route of administration, and they must demonstrate bioequivalence.11 However, as highlighted by expert observations, the FDA’s 80-125% acceptance range for Cmax and AUC, while a statistical standard, can still allow for a “potential outside range of 45 percent among generics” when patients are switched from one generic manufacturer’s product to another.52 Furthermore, relying solely on peak drug concentration (Cmax) as a proxy for the rate of absorption might overlook crucial differences in the overall drug concentration-time curve, particularly for complex or time-release drugs.52 Inactive ingredients, or excipients, are permitted to differ between generic and brand-name products, provided the FDA receives evidence that these differences do not affect the generic’s performance, safety, or effectiveness.11 Nevertheless, these “invisible” equivalence challenges, such as using different salts or excipients, necessitate extensive reverse-engineering, often termed “de-formulation,” to meticulously replicate the RLD’s performance without access to its proprietary formulation details.20
This means that the regulatory definition of “sameness” for generics, particularly concerning bioequivalence, is a sophisticated statistical and scientific construct aimed at ensuring therapeutic equivalence. However, the permissible variability within this definition, combined with differences in inactive ingredients or formulation, can lead to subtle but potentially clinically significant differences for certain sensitive patient populations or for complex drug products.37 This reality underscores the ongoing need for careful patient counseling by healthcare professionals when transitioning from brand-name to generic medications, or between different generic versions.53 It also implies that while the regulatory framework is robust, the practical manifestation of “equivalence” across a diverse patient population can be more complex than statistical averages suggest, requiring continuous post-market surveillance.
3.5. Data Integrity (DI)
Data integrity is an absolutely critical element for ensuring product quality and compliance throughout the pharmaceutical industry. It encompasses the accuracy, dependability, and security of data across its entire lifecycle, from initial collection to long-term storage.54 Regulatory bodies, including the FDA and EMA, explicitly expect all data submitted by manufacturers to obtain market approval to be both reliable and accurate.54 Data integrity serves as the fundamental basis for all manufacturing decisions, safety procedures, and regulatory clearances.55
The FDA’s ALCOA guidelines provide a robust framework for guiding businesses in preserving accurate and dependable data. These principles dictate that data must be:
- Attributable: Clearly indicating who performed an action and when.54
- Legible: Coherent, clear, and easy to understand.54
- Contemporaneous: Recorded in real-time at the moment an action is taken.54
- Original: Maintained in its original form, with copies properly credited.54
- Accurate: Reflecting actual circumstances and events, validated, and only altered by authorized individuals.54
Beyond these core ALCOA principles, the concept of data integrity has evolved to include additional criteria, often referred to as ALCOA++, which emphasizes that data should also be Complete, Consistent, Enduring, and Available.54 This comprehensive approach to data integrity is crucial across all stages of the drug lifecycle, including non-clinical laboratory studies 45, clinical trials 33, manufacturing records 44, and all aspects of regulatory submissions.5
A profound observation in the pharmaceutical landscape is the role of Data Integrity as the Unseen Foundation of Trust and Compliance. Data integrity is not merely a technical requirement; it is the bedrock upon which regulatory trust and public health assurance are built. Despite its critical importance, data integrity lapses are a “hot topic” frequently cited in FDA Warning Letters 56 and prominently highlighted in EMA non-compliance reports.57 Common issues include a lack of proper access control to IT systems, the use of shared accounts, inadequate controls to prevent the deletion of raw data, insufficient audit trail review, unvalidated or unprotected IT systems, and even outright falsification of data.56
The consequences of data integrity failures are severe. Case studies, such as that of Ranbaxy, starkly demonstrate how falsified data and a pervasive lack of quality control can lead to contaminated and substandard medications entering the market, resulting in massive financial penalties (e.g., a $500 million fine for Ranbaxy) and a severe loss of credibility.6 Similarly, the EMA’s decision to suspend approximately 100 generic drugs due to “flawed” bioequivalence studies conducted by a contract research organization (CRO) 59 directly points to fundamental problems with the integrity or methodology of the underlying data. This illustrates that data integrity failures, whether accidental (e.g., poor record-keeping, reliance on outdated systems) or intentional (e.g., deliberate falsification), have a cascading effect. They undermine the validity of all subsequent analyses, compromise the integrity of regulatory submissions, and ultimately jeopardize the safety and efficacy claims of the drug product. The persistent occurrence of data integrity issues in regulatory enforcement actions indicates a systemic vulnerability within the industry. This vulnerability is often exacerbated by a lack of robust digital controls, insufficient personnel training, and a corporate culture that may inadvertently prioritize expediency or cost-cutting over unwavering integrity.5 Therefore, ensuring data integrity requires not only comprehensive technological solutions and rigorous audit trails but, most importantly, a strong ethical culture throughout the organization that unequivocally prioritizes integrity at every stage of the drug lifecycle.
4. Key Compliance Challenges in Generic Drug Development
4.1. Navigating Evolving Regulatory Standards
The regulatory environment governing pharmaceutical development is characterized by constant evolution. Frequent changes to guidelines and standards issued by agencies like the FDA pose a significant and continuous challenge for generic drug companies.7 This dynamic landscape necessitates continuous investment in training and education for development and manufacturing teams to keep pace with the latest requirements.8 Furthermore, new and often complex requirements continue to emerge, particularly for specialized drug types such as complex generics, compelling regulatory agencies to continuously adapt their frameworks while simultaneously ensuring their robustness and effectiveness.35
This continuous evolution highlights what can be termed the Regulatory Treadmill: Keeping Pace with Perpetual Evolution. The pharmaceutical regulatory landscape is not static; it is a dynamic system that constantly responds to new scientific advancements, emerging public health needs, and critical lessons learned from past failures. This creates a perpetual “regulatory treadmill” for manufacturers, where continuous investment in regulatory intelligence gathering, technological upgrades, and workforce training is not a competitive advantage but a fundamental requirement for operational survival. Failure to keep pace with these evolving standards inevitably leads to non-compliance, resulting in costly delays, application rejections, and significant legal and financial consequences.61 The very term “Current” in cGMP (Current Good Manufacturing Practices) explicitly implies that manufacturers must utilize “up-to-date systems and technologies” to comply with regulations.40 This means that what was considered compliant yesterday may no longer meet regulatory expectations tomorrow, demanding a proactive and agile compliance strategy rather than a reactive one.
4.2. Ensuring Robust Bioequivalence Data
Demonstrating bioequivalence (BE) is a “defining moment” and often a “major hurdle” for generic drug regulatory approval.37 It is frequently described as navigating a “scientific tightrope” where precision is absolutely non-negotiable.5 Despite established statistical criteria for BE, significant challenges persist in generating and interpreting robust data.
