This article was originally published by Ekaterina Galkina Cleary, Jennifer M. Beierlein, Navleen Surjit Khanuja, Laura M. McNamee and Fred D. Ledley in PNAS under a Creative Commons Attribution-NonCommercial-NoDerivatives License 4.0 (CC BY-NC-ND).
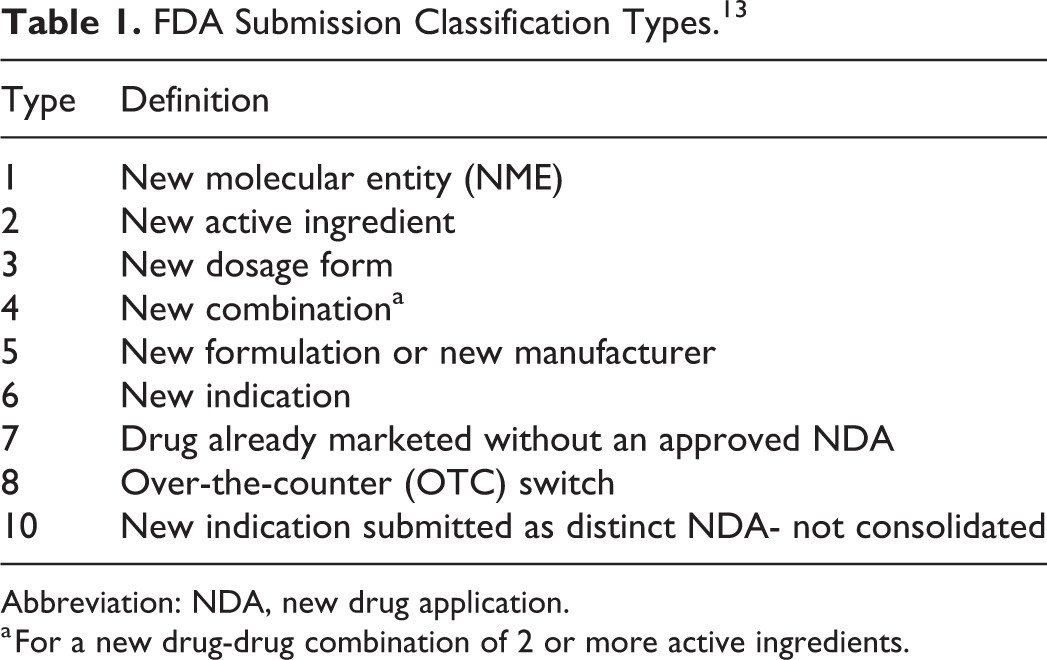
Significance
This report shows that NIH funding contributed to published research associated with every one of the 210 new drugs approved by the Food and Drug Administration from 2010–2016. Collectively, this research involved >200,000 years of grant funding totaling more than $100 billion. The analysis shows that >90% of this funding represents basic research related to the biological targets for drug action rather than the drugs themselves. The role of NIH funding thus complements industry research and development, which focuses predominantly on applied research. This work underscores the breath and significance of public investment in the development of new therapeutics and the risk that reduced research funding would slow the pipeline for treating morbid disease.
Abstract
This work examines the contribution of NIH funding to published research associated with 210 new molecular entities (NMEs) approved by the Food and Drug Administration from 2010–2016. We identified >2 million publications in PubMed related to the 210 NMEs (n = 131,092) or their 151 known biological targets (n = 1,966,281). Of these, >600,000 (29%) were associated with NIH-funded projects in RePORTER. This funding included >200,000 fiscal years of NIH project support (1985–2016) and project costs >$100 billion (2000–2016), representing ∼20% of the NIH budget over this period. NIH funding contributed to every one of the NMEs approved from 2010–2016 and was focused primarily on the drug targets rather than on the NMEs themselves. There were 84 first-in-class products approved in this interval, associated with >$64 billion of NIH-funded projects. The percentage of fiscal years of project funding identified through target searches, but not drug searches, was greater for NMEs discovered through targeted screening than through phenotypic methods (95% versus 82%). For targeted NMEs, funding related to targets preceded funding related to the NMEs, consistent with the expectation that basic research provides validated targets for targeted screening. This analysis, which captures basic research on biological targets as well as applied research on NMEs, suggests that the NIH contribution to research associated with new drug approvals is greater than previously appreciated and highlights the risk of reducing federal funding for basic biomedical research.
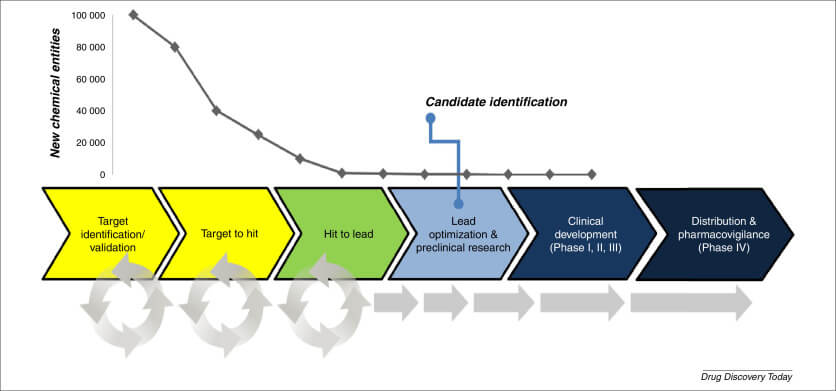
Ongoing public debate concerning budget allocations for the NIH and the propriety of pharmaceutical pricing have raised questions about the roles of the public and private sectors in drug discovery and development. The classic linear model of innovation in drug development posits that basic research, or use-inspired basic research (1), provides a scientific foundation for drug discovery by elucidating mechanisms of disease and strategies for therapy, validating drug targets, and, sometimes, identifying prototype compounds (2). This research is funded largely by the public sector, primarily by government (3), and is performed principally in academic institutions or government laboratories. The insights and intellectual property arising from this basic research are then transferred to the private sector for development. Biopharmaceutical companies are responsible for conducting applied preclinical research and clinical research, obtaining regulatory approval, and establishing the manufacturing, control, distribution, and marketing required to commercialize a new molecular entity (NME). This development is funded primarily from the profits generated by earlier products as well as by capital investments. This simplified model does not account for dynamic interactions that occur at the boundary between the academic and commercial sectors (4), contributions made to use-inspired basic research by the biotechnology and pharmaceutical industries (5–7), or efforts to promote translational science in the public domain (2, 8, 9). Nevertheless, this model is commonly invoked by scientists and policy makers alike to justify government support for basic biomedical research.
The timelines and costs involved in the commercial development of an NME have been extensively characterized (10–15). Recent data suggest that companies invest an average of $1.4 billion in out-of-pocket expenses for each NME launched, with the total cost of capital exceeding $2.5 billion (10).
Quantifying the contribution of public-sector funding to the emergence of new drugs is less well characterized. Stevens et al. (16) assessed how many NMEs arise from public-sector research institutions by identifying patents licensed by biopharmaceutical companies from academic institutions. Their analysis showed that 9.3% of NMEs approved from 1990–2007 were patented by public-sector institutions and subsequently licensed to commercial entities for development. These results are consistent with studies examining patents cited in the Food and Drug Administration’s (FDA’s) Orange Book (17), which suggest that 7.6% of drugs approved 1981–1990 (18) and 6.7% of new drugs approved 1990–1999 (11) originated in academia.
Using an analogous approach, Sampat (19) has estimated that 7.7% of all FDA approvals and 10.6% of NMEs are based on academic patents. Expanding on this analysis, Sampat and Lichtenberg (20) explored the indirect contributions of public-sector funding to drug patents by characterizing the prior art referenced in these patents. Their studies show that, of 379 drugs approved from 1988–2007, 48% were associated with a patent that cited prior art generated in the public sector. Kneller (21) also examined this indirect contribution by examining patents that described novel biological targets and prototype compounds, concluding that nonprofit research organizations made major contribution to the patent estate for 14% of NMEs approved from 1998–2007 and some contribution to 35% of NMEs. This fraction is consistent with the results of Patridge et al. (22), who found that for 38% of FDA-approved NMEs the first synthesis or purification of the molecular entity was reported from an academic institution.
Case-study analysis suggests the public-sector contribution to NME discovery and development may be even higher. Cockburn and Henderson (23) examined the development of 21 drugs that had the “most impact” on practice from 1965–1992, observing that 76% were associated with some input from the public sector. Chakravarthy et al. (6) studied the discovery and development of the 19 “most transformative” drugs of the past 25 y, concluding that the public sector contributed to the basic science underlying 54% of these NMEs but contributed directly to the discovery of only 15%. Similar results were obtained in the overlapping analysis by Zycher et al. (5).