One of the primary challenges lies in the study design and execution. A 2023 study revealed that a substantial 20% of Abbreviated New Drug Application (ANDA) rejections stemmed directly from inadequate bioequivalence data.5 Even a single miscalculation or oversight in a pivotal study, such as failing to account for food effects, can lead to months of costly rework or necessitate a complete restart of the study.5 The complexities are compounded for
complex generics, which include products like injectables, inhalers, and topical formulations. These often involve intricate delivery systems or unique formulations that defy standard BE testing methodologies, posing “layers of difficulty”.5 Proving therapeutic equivalence becomes particularly challenging when the branded drug utilizes a proprietary device or requires demonstration of local effects rather than systemic absorption.5 Furthermore, issues such as variable absorption rates and differing effects of formulations, especially for modified-release products or drugs with a narrow therapeutic index, add to the scientific complexity of BE studies.37 A critical vulnerability also arises from reliance on external partners; the European Medicines Agency (EMA) notably suspended approximately 100 generic medicines that had come to market based on “flawed” bioequivalence studies conducted by an Indian Contract Research Organization (CRO), Synchron Research Services. This incident underscores the significant risk associated with insufficient oversight of third-party data generation.25
These challenges collectively reveal what can be described as the Hidden Vulnerability in Bioequivalence: Beyond the Numbers. While bioequivalence studies are central to generic approval and are governed by specific statistical criteria like the 80-125% rule for Cmax and AUC 12, the challenge extends far beyond merely hitting these numerical targets. It encompasses the fundamental scientific rigor of the study design, including anticipating and accounting for all relevant variables, such as food effects.5 It also critically involves the absolute integrity of data generation, whether conducted in-house or through external CROs. Furthermore, a nuanced interpretation of pharmacokinetic profiles is essential, especially for non-traditional dosage forms where the relationship between systemic exposure and clinical effect might be complex.17 A “bioequivalence blunder” 5 can lead to profound delays and significant financial costs, emphasizing that a purely numerical, checklist-based approach to compliance is insufficient. The true vulnerability lies not just in failing to meet the statistical criteria, but in the underlying scientific and operational practices that generate those numbers, and the potential for these practices to be compromised or misinterpreted.
4.3. Maintaining Manufacturing Quality and cGMP Adherence
Manufacturing quality issues represent a persistent and significant challenge within the generic drug industry, frequently identified as a leading cause of drug shortages, particularly for older generic medications.24 These issues often stem from the use of outdated manufacturing technologies and a lack of mature quality management practices.24
Common violations observed during regulatory inspections are diverse and often indicative of systemic problems. These include pervasive contamination and poor aseptic practices, with repeated observations of inadequate environmental monitoring (e.g., mold growth, liquid dripping from ceilings in stability chambers) and significant cross-contamination risks, especially when shared equipment is used for potent drug products.57 Manufacturers frequently demonstrate
inadequate investigations into Out-of-Specification (OOS) results, failing to thoroughly determine the root cause of repeated dissolution failures or other quality deviations, and sometimes proposing corrective and preventive actions (CAPA) without sufficient validation.63 In some cases, failed drug products were not rejected, indicating a breakdown in quality control.58
Inadequate facility and equipment maintenance are also common FDA observations, encompassing issues like insufficient cleaning and sanitization, crumbling insulation, peeling surfaces, and uncleaned equipment in critical clean areas.57 Furthermore, a lack of proper
process validation for manufacturing steps, including HVAC systems, filtration, and lyophilization, can lead to significant quality risks.57 Deficiencies in
raw material and Active Pharmaceutical Ingredient (API) control are also frequently cited, ranging from the falsification of API sources (e.g., repackaging non-GMP API as in-house) to the use of unapproved API sites and a failure to adequately test incoming raw materials for identity, strength, purity, and quality.57
Regulatory bodies respond to these violations with various enforcement actions. The FDA issues Form 483 observations, which detail inspectional findings, followed by Warning Letters for significant violations.56 These can lead to severe consequences, including import bans on products from non-compliant facilities.66 Similarly, the EMA issues non-compliance reports, which can result in the suspension or revocation of manufacturing authorizations.34
These persistent issues underscore what can be understood as the Systemic Nature of Manufacturing Quality Failures. Manufacturing quality failures are rarely isolated incidents; instead, they are typically symptoms of deeper, systemic deficiencies within a company’s overall Quality Management System (QMS) and operational culture. These underlying issues often include inadequate investment in manufacturing infrastructure and advanced technologies 24, insufficient personnel training, a lack of robust root cause analysis for deviations, and a fundamental failure to integrate quality principles throughout the entire manufacturing process, rather than treating quality control as a final checkpoint.7 The inherent complexities of the global supply chain further exacerbate these challenges, as comprehensive oversight of numerous foreign facilities becomes increasingly difficult for individual regulatory agencies.23 The “Cost of Cutting Corners” 5 serves as a stark lesson: short-term savings achieved by compromising quality inevitably lead to severe long-term repercussions, including significant financial penalties and reputational damage.6 Therefore, preventing recurring violations and safeguarding public health requires a robust, proactive QMS, unwavering leadership commitment to quality, and thorough, unbiased root cause analysis for every deviation.
4.4. Managing Intellectual Property Disputes
The foundation of generic drug development rests upon the expiration of innovator patents, which opens the door for competition.12 However, the landscape of intellectual property (IP) is often complex, and it is “not always clear whether the patents covering a drug are valid or applicable to a potential generic version,” leading to frequent and costly legal disputes.70
The Hatch-Waxman Act of 1984 (officially the Drug Price Competition and Patent Term Restoration Act) was enacted to balance two competing policy interests: incentivizing pioneering drug development and facilitating the efficient market entry of lower-cost generic copies.31 This act created the abbreviated regulatory pathway (ANDA) for generics, allowing them to rely on the innovator’s safety and efficacy data by demonstrating bioequivalence.31
A key mechanism within Hatch-Waxman involves patent certifications and litigation. When a generic manufacturer files an ANDA, it must make one of four certifications for each patent listed by the brand-name drug manufacturer in the FDA’s Orange Book.70 A Paragraph IV (PIV) certification, which states that the patent is either invalid or not infringed by the generic product, is particularly significant.20 If a PIV certification is made, the generic manufacturer must notify the patent holder, who then has 45 days to initiate a patent infringement lawsuit against the generic applicant. Such a lawsuit triggers an automatic 30-month stay on the FDA’s final approval of the generic application, allowing time for the patent dispute to be litigated before the generic drug can enter the market.20 A powerful economic incentive exists for generic companies: the “first generic company to file an ANDA with a Paragraph IV certification and prevail” in the ensuing patent infringement lawsuit is granted a 180-day period of market exclusivity, during which it is the sole generic version allowed on the market.20 This exclusivity fuels an “intense ‘race to file'” among generic manufacturers.20
Despite these mechanisms, significant challenges arise. Innovator companies often employ “evergreening” strategies, applying for additional patents on minor modifications such as new formulations, delivery methods, or combinations, to extend their market exclusivity beyond the original patent term.13 This practice contributes to the formation of “patent thickets”—portfolios of numerous, overlapping patents on the same pharmaceutical product—which act as formidable strategic barriers. These thickets deter generic competition due to the high risk of infringement and the prohibitive costs associated with patent litigation.20 Furthermore, litigation can sometimes lead to strategic settlements, including controversial “pay-for-delay” or “reverse payment” agreements, where the innovator compensates the generic manufacturer to delay its market entry.20 For complex generics delivered via devices (e.g., inhalers, auto-injectors), an additional layer of complexity exists, as the branded drug maker may still hold intellectual property rights on certain features of the device, complicating generic approval even if the drug itself is off-patent.17
These dynamics highlight what can be termed the Dual Nature of IP in Generic Drug Development: Incentive and Barrier. Intellectual property rights, while undeniably essential for incentivizing pharmaceutical innovation and enabling companies to recoup substantial research and development costs 71, paradoxically serve as a formidable and often strategically manipulated barrier to generic market entry. The legal strategies employed by innovator companies, such as the creation of patent thickets or engagement in “pay-for-delay” settlements, can effectively extend market exclusivity beyond the initial patent term, thereby delaying the availability of more affordable generics and impacting drug competition.16 This complex environment necessitates that generic manufacturers invest heavily not only in scientific and manufacturing capabilities but also in sophisticated legal and competitive intelligence strategies. This includes conducting thorough Freedom-to-Operate (FTO) analyses to identify potential patent barriers and devise “design-around” strategies, as well as engaging in strategic litigation when appropriate.20 The “artificial” act of patent infringement triggered by an ANDA filing 70 starkly underscores the highly litigious nature of this phase of generic drug development.