We have previously explored the relationship between the advance of biomedical research and the emergence of NMEs from this research (24, 25). We used an analytical model for the growth and maturation of research that quantifies technology growth based on the rate of accumulation of publications in PubMed. These studies show that the growth of research on novel drug targets follows a characteristic S-curve pattern, with a point of initiation leading to a phase of exponential growth, which slows as the technology becomes established. Studies on more than 400 NMEs show that few NMEs discovered through targeted screening or biological products are approved when the underlying research is in the exponential growth phase and that NME approval occurs an average of 14 y after the established point (26–28). These data are consistent with the expectation that targeted drug discovery, including biologicals, is enabled by a body of basic research, which identifies and validates drug targets as well as potential mechanisms for therapeutic action (29, 30). In contrast, our analysis shows no relationship between metrics of technology growth and approval of NMEs discovered through phenotypic methods (26, 28), consistent with the expectation that phenotypic discovery is not predicated on knowledge of drug targets or mechanisms of action (31–34).
In the present study, we examined the scope of NIH support for published research associated with the 210 NMEs approved by the FDA from 2010–2016. Specifically, we used PubMed to identify publications related to each of these NMEs as well as the 151 known molecular targets for these drugs. We then used the NIH RePORTER database to identify publications that cited NIH funding, the core projects (i.e., grants) that supported this research, and the fiscal-year costs of those projects. We specifically focused on the 84 first-in-class drugs approved from 2010–2016, identifying publications, projects, and project costs leading to the first approval of these innovative therapeutics.
We identified NIH-funded research associated with every one of the 210 NMEs approved from 2010–2016, most of which was focused on the biological targets rather than on the drugs themselves. This research comprises over 2 million publications and was supported by more than 200,000 fiscal years of federal (primarily NIH) funding totaling more than $100 billion. These results demonstrate the scale of basic research involved in bringing a novel product to market and the magnitude of public sector support for this research.
Methods
NMEs approved by the FDA from 2010–2016 were identified from FDA reports (35) and designated “first in class” or “follow-on” based on assessment by the FDA (36). NMEs were designated “phenotypic” or “targeted” based on the criteria of Swinney et al. (29, 30). Known molecular targets for each NME and approved clinical indications were determined from FDA labels (37) and other sources as described in SI Methods. For biological products comprising a naturally occurring protein, the target is considered to be the normal counterpart of the biological product.
PubMed searches were performed for each drug (“drug search”) using an ontology of drug name synonyms in ChEMBL (38) and the National Center for Biotechnology Information (NCBI) Query Translation. PubMed searches for molecular targets (“target searches”) were performed using Boolean search terms and NCBI Query Translation. The PubMed Identifier (PMID) was recorded for each publication identified in the search.
Data associating publications with specific NIH-funded projects were obtained from the RePORTER/ExPORTER format files catalog (39). The “Link Tables for Project to Publication Associations” (hereafter, “Link Table”) associates PMIDs from 1980–present with projects that provided research funding and the PMID year. Each PMID was associated with a funding year corresponding to the project number and year in the Link Table. The Project Data Table provides the fiscal year cost for each project (2000–present). Costs were assigned for each funding year corresponding to the program cost in the year associated with the PMID in the Link Table. For publications with dates 1–4 y after the end of the project, costs for the final year of the project were used. The activity code associated with the core project number indicates the grant type.
Redundant identification of PMIDs and funding years occurred when a publication was identified in different drug or target searches or was cited in more than one supporting project. Consequently, each analysis required two steps, first identifying all PMIDs or project years with the specific properties being characterized and then eliminating duplicates within that subset.
Funding years were categorized as “drug” if one or more of the PMIDs associated with that project were identified in a drug search. Funding years were categorized as “target only” if every PMID associated with that project was identified through target searches. The process is illustrated in a schematic (Fig. S1), and an illustrative example (venetoclax) is shown in Fig. S2.
Data analysis and visualization were performed in PostgreSQL, Excel, and Tableau. All costs are given in constant dollars inflation-adjusted to 2016 using the US Bureau of Labor Statistics’ consumer price index (CPI) (40). A more detailed description of the analytical methods is provided in SI Methods. The search terms, summary statistics of each search, and complete dataset of PMIDs and associated funding years are provided in Dataset S1.
Results
Publications, NIH Funding Years, and Project Costs Associated with NMEs Approved 2010–2016.
The FDA approved 210 NMEs from 2010–2016. Of these, 197 NMEs were associated with 151 known molecular targets (Dataset S2), while 13 have no known target. This set of NMEs includes 84 first-in-class products associated with 77 novel molecular targets.
A total of 131,092 publications were identified from the 210 drug searches, and 1,966,481 publications were identified from the 151 target searches (Table 1). Of the 2,097,573 total publications identified, 610,702 (29%) were associated with one or more NIH-funded projects in the RePORTER database (Table 1). This includes 17% of the publications identified from drug searches and 30% of the publications identified from target searches. These fractions are consistent with data showing that 29–35% of entries in PubMed originate from US institutions (3, 41, 42). Significantly, 94% of all publications and 96% of the publications associated with NIH funding were identified through target searches rather than drug searches. Data from individual drug and target searches are described in Tables S2 and S3.
Table 1.
Research publications, funding years, and project costs associated with 210 NMEs approved 2010–2016 or their molecular targets
| Metrics | Drug | Target | Total |
| PubMed results | |||
| Searches | 210 | 151 | 361 |
| Publications | 131,092 | 1,966,481 | 2,097,573 |
| NIH funding | |||
| Publications (%) | 22,706 (17) | 587,996 (30) | 610,702 (29) |
| Searches (%) | 198 (94) | 151 (100) | |
| Funding years 1980–2016 | 14,292 | 207,599* | 221,891 |
| Funding years with costs | 10,031 | 150,278* | 160,309 |
| Costs 2000–2016, billion $ | 12.5 | 102.8* | 115.3 |
-
↵* Target only.
Overall, NIH-supported publications were identified in 198 of the 210 drug searches and in all 151 target searches. Thus, NIH funding was directly or indirectly associated with every one of the 210 NMEs approved from 2010–2016.
We identified 221,891 funding years associated with the corpus of published research. Of these, 14,292 funding years were associated with publications identified in one or more drug searches and represent applied research related to the NME. The other 207,599 funding years were associated with publications identified in target searches but not drug searches (target only). These publications and funding years represent more basic research, which contributes to the body of knowledge related to the drug target without explicit reference to the NME (Table 1).
Analysis of the grant activity codes showed that the largest fraction of grants were R01 research project grants (53%), followed by T32 training programs (6%), P01 research program projects (4%), and ZIA intramural research programs (4%) (Fig. S4 and Table S3).
The time course of publications and funding years is shown in Fig. 1. Publications identified through target searches increased through the 1970s and then slowed after 2010. Publications identified through drug searches showed little growth through the 2000s and then accelerated after 2007 (Fig. 1A). The growth of NIH-funded publications exhibited a parallel pattern (Fig. 1 A and B). The time course of funding years mirrors the growth of NIH-funded publications, with the number of funding years related to molecular targets increasing from the 1980s and the number of funding years directly related to the NMEs increasing only in the late 2000s (Fig. 1C).
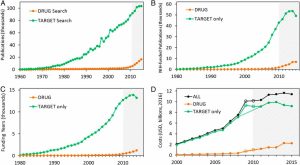
PMIDs, NIH-funded PMIDs, NIH funding year, and costs associated with 210 NMEs approved from 2010–2016 or the 151 known molecular targets for these NMEs. (A) PMIDs identified searching for NMEs (drug search) or their molecular targets (target search). (B) PMIDs associated with NIH funding in RePORTER (1980–present). (C) Funding years associated with NIH-funded PMIDs directly related to NMEs (drug) or their targets (target only). (D) Project costs (2000–2016) associated with funding years (all), costs directly related to the NMEs (drug), or costs related to the molecular target only (target only). Open circles indicate years of supplemental funding from the ARRA. Dashed line shows trend without ARRA data. Shaded areas show the years of drug approvals.
We associated the cost of one fiscal year of project funding with 160,309 funding years. The inflation-adjusted costs for these funding years totaled $115.3 billion, with $12.5 billion for funding years associated with publications related to the NMEs and $102.8 billion for funding years associated with publications on molecular targets (Table 1). The average cost of each funding year associated with publications identified in a drug search was significantly greater than the cost of funding years associated with publications identified in target-only searches ($1.20 million versus $684,000). The time course of costs paralleled the growth of publications and funding years, with the exception of 2009–2010 when the costs were significantly higher (Fig. 1D). This discrepancy is consistent with the increased NIH funding provided by the American Recovery and Reinvestment Act (ARRA), which provided a supplemental allocation of $10.4 billion from 2009–2010, of which $8.2 billion was invested in research (43).
Therapeutic Areas.
The largest fraction of NMEs approved from 2010–2106 were antineoplastic agents, followed by antiinfectives (primarily for HIV and hepatitis) and metabolic, cardiovascular, immunologic, and central nervous system therapies. Costs associated with NMEs for major therapeutic indications are shown in Fig. S5. The number of NMEs in each therapeutic area was correlated with both drug costs and target costs (r2 > 0.86, d.f. = 9). For each indication, costs associated with research on molecular targets constituted >85% of the total costs.