4.5. Oversight of Complex Global Supply Chains
The supply of generic drugs, particularly in the United States, is heavily reliant on a complex and globalized supply chain. Over 70% of active pharmaceutical ingredients (APIs) are sourced internationally, originating from hundreds of facilities across dozens of countries.5 This global dependency introduces numerous compliance challenges and vulnerabilities.
One of the most significant challenges is the vulnerability to disruptions. Generic drug supply chains are often “tightly concentrated, price-sensitive, and susceptible to disruption”.19 A lack of redundancy and heavy reliance on key starting materials (KSMs) and APIs from a limited number of countries, notably China and India, make these chains highly susceptible to disruptions caused by natural disasters, geopolitical tensions, trade restrictions, or quality-related breakdowns.19 Managing compliance across these international borders is often described as a “logistical nightmare” due to differing national standards and potential customs delays.5 While regulatory bodies like the FDA do oversee foreign suppliers through inspections, the sheer volume and geographical dispersion of manufacturing facilities globally make comprehensive policing by any single agency an immense challenge.23
Another critical issue is the lack of transparency within these complex chains. Regulations that classify manufacturing locations as “commercial confidential information” can prevent their disclosure, increasing skepticism and distrust among prescribers, pharmacists, and patients regarding the origin and quality of their medications.38 Furthermore, the intense
cost and pricing pressures faced by generic manufacturers, who operate on “razor-thin margins,” can lead to reductions in manufacturing costs to potentially unsustainable levels.19 This financial pressure, combined with the potential impact of tariffs, further stresses the supply chain and can deter investment in necessary quality improvements or advanced manufacturing technologies.19
These challenges collectively illustrate what can be understood as the Interconnected Fragility of the Global Generic Supply Chain. The globalized nature of the generic drug supply chain, while enabling significant cost efficiencies and broader access, is inherently fragile and complex. Its vulnerabilities are not merely logistical; they are deeply intertwined with the limitations of global regulatory oversight and the intense economic pressures placed upon manufacturers. A single quality issue at an API supplier in one country can trigger widespread drug shortages globally.22 The lack of transparency regarding manufacturing locations further compounds this issue, making it difficult for healthcare providers and patients to make fully informed decisions about their medications.38 This situation calls for a systemic shift in approach, moving beyond reactive detection of failures towards building greater supply chain resilience through strategies like multi-sourcing and real-time visibility, rather than solely relying on post-market detection of failures.
4.6. Addressing Data Integrity Lapses
Data integrity, while a cornerstone of pharmaceutical quality and compliance, presents a “Herculean task” in its maintenance and can become a significant liability in the increasingly digital age. Reports frequently highlight data breaches and integrity lapses directly tied to broader compliance issues.5
Common data integrity issues frequently cited in FDA warning letters and EMA non-compliance reports include a pervasive lack of access control to IT systems, often manifested through the use of shared accounts and inadequate administrative rights, which can allow unauthorized data manipulation.56 There is often a
lack of control to prevent the deletion of raw data, compromising the foundational records of studies and manufacturing.56
Inadequate audit trail review and deficient data review procedures are also common, meaning that changes to data are not properly tracked or scrutinized.56 For paper-based records, a
lack of traceability to individuals who recorded the data is a recurring problem.56 The use of
unvalidated or unprotected QMS excel spreadsheets poses a significant risk to data reliability.56 Furthermore, regulatory inspections frequently uncover
missing or incomplete original quality records, as well as illegible documentation.56 Perhaps most alarmingly, instances of
falsification of source data are reported, including manipulated chromatograms and the practice of performing “trial” injections to achieve “acceptable” results, indicating intentional deceit.57 Inadequate backup of electronic data also contributes to the vulnerability of critical information.56
The consequences of such data integrity lapses are severe and far-reaching. Data falsification has led to substantial penalties, including import bans and massive fines, as exemplified by Ranbaxy’s $500 million fine for falsified drug safety data.6 Fundamentally, these lapses undermine the safety, effectiveness, and quality of the drugs, jeopardizing public health.56
These pervasive issues underscore what can be described as the Ethical and Systemic Roots of Data Integrity Failures. Data integrity failures are not merely technical glitches or isolated incidents; they often reflect a deeper ethical and cultural problem within an organization. This can stem from intense pressure to meet production targets or cut costs, which can lead to compromised data. The widespread prevalence of issues such as shared accounts, a lack of robust audit trails, and documented data manipulation suggests a systemic failure to prioritize strong data governance and ethical conduct within these companies. This problem can be exacerbated by reliance on legacy systems that are difficult to integrate or prone to generating incorrect data.60 The consequences of such failures extend far beyond regulatory penalties, leading to a fundamental erosion of public trust, which is vital for the pharmaceutical industry’s legitimacy and success.7 Therefore, addressing data integrity requires not only robust technological solutions (e.g., integrated Quality Management Systems, automation) and stringent access controls with comprehensive audit trails but, most importantly, the cultivation of a strong organizational culture that unequivocally prioritizes integrity over expediency.
4.7. Human Error and Training Gaps
The pharmaceutical industry, particularly the generic drug sector, faces a significant challenge in securing and retaining skilled talent. It has been observed that “skilled talent is the engine of compliance, but finding it is like searching for a unicorn”.5 In 2025, a notable 56% of pharmaceutical companies reported shortages in regulatory expertise.5 This deficit is compounded by the fact that human error accounts for a substantial 54% of all compliance failures.5
The core challenges related to the human element include inadequate training, miscommunication, and high employee turnover, all of which can directly lead to costly compliance breaches and failed regulatory inspections.7 Furthermore, a lack of clearly defined procedures and Standard Operating Procedures (SOPs) contributes significantly to ambiguity in roles and responsibilities, increasing the likelihood of errors.60
This situation highlights what can be termed The Human Element: The Unpredictable Variable in Compliance. While the implementation of advanced technologies and robust quality systems is undeniably crucial for compliance, the human element remains the most unpredictable and often overlooked variable. Even the most meticulously designed system can be undermined by human error, a lack of understanding of complex procedures, or, in more severe cases, intentional misconduct. The prevailing shortage of skilled talent, coupled with the inherent financial burden of compliance, can create a vicious cycle where companies may underinvest in the very training and personnel development that could proactively prevent compliance failures. This was tragically illustrated in the McNeil/Johnson & Johnson case, where allegations suggested that aggressive cost cuts on quality assurance staff contributed to massive product recalls.69 The effectiveness of fundamental quality principles like Good Manufacturing Practices (GMP), Good Laboratory Practices (GLP), and Good Clinical Practices (GCP) is ultimately contingent upon the competency, qualification, and continuous training of all personnel involved.39 This underscores that effective compliance is not solely about adherence to rules and systems, but about fostering a deep understanding and unwavering commitment to quality and regulatory standards among all employees, from the manufacturing floor to senior management.