NIH Contribution to First-in-Class NMEs.
The 210 NMEs approved from 2010–2016 include 84 first-in-class NMEs, defined as NMEs that work through a novel mechanism of action or molecular target. These 84 first-in-class NMEs are associated with 77 unique molecular targets. To assess the NIH funding that contributed to the emergence of first-in-class compounds, we clustered PMID, funding year, and cost data for each of these 77 targets with data for each of the drugs associated with these targets. Clusters were characterized as “first in class” if the first-in-class NME against that target was discovered using targeted screening methods (including biological products) or phenotypic methods (29, 30). There were 67 clusters with first-in-class NMEs discovered by targeted screening and 10 clusters with first-in-class NMEs discovered through phenotypic methods. The total number of funding years associated with these clusters is shown in Table 2.
Table 2.
Funding years contributing to first-in-class products discovered through targeted or phenotypic methods
| Metrics | Drug | Target only | Total |
| Funding years | |||
| All | 12,840 | 184,015 | 196,855 |
| Targeted | 9,170 | 166,970 | 176,140 |
| Phenotypic | 3,670 | 17,045 | 20,715 |
| Funding years per NME | |||
| All, n = 87 (%) | 167 (7) | 2,390 (93) | 2,557 |
| Targeted, n = 77 (%) | 137 (5) | 2,492 (95) | 2,629 |
| Phenotypic, n = 10 (%) | 367 (18) | 1,704 (82) | 2,071 |
-
Funding years associated with multiple NMEs are not unique.
The time course of funding years leading to approval of a first-in-class NME discovered through targeted or phenotypic methods is shown in Fig. 2A. The relative proportion of funding years directly related to targets is shown in Fig. 2B for products discovered through targeted screening and phenotypic methods. These data show that for first-in-class products, a larger fraction of the funding years was associated with target only and that this fraction dropped in the years immediately before approval. Overall, for first-in-class NMEs discovered through targeted screening, 95% of funding years were classified as “target only,” and 5% were classified as “drug,” while for those discovered by phenotypic methods 82% were classified as “target only,” and 18% were classified as “drug.”
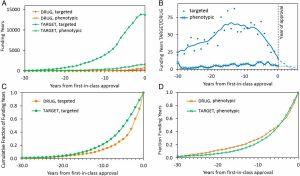
NIH funding years associated with research on first-in-class products (2010–2016). Data are normalized to the year of first FDA approval. (A) Funding years directly related to NMEs (drug) or their molecular target (target). Data are shown for research leading to first-in-class NMEs discovered by targeted or phenotypic methods. (B) Ratio of funding years directly related to drugs or targets for first-in-class NMEs discovered by targeted or phenotypic methods. Data after the year of first approval are shown as dashed lines. (C) Timeline of funding years related to the NME (drug, targeted) or the molecular target (target, targeted) for first-in-class drugs discovered by targeted screening. (D) Timeline of funding years related to the NME (drug, phenotypic) or the molecular target (target, phenotypic) for first-in-class drugs discovered with phenotypic methods.
For first-in-class NMEs discovered through targeted methods, the accumulation of funding years directly related to targets precedes the accumulation of funding years directly related to the drugs (Fig. 2C). This result is consistent with the fact that targeted discovery is predicated on knowledge of the target and proposed therapeutic mechanism. A distinctly different pattern is evident for first-in-class NMEs discovered using phenotypic methods, where the accumulation of funding years directly related to drugs precedes the accumulation of funding years directly related to targets. This result is similarly consistent with the fact that the targets for phenotypic drugs are often unknown or incompletely characterized at the time of drug discovery.
Discussion
This study provides a perspective on the scale of the public-sector contribution to the discovery and development of new drugs. We identified NIH-funded publications and projects directly related to all the 210 NMEs approved by the FDA from 2010–2016 or their molecular targets. This research comprised more than 200,000 funding years and project costs totaling more than $100 billion.
This analysis paints a more expansive picture of the public sector’s contribution to new drug discovery and development than previous studies. Previous studies showed that 6–10% of NMEs were first patented by the public sector and academic institutions (11, 16, 18⇓–20), that as many as half of the patents on new drugs cite prior art produced in the public sector (20, 21), and that up to 40% of the new molecular entities were first synthesized or purified in academic institutions (22). Case studies have identified a public-sector contribution to the basic or applied science underlying 50–75% of new drugs (5, 6, 23).