4.8. The Financial Burden of Compliance
A significant and often underestimated challenge in generic drug development is the substantial financial burden associated with achieving and maintaining compliance. Implementing and sustaining comprehensive compliance systems, including robust Quality Management Systems (QMS), extensive staff training programs, and rigorous audit protocols, requires “significant investment”.7 This financial and resource burden is particularly acute for smaller companies, which often struggle to allocate the necessary capital and personnel.7
The impact on margins for generic drug manufacturers is profound. Due to intense price competition in the market, these companies typically operate on “razor-thin margins”.19 This economic reality makes it exceptionally challenging for them to absorb additional costs, such as those imposed by new tariffs on imported raw materials or the substantial upfront investment required for advanced manufacturing technologies (AMTs) that could enhance quality and reduce risks.19 As one expert observed, the “regulatory approach… has driven up the costs of generic drugs”.73
Conversely, the cost of non-compliance is staggering and far outweighs the upfront investment in quality. Compliance failures lead to substantial financial losses through product recalls, regulatory penalties, and protracted legal battles.6 For example, a flawed bioequivalence study for an antihypertensive drug resulted in a $10 million cost to rectify 5, and the generic manufacturer Ranbaxy faced a monumental $500 million penalty for falsified data and quality control lapses.6
These economic realities collectively highlight what can be conceptualized as The Cost-Quality-Access Trilemma. The generic drug industry faces a fundamental trilemma in balancing the imperatives of cost-effectiveness, product quality, and patient access. The relentless pressure to keep drug prices low directly impacts manufacturers’ capacity and willingness to invest in the advanced technologies and robust quality systems that are demonstrably needed to prevent compliance failures and ensure high product quality.19 This creates an inherent tension where the pursuit of affordability can inadvertently compromise quality and, ironically, lead to drug shortages that ultimately restrict patient access. The long-term financial and reputational costs of non-compliance—including recalls, fines, and erosion of public trust—far exceed the upfront investment required for building quality into the manufacturing process.6 Yet, the immediate financial pressures often compel short-sighted decisions. This situation strongly suggests a need for supportive policy frameworks and incentives to bolster quality infrastructure within the generic sector, recognizing the true cost of producing high-quality, affordable medicines.19
5. Lessons Learned from Compliance Failures: Case Studies
Examining specific instances of compliance failures provides invaluable lessons for the generic drug industry, highlighting critical areas for improvement and emphasizing the profound consequences of cutting corners.
5.1. The Bioequivalence Blunder: Anticipating Variables
A significant lesson emerged from a 2019 incident involving a mid-sized generics firm. Their Abbreviated New Drug Application (ANDA) for a major antihypertensive drug was rejected due to a flawed bioequivalence (BE) study.5 The core issue was the study’s failure to adequately account for food effects, a critical variable in drug absorption. This oversight led to an 18-month delay in approval and incurred an estimated cost of $10 million to rectify the deficiencies.5 The critical takeaway from this experience, as noted by an executive from the firm, was a realization that “We assumed too much and tested too little”.5 This case underscores the fundamental importance of anticipating all potential variables and adopting an overly prepared, comprehensive approach in the design and execution of bioequivalence studies. It highlights that even seemingly minor omissions in study design can have substantial financial and timeline repercussions, emphasizing that precision and thoroughness are non-negotiable in demonstrating therapeutic equivalence.
5.2. The Cost of Cutting Corners: Integrity Over Expediency
The imperative of integrity over expediency is starkly illustrated by a 2022 FDA warning letter issued to an Indian manufacturer for falsified batch records.5 This severe compliance failure resulted in an immediate ban on U.S. imports for the manufacturer’s products and a significant 30% drop in its stock value.5 The unequivocal lesson from this case is that taking shortcuts, while potentially appearing to save time or resources in the short term, inevitably leads to severe and costly long-term repercussions. The principle that “Integrity beats expediency every time” is a hard-won truth in the pharmaceutical industry.5
Numerous other examples reinforce this lesson. The European Medicines Agency (EMA) took decisive action by suspending approximately 100 generic medicines that had gained market authorization based on “flawed” bioequivalence studies conducted by an Indian Contract Research Organization (CRO), Synchron Research Services.59 This points to systemic issues in data generation and oversight of third-party vendors. The notorious case of Ranbaxy Laboratories, a major generic drug producer, involved admissions of falsifying drug safety data to gain FDA approval. Their pervasive lack of quality control led to contaminated and substandard medications entering the market, culminating in a $500 million penalty and a severe loss of credibility.6 FDA warning letters issued to companies like Glenmark Pharmaceuticals have cited repeated dissolution failures and inadequate investigations into out-of-specification results, with proposed corrective actions lacking sufficient validation.63 Sun Pharmaceutical has faced recurring observations of poor aseptic behavior and inadequate environmental monitoring, including mold and liquid dripping in stability chambers.64 Daewoo Pharmaceutical was cited for mold in multiple facility areas and late testing despite patient complaints, with concerns over component contamination linked to lethal poisoning incidents.64 Furthermore, EMA non-compliance reports have consistently detailed instances of data manipulation, such as falsification of API sources, unauthorized repackaging, and the use of administrator passwords to overwrite raw data from sample testing, alongside broader Quality Management System (QMS) failures.57 These cases collectively demonstrate that data falsification and quality control lapses are not isolated incidents but often reflect a deep-seated cultural problem that prioritizes short-term gains over fundamental quality and patient safety.
5.3. Systemic Quality Failures: The McNeil/Johnson & Johnson Case
The case of McNeil Consumer Healthcare, a subsidiary of Johnson & Johnson, provides a compelling illustration of how systemic quality failures, particularly those linked to corporate strategic decisions, can lead to widespread compliance breaches and significant public health risks. A detailed five-year review of McNeil from 2007 to 2011 revealed a series of massive product recalls, including popular over-the-counter medications like Tylenol, Zyrtec, Motrin, and Benadryl.69 A notable quality assurance failure involved adult Tylenol, where the chemical breakdown of a protective coating on wooden transport pallets caused a moldy odor that was absorbed by drug containers and their contents.69
The FDA responded with stringent measures, including out-of-compliance Form 483 inspection reports and, eventually, a judicial consent decree that mandated the closure of a McNeil manufacturing plant and imposed stringent external supervision by cGMP consultants.69 Subsequent investigations and a class-action lawsuit filed on behalf of Johnson & Johnson shareholders revealed deeper systemic issues. Allegations suggested that Johnson & Johnson, following its $16.6 billion acquisition of Pfizer Consumer Healthcare in 2007, denied McNeil adequate funding for essential staff and capital improvements necessary to integrate the new product lines and maintain quality standards. Instead, the parent company was accused of recklessly imposing aggressive cost cuts on McNeil, including its quality assurance department, in an effort to boost corporate growth and profitability.69
This case demonstrates that manufacturing quality issues are not always confined to the operational level but can originate from high-level corporate decisions. When cost-cutting measures are prioritized over fundamental quality assurance and adequate investment in personnel and infrastructure, the entire quality system becomes vulnerable. The McNeil case serves as a powerful reminder that a robust quality culture must be embedded from the top down, with leadership fully committed to providing the necessary resources and oversight to ensure continuous compliance and safeguard patient safety, even amidst financial pressures or strategic acquisitions.
6. Strategies for Enhanced Compliance and Future Readiness
Addressing the multifaceted compliance challenges in generic drug development requires a holistic, proactive, and continuously adaptive approach.
6.1. Proactive Regulatory Intelligence and Engagement
Maintaining continuous awareness of the dynamic regulatory landscape is paramount. Generic drug companies must invest in robust systems for proactive regulatory intelligence, enabling them to monitor evolving guidelines, standards, and new requirements, particularly for complex generics.7 This involves not just passive monitoring but active
engagement with health authorities early in the development lifecycle. Such collaboration helps align development strategies with regulatory expectations, address potential scientific and quality concerns pre-emptively, and gain valuable guidance on innovative approaches, thereby mitigating risks and avoiding costly delays.61
The adoption of AI-based technologies is rapidly transforming this area. These tools can facilitate semi-automated regulatory intelligence tracking, streamline label updates, and map critical data attributes to international standards like Identification of Medicinal Products (IDMP).76 Leveraging Natural Language Processing (NLP) and Large Language Models (LLMs) can synthesize vast amounts of regulatory information, providing user-friendly access to updated guidelines, safety alerts, and risk categorizations.76 Furthermore, participation in and leveraging insights from scientific forums like the FDA Generic Drug Cluster can significantly enhance technical understanding and inform decision-making processes, leading to more robust regulatory evaluations and consistent global approaches.17
6.2. Robust Quality Management Systems (QMS) and Continuous Monitoring
A strong Quality Management System (QMS) is the bedrock of compliance. Companies must move beyond a mere “compliance checklist” mentality to genuinely integrate quality throughout the entire product lifecycle, from development to distribution.7 This involves several key practices:
- Standardizing Processes with Standard Operating Procedures (SOPs): Detailed SOPs for every critical task, from formulation to packaging, are essential. These procedures reduce variability, enforce consistency, and ensure products are manufactured under tightly controlled conditions.7
- Enforcing Current Good Manufacturing Practices (cGMP): Rigorous adherence to cGMP guidelines is mandatory. This ensures that manufacturing environments, equipment, personnel, and processes meet strict quality criteria, building quality into the product rather than attempting to test it in at the end.7
- Regular Audits and Inspections: Both internal audits and external inspections are critical components of a robust QMS. Internal audits should proactively simulate real regulatory inspections, focusing on high-risk areas and systematically tracking the closure of corrective actions. This process identifies gaps, verifies adherence to protocols, and drives continuous improvement.7
- Real-Time Monitoring and Corrective and Preventive Actions (CAPA): Implementing real-time monitoring tools, such as sensors, process analytics, and electronic records, allows for continuous tracking of manufacturing variables. This enables instant detection of deviations and facilitates prompt corrective actions.7 Establishing clear and structured CAPA procedures is vital for conducting thorough root cause analyses and implementing effective fixes that prevent recurrence of issues.7
- Strategic Use of GMP Certificates: In exceptional circumstances, particularly for critical medicines, the possibility of a restricted GMP certificate should be maintained. This measure can help ensure continuity of supply during periods of non-compliance remediation, provided appropriate risk assessments and supplementary measures are in place.68
6.3. Advanced Data Governance and Technology Adoption
Given the prevalence of data integrity issues, robust data governance is indispensable. Companies must implement stringent data integrity controls that adhere to the ALCOA++ principles (Attributable, Legible, Contemporaneous, Original, Accurate, Complete, Consistent, Enduring, Available) across all data types, both electronic and paper.7
Key actions include ensuring proper access control to IT systems, implementing comprehensive audit trails, and establishing secure storage protocols to prevent unauthorized alteration or deletion of raw data.56 Investment in
validated IT systems is crucial, along with efforts to integrate data from standalone equipment into networked systems to enhance traceability and accuracy.56
The strategic adoption of advanced technologies is a game-changer. Leveraging Artificial Intelligence (AI) and predictive analytics can enable companies to flag potential bioequivalence study flaws, anticipate supply chain disruptions, and identify compliance lapses before they manifest as significant problems.5 This transforms data from a mere record-keeping burden into actionable intelligence. Furthermore, digital transformation initiatives, including the use of blockchain technology for enhanced traceability, can significantly improve compliance monitoring and ensure the integrity of the supply chain.26
6.4. Strategic Intellectual Property Management
Effective management of intellectual property (IP) is crucial for generic drug manufacturers to navigate the competitive landscape and ensure timely market entry.
- Market Entry Forecasting and Portfolio Management: Generic companies must conduct thorough market and patent analyses to accurately forecast “patent cliffs”—the precise times when patents on key innovator drugs are set to expire.13 This foresight allows them to strategically manage their product portfolios and prioritize research and development (R&D) investments toward drugs nearing patent expiry, ensuring a bioequivalent generic alternative is ready for launch at the opportune moment.20
- Freedom-to-Operate (FTO) Analysis: Performing early and continuous Freedom-to-Operate (FTO) analyses is critical. This legal assessment identifies potential patent barriers that could prevent a generic product from being developed, manufactured, or commercialized without infringing existing IP rights.20 It enables companies to devise “design-around” strategies (e.g., altering chemical structures, developing new formulations, or creating novel delivery methods) or explore licensing opportunities to mitigate patent risks.20
- Paragraph IV Certifications: Strategically utilizing Paragraph IV (PIV) certifications, as incentivized by the Hatch-Waxman Act, allows generic companies to challenge existing patents listed in the FDA’s Orange Book.20 Successfully prevailing in the ensuing patent infringement lawsuit can grant the first-filer a lucrative 180-day period of market exclusivity, a powerful economic driver that creates an intense “race to file”.20
- Strategic Litigation and Settlement Considerations: Generic manufacturers must be prepared to engage in strategic litigation when challenging patents, understanding the significant legal costs, time investment, and inherent risks involved. This also includes navigating potential strategic settlements, such as “pay-for-delay” agreements or authorized generics, which profoundly shape market entry dynamics.20
- Competitive Intelligence: Comprehensive competitive intelligence tools are vital for tracking competitor pipelines, analyzing regulatory filings, understanding product positioning, and anticipating market shifts. This intelligence informs strategic decision-making across all aspects of generic drug development and launch.32
6.5. Building Resilient Global Supply Chains
The inherent complexities and vulnerabilities of the global generic drug supply chain necessitate proactive strategies to enhance resilience and ensure continuous supply of quality medicines.