The differences in our findings likely relate to the use of a method designed to capture the contribution of basic research or use-inspired basic research as well as applied research. Both the NIH and National Science Foundation (NSF) define basic research as being undertaken “without specific applications towards processes or products in mind” (44, 45). Our analysis focuses on published research, which is the primary deliverable for NIH-funded basic research.
In contrast, studies based on drug patents are explicitly limited to contributions that meet legal standards for patentability. In the United States, these standards require inventors to establish that their inventions are both “new and useful” according to 35 USC 101 (46, 47). In the European Union, European Patent Office standards require inventors to establish that their invention is “susceptible of industrial application” according to EPC Article 52 and Article 57 (48). Thus, while there is often considerable latitude in the interpretation of these standards, patent-based analyses are implicitly biased in favor of applied research with specific processes or product applications. Studies have shown, in fact, that patent analysis is a poor measure of knowledge flow from public institutions or funding (49, 50). Case-study methods are more likely to recognize the contributions of basic science or “fundamental scientific knowledge” (23) but may be similarly biased in favor of research that is linked to a specific process or product. Thus, the methods used in previous studies may have systematically underestimated the contribution of basic research to new drug approvals.
In underestimating the scope of basic research, previous studies may have also underestimated the contribution of public funding, specifically funding from the NIH. The NIH has traditionally prioritized funding for investigator-initiated basic research (51, 52) and continues to direct more than half of its funding to basic, as opposed to applied, research (53). The finding that more than 90% of the publications citing NIH support appeared in PubMed searches for the targets of newly approved drugs, but not in searches for the drugs themselves, suggests that this research was not focused on specific processes or products to the extent that this association would be identified in the title, abstract, or PubMed medical subject headings (MeSH terms). Thus, most of these publications likely represent basic research.
This study does not attempt to identify publications that describe seminal inventions or milestones in drug discovery or development. Rather, this work posits that the corpus of published research, taken as a whole, reflects the advancing forefront of knowledge from which new drugs are discovered and developed. This approach builds on an increasing body of scholarship that views innovation not as the end product of a discrete sequence of insights or inventions but as an outgrowth of extensive knowledge networks, social networks, and intersecting communities in an ecosystem that both generates and applies new knowledge (4, 54, 55). Consistent with this view, our previous work has shown that metrics of research growth based on the accumulation of publications are strongly associated with successful development of targeted and biological NMEs (26, 28).
These data demonstrate that a sizable public-sector investment occurs before the approval of first-in-class NMEs, particularly those discovered using targeted discovery methods (including recombinant biologicals). The scale of this investment can be estimated from the costs associated with first-in-class NMEs approved in 2010–2016 and their molecular targets (Table 3). These data suggest that the public-sector investment in research underlying each first-in-class drug is as high as $839 million, with 89% of this cost associated with target research and 11% of the cost associated with the first-in-class compound or follow-on compounds approved from 2010–2016.
Table 3.
Costs contributing to first-in-class NMEs approved 2010–2016
| Metrics | Drug | Target | Total |
| Costs, million $, 2016 | 7,039 | 57,586 | 64,625 |
| Costs per NME, million $, 2016 | 91 | 748 | 839 |
This estimate of public-sector contribution to first-in-class products should not be interpreted as a per-drug investment. Since most of the public-sector funding we identified is associated with research on molecular targets, rather than specific NMEs, this funding may contribute not only to the first-in-class NME approved from 2010–2016 but also to follow-on products in the same class. It is also likely that basic research on drug targets has spillover effects that could lead to new classes of products that are not yet anticipated as well as to new diagnostics, devices, or approaches to disease management.
Overall, this analysis suggests that as much as 20% of the NIH budget allocation from 2000–2016 was associated with published research that directly or indirectly contributed to NMEs approved from 2010–2016. This fraction does not include research that contributed to drugs approved before 2010 or drugs currently in development that may emerge in years to come. Thus, while the NIH may continue to emphasize basic or use-inspired basic research arising from investigator-driven initiatives (56), this analysis shows that a substantial fraction of NIH spending is contributing directly or indirectly to new therapies for disease.