- Multi-Sourcing Models: Implementing multi-sourcing models for raw materials and Active Pharmaceutical Ingredients (APIs) is crucial to reduce over-reliance on single geographies or suppliers. This diversification enhances resilience against regional disruptions, natural disasters, geopolitical tensions, or trade restrictions.19
- Improved Material Availability and Visibility: Achieving real-time visibility across the entire value chain is critical for ensuring material availability and improving “On-Time, In-Full” (OTIF) delivery. This can be facilitated through multi-tier supply networks with pre-screened supplier profiles, enabling quicker supplier switching when needed.22
- Smart Logistics and Traceability: Utilizing smart logistics solutions, including cold chain monitoring and lot/batch level traceability, is essential for maintaining product quality and ensuring regulatory and patient compliance throughout the distribution process.22
- Digitization of Quality and Batch Release: Implementing a Quality System of Intelligence that digitizes the batch release process and provides predictive insights, alerts, and scenario planning can significantly improve supply chain responsiveness and prevent quality-related breakdowns.22
- Proactive Trade Policy Adaptation: Companies must proactively address the potential impacts of evolving trade policies and tariffs by building internal customs compliance capabilities. This includes expertise in tariff classification, country of origin documentation, and accurate customs valuation, enabling them to prepare for enforcement and audit risks while optimizing supply chain transactions.19
6.6. Fostering a Culture of Quality and Continuous Learning
Ultimately, compliance is not solely a matter of systems and procedures; it is deeply rooted in an organization’s culture and the capabilities of its people.
- Prioritizing Talent and Training: Recognizing that “skilled talent is the engine of compliance” 5, companies must prioritize regulatory expertise and invest in continuous, role-specific training for all employees. This training should incorporate hands-on learning, simulations, and real-time updates on regulatory changes to ensure employees are prepared to make compliant decisions in their day-to-day work.7
- Cultivating Open Communication: Fostering a culture of open communication is vital, where employees are encouraged to ask questions and report issues without fear of reprisal. Training should emphasize why compliance matters, not just what the rules are, integrating compliance into onboarding and role changes to ensure clear expectations.7
- Leadership Commitment: Leadership must model compliance-first behavior, actively recognize and reward compliance initiatives, and hold all teams accountable. Embedding compliance-related Key Performance Indicators (KPIs) into employee evaluations helps reinforce that compliance is a shared responsibility and a core driver of business success.77
- Integrating Quality: Moving beyond a “compliance checklist” mentality, teams should be encouraged to prioritize quality at every stage, from clinical research to product release, understanding that strong quality practices naturally lead to regulatory compliance.77 A “highly developed culture of quality spends, on average, $350 million less annually fixing mistakes than a company with a poorly developed one,” demonstrating the tangible return on investment for quality.74
- Addressing Patient Perceptions: Companies must also address patient perceptions regarding generic drug appearance and provide comprehensive patient counseling during brand-to-generic transitions. Studies indicate that patients are more likely to stop taking their generic medications when they experience a change in their drugs’ physical appearance, even if the generic is therapeutically equivalent.53 The FDA encourages generic manufacturers to consider physical attributes in development.53 Healthcare professionals play a critical role in conveying the FDA’s commitment to ensuring the quality and safety of all approved products.3
- Building Public Trust: Ultimately, the pharmaceutical industry’s legitimacy depends on public confidence. Any lapse in compliance, such as data falsification or off-label marketing, can severely damage reputations and reduce patient willingness to use vital treatments.7 Transparency, particularly regarding manufacturing locations and quality documentation, is crucial to address skepticism and distrust.38
7. Conclusion: Towards a More Resilient and Compliant Generic Drug Future
The journey of generic drug development is characterized by a complex interplay of scientific rigor, regulatory demands, economic pressures, and global supply chain intricacies. The analysis presented highlights that compliance challenges in this sector are not isolated incidents but often stem from systemic vulnerabilities, including rapidly evolving regulatory landscapes, the nuanced scientific demands of bioequivalence, the critical need for robust manufacturing quality, the strategic complexities of intellectual property disputes, the pervasive issue of data integrity lapses, the impact of human error and training gaps, and the overarching financial burden of compliance on razor-thin margins.
The lessons learned from past failures are unequivocal: superficial compliance or “cutting corners” inevitably leads to severe consequences, far outweighing any perceived short-term gains. The cases of bioequivalence blunders, data falsification, and systemic quality breakdowns underscore the absolute necessity of prioritizing integrity, thoroughness, and a proactive approach at every stage of development and manufacturing.
Moving forward, the future of generic drug development hinges on a comprehensive and integrated strategy. This includes continuous investment in proactive regulatory intelligence and engagement with health authorities, the establishment and rigorous maintenance of robust Quality Management Systems with continuous monitoring capabilities, and the strategic adoption of advanced technologies for data governance, predictive analytics, and supply chain resilience. Mastering intellectual property management, including FTO analysis and strategic litigation, remains critical for navigating market entry. Furthermore, building truly resilient global supply chains through multi-sourcing and enhanced transparency is paramount to mitigate risks and ensure consistent supply.
Crucially, fostering a pervasive culture of quality and continuous learning throughout the organization is indispensable. This involves prioritizing talent development, providing role-specific training, encouraging open communication, and ensuring unwavering leadership commitment to ethical conduct and quality standards. As FDA officials have emphasized, leveraging regulatory science is key to advancing the generic drug program, promoting competition, and improving access to healthcare.17 The industry must continue to adapt to evolving regulations, deepen its scientific understanding for complex products, and engage in stronger global collaborative efforts among regulators and industry stakeholders to ensure that safe, high-quality, and affordable medicines remain accessible to patients worldwide. This may also involve exploring policy incentives to support the adoption of advanced manufacturing technologies and strengthen domestic production capabilities, thereby enhancing overall supply chain security and quality.19 The path to a more resilient and compliant generic drug future requires a sustained commitment to excellence that transcends mere regulatory checkboxes and embraces a holistic vision for patient well-being.
Works cited
- Office of Generic Drugs 2022 Annual Report – FDA, accessed July 25, 2025, https://www.fda.gov/drugs/generic-drugs/office-generic-drugs-2022-annual-report
- Generic Drugs Market Size, Research, Trends and Forecast – Towards Healthcare, accessed July 25, 2025, https://www.towardshealthcare.com/insights/generic-drugs-market
- A Real-World Case Study of Levothyroxine Use Addresses Institutional Concerns About Generic Product Interchangeability | FDA, accessed July 25, 2025, https://www.fda.gov/drugs/spotlight-cder-science/real-world-case-study-levothyroxine-use-addresses-institutional-concerns-about-generic-product
- Generic Drugs – FDA, accessed July 25, 2025, https://www.fda.gov/drugs/buying-using-medicine-safely/generic-drugs
- Compliance Challenges in Generic Drug Development: Lessons …, accessed July 25, 2025, https://www.drugpatentwatch.com/blog/compliance-challenges-in-generic-drug-development-lessons-learned/
- From Lab to Lawsuit: What Happens When Pharma Skips Regulatory Steps?, accessed July 25, 2025, https://emmainternational.com/from-lab-to-lawsuit-what-happens-when-pharma-skips-regulatory-steps/
- Understanding Pharmaceutical Compliance: Challenges and Best Practices – V-comply, accessed July 25, 2025, https://www.v-comply.com/blog/pharmaceutical-compliance-challenges/
- Generic Drug Development Hindered by Evolving FDA Guidelines, Quality Control: Analysis, accessed July 25, 2025, https://www.geneonline.com/generic-drug-development-hindered-by-evolving-fda-guidelines-quality-control-analysis/
- Generic Drug Developers Face Compliance Hurdles Amid Evolving FDA Regulations and Stringent Quality Control Mandates. – GeneOnline, accessed July 25, 2025, https://www.geneonline.com/generic-drug-developers-face-compliance-hurdles-amid-evolving-fda-regulations-and-stringent-quality-control-mandates/
- Generic and hybrid medicines – EMA – European Union, accessed July 25, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/marketing-authorisation/generic-hybrid-medicines
- Generic Drugs: Questions & Answers – FDA, accessed July 25, 2025, https://www.fda.gov/drugs/frequently-asked-questions-popular-topics/generic-drugs-questions-answers
- What is a generic drug, and how does it get approved? – Patsnap Synapse, accessed July 25, 2025, https://synapse.patsnap.com/article/what-is-a-generic-drug-and-how-does-it-get-approved
- The Impact of Patent Expirations on Generic Drug Market Entry – PatentPC, accessed July 25, 2025, https://patentpc.com/blog/the-impact-of-patent-expirations-on-generic-drug-market-entry
- The ANDA Process: A Guide to FDA Submission & Approval – Excedr, accessed July 25, 2025, https://www.excedr.com/blog/what-is-abbreviated-new-drug-application
- What is ANDA? – UPM Pharmaceuticals, accessed July 25, 2025, https://www.upm-inc.com/what-is-anda
- Dr. Scott Gottlieb’s first speech as FDA head: 4 quotes – Becker’s Hospital Review, accessed July 25, 2025, https://www.beckershospitalreview.com/supply-chain/dr-scott-gottlieb-s-first-speech-as-fda-head-4-quotes/
- Remarks to FDA employees on Generic Drug Science Day – 11/28/2017, accessed July 25, 2025, https://www.fda.gov/news-events/speeches-fda-officials/remarks-fda-employees-generic-drug-science-day-11282017
- Generic Drugs Market Size, Share And Trends Report, 2033 – Nova One Advisor, accessed July 25, 2025, https://www.novaoneadvisor.com/report/generic-drugs-market
- USP Expert Discusses Balancing Drug Cost, Quality, and Access in a Changing Trade Landscape – Pharmacy Times, accessed July 25, 2025, https://www.pharmacytimes.com/view/usp-expert-discusses-balancing-drug-cost-quality-and-access-in-a-changing-trade-landscape
- Overcoming Formulation Challenges in Generic Drug Development …, accessed July 25, 2025, https://www.drugpatentwatch.com/blog/overcoming-formulation-challenges-in-generic-drug-development/
- Tariffs & Trade Policy: What to Watch for, Cost Impacts, and Supply Chain Strategies, accessed July 25, 2025, https://www.pharmtech.com/view/tariffs-trade-policy-what-to-watch-for-cost-impacts-and-supply-chain-strategies
- Optimizing the Generic Drug Supply Chain: Strategies for Success – DrugPatentWatch, accessed July 25, 2025, https://www.drugpatentwatch.com/blog/optimizing-the-generic-drug-supply-chain-strategies-for-success/
- Competition And Vulnerabilities In The Global Supply Chain For US Generic Active Pharmaceutical Ingredients | Health Affairs, accessed July 25, 2025, https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2022.01120?journalCode=hlthaff
- Considerations for FDA’s New Advanced Pharmaceutical Manufacturing Programs, accessed July 25, 2025, https://healthpolicy.duke.edu/publications/considerations-fdas-new-advanced-pharmaceutical-manufacturing-programs
- INVESTIGATING GENERICS: America’s Overlooked Drug Crisis – MedShadow Foundation | Independent Health & Wellness Journalism, accessed July 25, 2025, https://medshadow.org/are-generic-drugs-safe/
- The Significance of Generic Compliance Ratios in the Pharmaceutical Industry – Drugzone, accessed July 25, 2025, https://www.drugzone.com/blog/the-significance-of-generic-compliance-ratios-in-the-pharmaceutical-industry
- Abbreviated New Drug Application (ANDA) Approval Process – FDA, accessed July 25, 2025, https://www.fda.gov/media/166141/download
- Navigating the ANDA and FDA Approval Processes – bioaccess, accessed July 25, 2025, https://www.bioaccessla.com/blog/navigating-the-anda-and-fda-approval-processes
- Generic and hybrid applications | European Medicines Agency (EMA), accessed July 25, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/marketing-authorisation/generic-hybrid-medicines/generic-hybrid-applications
- From lab to patient – Timeline | European Medicines Agency (EMA), accessed July 25, 2025, https://www.ema.europa.eu/en/from-lab-to-patient-timeline
- Hatch-Waxman 101 – Fish & Richardson, accessed July 25, 2025, https://www.fr.com/insights/thought-leadership/blogs/hatch-waxman-101-3/
- What is Competitive Intelligence in the pharmaceutical industry? – Lifescience Dynamics, accessed July 25, 2025, https://www.lifesciencedynamics.com/press/articles/what-is-competitive-intelligence-in-the-pharma-industry/
- E6(R2) Good Clinical Practice: Integrated Addendum to ICH E6(R1) (March 2018) – FDA, accessed July 25, 2025, https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e6r2-good-clinical-practice-integrated-addendum-ich-e6r1
- FDA and EMA inspections: Similarities and Differences | Scilife, accessed July 25, 2025, https://www.scilife.io/blog/fda-and-ema-inspections-pharma
- The Generic Drug Cluster Third Anniversary Reflection – FDA, accessed July 25, 2025, https://www.fda.gov/drugs/generic-drugs/generic-drug-cluster-third-anniversary-reflection
- Good manufacturing practice | European Medicines Agency (EMA), accessed July 25, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/research-development/compliance-research-development/good-manufacturing-practice
- Stability and bioequivalence challenges in generic drug formulation: A regulatory perspective – GSC Online Press, accessed July 25, 2025, https://gsconlinepress.com/journals/gscbps/sites/default/files/GSCBPS-2025-0189.pdf
- Is the Quality of Generic Drugs Cause for Concern? – PMC, accessed July 25, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10391121/