There are several significant limitations to the methods utilized in this analysis. First, PubMed searches identify papers by the content of the title, abstract, and metadata, including MeSH terms, but may fail to identify research published before its relevance to a specific target or NME is recognized. Our method also does not identify research on enabling technologies, such as new analytical or genomic technologies, with broad applications in biomedical research or research focused generally on mechanisms or outcomes of disease. Second, we encountered numerous mismatches between the funding years inferred from the Link database in RePORTER and the actual fiscal years of funded projects. Related problems have been noted by others who describe false-positive matches between publications and grants as well as false negatives in which grant information was not indexed within articles (42). Many mismatches involved publications with dates after the last year of grant funding. Based on the observations of Boyack and Jordan (42), who estimated a 3-y lag between publication dates and entries in RePORTER, we associated the costs associated with the final year of the project with research published 1–4 y after the end of the project. With this correction, we were able to associate costs with 86.3% of funding years from 2000–2016. Possible explanations for mismatches between the other 13.7% of funding years and fiscal years of projects include errors in acknowledging specific projects or errors in data curation. These experimental limitations would tend to underestimate the magnitude of NIH funding for research related these products and should be considered lower bounds (42). Third, this analysis does not account for research funding from government agencies, such as the Department of Defense or NSF, or other nations, which are not represented in the RePORTER database, and does not include research funding from other public-sector sources, such as academic institutions or philanthropies. A recent report estimated that 30% of nonindustrial medical and health research and development (R&D) was funded by universities, research institutes, or foundations (57). Thus, these results do not reflect the full public-sector contribution to research underlying NME approvals over this interval but predominantly reflect the contribution made by NIH funding.
This work demonstrates that NIH funding was associated directly or indirectly with every drug approved from 2010–2016 and suggests that the scale of this contribution is larger than generally appreciated. This contribution primarily involved funding for research related to molecular targets for new drugs and likely represents basic research or use-inspired basic research, as opposed to applied research. These data are consistent with the classic expectation that the public sector’s contribution to translational science primarily involves basic science or use-inspired basic science, which enables subsequent development and commercialization of new products in the private sector.
It is important to appreciate the scope of the public sector’s investment in the ecosystem for new drug discovery and development in light of proposals to cut allocations to the NIH and NSF (58) as well as the diminution of science’s role throughout government (59). The magnitude of this contribution to the science underlying recently approved drugs cannot be effectively made up by philanthropy or investment or by academic or advocacy organizations. Initiatives to reduce waste and improve the efficiency of biomedical research (60⇓–62), while necessary, are also unlikely to make up for any substantial shortfall in funding. Moreover, it is unlikely that any shortfall would be rectified by the biopharmaceutical industry, given the long-term trend toward decreasing corporate investment in basic research (63), as well as the limited incentives for companies to make investments toward basic research that would negatively impact near-term earnings, offer uncertain competitive advantage, and may not generate profitable products for decades.
This work underscores the breath and significance of public investment in the development of new therapeutics and the risk that reduced research funding would slow the pipeline for treating morbid disease. The science community has long recognized the importance of basic research as the engine of an innovation ecosystem (51, 52). We are currently witnessing the emergence of exciting new products associated with targets identified through basic research in areas such as genomics, gene expression, protein trafficking, cell cycle, apoptosis, patterns of differentiation, and mechanisms of the immune response. Our previous studies demonstrate that the time required for this basic research to mature to the point necessary for successful development represents the most prolonged stage of the translational process (26, 28). This work shows that a large fraction of the NIH research budget is focused on the basic research required to bring new products to market. Any reduction in this funding that slows the pace of this research could significantly delay the emergence of new drugs in the future.
Acknowledgments
This project benefited from discussions with Drs. Michael Kinch and Rebekah Griesenauer at Washington University, St. Louis and Dr. Robert Kneller at University of Tokyo, the analytical expertise of Drs. Michael Walsh, Christopher Bresten, and David Oury at the Center for Integration of Science and Industry, the constructive comments of Drs. Michael Boss and Nancy Hsiung, and the assistance of Danielle Solar in preparation of the manuscript. This work was supported by a grant from the National Biomedical Research Foundation.
Footnotes
↵1To whom correspondence should be addressed. Email: fledley@bentley.edu.
Author contributions: E.G.C., J.M.B., L.M.M., and F.D.L. designed research; E.G.C., J.M.B., N.S.K., L.M.M., and F.D.L. performed research; E.G.C., J.M.B., N.S.K., and F.D.L. analyzed data; and E.G.C. and F.D.L. wrote the paper.
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1715368115/-/DCSupplemental.
Copyright © 2018 the Author(s). Published by PNAS.
This open access article is distributed under Creative Commons Attribution-NonCommercial-NoDerivatives License 4.0 (CC BY-NC-ND).