- Good Manufacturing Practice (GMP) | Definitive Healthcare, accessed July 25, 2025, https://www.definitivehc.com/resources/glossary/good-manufacturing-practice
- What is GMP | Good Manufacturing Practices | SafetyCulture, accessed July 25, 2025, https://safetyculture.com/topics/gmp/
- FDA 21 CFR Part 210-211 Compliance – MasterControl, accessed July 25, 2025, https://www.mastercontrol.com/compliance/21-cfr-regulations/210-211/
- Ensuring Drug Quality: An Overview of 21 CFR Parts 210 & 211 – Eurofins USA, accessed July 25, 2025, https://www.eurofinsus.com/food-testing/resources/ensuring-drug-quality-an-overview-of-21-cfr-parts-210-211/
- Facts About the Current Good Manufacturing Practice (CGMP) – FDA, accessed July 25, 2025, https://www.fda.gov/drugs/pharmaceutical-quality-resources/facts-about-current-good-manufacturing-practice-cgmp
- GMP Requirements in the European Union – MIAS Pharma, accessed July 25, 2025, https://miaspharma.com/gmp-requirements-in-the-european-union/
- Understanding Good Laboratory Practices (GLP): A Comprehensive Guide – JAF Consulting, accessed July 25, 2025, https://jafconsulting.com/blog/understanding-good-laboratory-practices-glp-a-comprehensive-guide/
- How to Comply with FDA Good Laboratory Practice Requirements – Lab Manager, accessed July 25, 2025, https://www.labmanager.com/how-to-comply-with-fda-good-laboratory-practice-requirements-28204
- Good laboratory practice | European Medicines Agency (EMA), accessed July 25, 2025, https://www.ema.europa.eu/en/glossary-terms/good-laboratory-practice
- What is GLP & Why Is Good Laboratory Practice Important? – Allucent, accessed July 25, 2025, https://www.allucent.com/resources/blog/what-are-good-laboratory-practices-glp-nonclinical-studies
- ICH E6 (R3) Guideline on good clinical practice (GCP)_Step 5 – EMA, accessed July 25, 2025, https://www.ema.europa.eu/en/documents/scientific-guideline/ich-e6-r3-guideline-good-clinical-practice-gcp-step-5_en.pdf
- Q&A: Good clinical practice (GCP) | European Medicines Agency (EMA), accessed July 25, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/research-development/compliance-research-development/good-clinical-practice/qa-good-clinical-practice-gcp
- Bioequivalence Study In Generic Products – Veeprho, accessed July 25, 2025, https://veeprho.com/bioequivalence-study-in-generic-products/
- Quotes by Katherine Eban (Author of Bottle of Lies) – Goodreads, accessed July 25, 2025, https://www.goodreads.com/author/quotes/448928.Katherine_Eban
- Utilizing Generic Drug Awareness to Improve Patient Outcomes with Dr. Sarah Ibrahim | FDA, accessed July 25, 2025, https://www.fda.gov/drugs/news-events-human-drugs/utilizing-generic-drug-awareness-improve-patient-outcomes-dr-sarah-ibrahim
- Data Integrity | ISPE | International Society for Pharmaceutical Engineering, accessed July 25, 2025, https://ispe.org/topics/data-integrity
- What is data integrity in pharma and what are the five principles? – Eurofins, accessed July 25, 2025, https://www.eurofins.com/assurance/resources/articles/what-is-data-integrity-in-pharma-and-what-are-the-five-principles/
- Data Integrity: A hot topic in FDA Warning Letters – PharmOut, accessed July 25, 2025, https://www.pharmout.net/data-integrity-fda/
- Already 13 EMA GMP Non-compliance Reports in 2016 published – ECA Academy, accessed July 25, 2025, https://www.gmp-compliance.org/gmp-news/already-13-ema-gmp-non-compliance-reports-in-2016-published
- EMA publishes several GMP Non Compliance Reports – ECA Academy, accessed July 25, 2025, https://www.gmp-compliance.org/gmp-news/ema-publishes-several-gmp-non-compliance-reports
- Euro Roundup: EMA moves to suspend 100 generic drugs over ‘flawed studies’ run by Indian CRO | RAPS, accessed July 25, 2025, https://www.raps.org/news-and-articles/news-articles/2022/5/euro-roundup-ema-moves-to-suspend-100-generic-drug
- 7 Common Compliance Issues Faced By Pharmaceutical Industry, accessed July 25, 2025, https://www.qualityze.com/blogs/7-common-compliance-issues-faced-by-pharmaceutical-industry
- Challenges to Navigating the Pharmaceutical Regulatory Landscape, accessed July 25, 2025, https://www.pharmexec.com/view/challenges-navigating-regulatory-landscape
- How Generic Drugs Are Developed : Pharmaceutical process – ZIM Labs, accessed July 25, 2025, https://www.zimlab.in/blog-posts/how-generic-drugs-are-developed-a-deep-dive-into-the-pharmaceutical-process
- Glenmark Pharmaceuticals Limited – 708270 – 07/11/2025 – FDA, accessed July 25, 2025, https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/warning-letters/glenmark-pharmaceuticals-limited-708270-07112025
- FDA hands down citations to 3 drugmakers after inspections found contamination, testing concerns | Fierce Pharma, accessed July 25, 2025, https://www.fiercepharma.com/manufacturing/fda-hands-down-manufacturing-citations-3-drugmakers-after-inspections-found
- Daewoo Pharmaceutical Co., Ltd. – 706371 – 07/02/2025 – FDA, accessed July 25, 2025, https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/warning-letters/daewoo-pharmaceutical-co-ltd-706371-07022025
- Case Studies: How Unsafe Drugs Can Reach Patients | The Pew Charitable Trusts, accessed July 25, 2025, https://www.pew.org/en/research-and-analysis/issue-briefs/2014/02/26/case-studies-how-unsafe-drugs-can-reach-patients
- Threat in Your Medicine Cabinet: The FDA’s Gamble on America’s Drugs, accessed July 25, 2025, https://www.propublica.org/article/fda-drug-loophole-sun-pharma
- efpia-comments-eu-template-for-gmp-non-compliance-statement_final.docx, accessed July 25, 2025, https://www.efpia.eu/media/361857/efpia-comments-eu-template-for-gmp-non-compliance-statement_final.docx
- McNeil, a Johnson & Johnson Subsidiary FDA Case Study – CSUSB ScholarWorks, accessed July 25, 2025, https://scholarworks.lib.csusb.edu/cgi/viewcontent.cgi?article=1359&context=ciima
- Pharmaceutical Patent Disputes: Generic Entry for Small-Molecule Drugs Under the Hatch-Waxman Act | Congress.gov, accessed July 25, 2025, https://www.congress.gov/crs-product/IF13028
- The Role of Patents and Regulatory Exclusivities in Drug Pricing | Congress.gov, accessed July 25, 2025, https://www.congress.gov/crs-product/R46679
- Trade Policy Shifts: Compliance and Cost Strategies for Pharma, accessed July 25, 2025, https://www.pharmtech.com/view/trade-policy-shifts-compliance-and-cost-strategies-for-pharma
- Regulatory Quotes – BrainyQuote, accessed July 25, 2025, https://www.brainyquote.com/topics/regulatory-quotes
- FDA 483 Trends – Regulatory Compliance Associates, accessed July 25, 2025, https://www.rcainc.com/published-articles/fda-483-trends/
- “Improving Generic Drug Approval at the FDA” by Kathleen Craddock – University of Michigan Law School Scholarship Repository, accessed July 25, 2025, https://repository.law.umich.edu/mjeal/vol7/iss2/6/
- How Pharma Companies Are Solving Regulatory Challenges with AI-based Technology, accessed July 25, 2025, https://www.americanpharmaceuticalreview.com/Featured-Articles/611954-How-Pharma-Companies-Are-Solving-Regulatory-Challenges-with-AI-based-Technology/
- Guidelines for Pharmaceutical Compliance and Best Practices – V-comply, accessed July 25, 2025, https://www.v-comply.com/blog/pharmaceutical-compliance-best-practices/
- How to Implement a Successful Generic Drug Launch Strategy …, accessed July 25, 2025, https://www.drugpatentwatch.com/blog/how-to-implement-a-successful-generic-drug-launch-strategy/