References
- Stokes DE (2011) Pasteur’s Quadrant: Basic Science and Technological Innovation (Brookings Institute, Washington, DC)
- Collins FS (2011) Reengineering translational science: The time is right. Sci Transl Med 3:90cm17
- Moses H 3rd, et al. (2015) The anatomy of medical research: US and international comparisons. JAMA 313:174–189
- Cockburn I, Henderson R (1996) Public-private interaction in pharmaceutical research. Proc Natl Acad Sci USA 93:12725–12730
- Zycher B, DiMasi JA, Milne C-P (2010) Private sector contributions to pharmaceutical science: Thirty-five summary case histories. Am J Ther 17:101–120
- Chakravarthy R, Cotter K, DiMasi J, Milne C-P, Wendel N (2016) Public-and private-sector contributions to the research and development of the most transformational drugs in the past 25 years: From theory to therapy. Ther Innov Regul Sci 50:759–768
- Reichert JM, Milne C-P (2002) Public and private sector contributions to the discovery and development of “impact” drugs. Am J Ther 9:543–555
- Varmus H (2006) The new era in cancer research. Science 312:1162–1165
- Woodcock J, Brumfield M, Gill D, Zerhouni E (2014) The driving role of consortia on the critical path to innovative therapies. Nat Rev Drug Discov 13:781–782
- DiMasi JA, Grabowski HG, Hansen RW (2016) Innovation in the pharmaceutical industry: New estimates of R&D costs. J Health Econ 47:20–33
- DiMasi JA, Hansen RW, Grabowski HG (2003) The price of innovation: New estimates of drug development costs. J Health Econ 22:151–185
- Munos B (2009) Lessons from 60 years of pharmaceutical innovation. Nat Rev Drug Discov 8:959–968
- Scannell JW, Blanckley A, Boldon H, Warrington B (2012) Diagnosing the decline in pharmaceutical R&D efficiency. Nat Rev Drug Discov 11:191–200
- DiMasi JA, Grabowski HG (2007) The cost of biopharmaceutical R&D: Is biotech different? Manage Decis Econ 28:469–479
- DiMasi JA, Grabowski HG, Vernon J (2004) R&D costs and returns by therapeutic category. Drug Inf J 38:211–223
- Stevens AJ, et al. (2011) The role of public-sector research in the discovery of drugs and vaccines. N Engl J Med 364:535–541
- US Food & Drug Administration (2017) Orange Book: Approved Drug Products with Therapeutic Equivalence Evaluations. Available at https://www.accessdata.fda.gov/scripts/cder/ob/. Accessed April 12, 2017
- Kaitin KI, Bryant NR, Lasagna L (1993) The role of the research-based pharmaceutical industry in medical progress in the United States. J Clin Pharmacol 33:412–417
- Sampat BN (2009) Academic patents and access to medicines in developing countries. Am J Public Health 99:9–17
- Sampat BN, Lichtenberg FR (2011) What are the respective roles of the public and private sectors in pharmaceutical innovation? Health Aff (Millwood) 30:332–339
- Kneller R (2010) The importance of new companies for drug discovery: Origins of a decade of new drugs. Nat Rev Drug Discov 9:867–882
- Patridge EV, Gareiss PC, Kinch MS, Hoyer DW (2015) An analysis of original research contributions toward FDA-approved drugs. Drug Discov Today 20:1182–1187
- Cockburn IM, Henderson RM (2000) Publicly funded science and the productivity of the pharmaceutical industry. Innov Policy Econ 1:1–34
- McNamee LM, Walsh MJ, Ledley FD (2017) Timelines of translational science: From technology initiation to FDA approval. PLoS One 12:e0177371
- McNamee LM, Ledley FD (2012) Patterns of technological innovation in biotech. Nat Biotechnol 30:937–943
- Beierlein JM, et al. (2017) Landscape of innovation for cardiovascular pharmaceuticals: From basic science to new molecular entities. Clin Ther 39:1409–1425.e20
- Beierlein JM, McNamee LM, Walsh MJ, Ledley FD (2015) Patterns of innovation in Alzheimer’s disease drug development: A strategic assessment based on technological maturity. Clin Ther 37:1643–51.e3
- McNamee LM, Ledley FD (2017) Modeling timelines for translational science in cancer; the impact of technological maturation. PLoS One 12:e0174538
- Swinney DC (2013) Phenotypic vs. target-based drug discovery for first-in-class medicines. Clin Pharmacol Ther 93:299–301
- Swinney DC, Anthony J (2011) How were new medicines discovered? Nat Rev Drug Discov 10:507–519
- Drews J (2000) Drug discovery: A historical perspective. Science 287:1960–1964
- Gibbs JB (2000) Mechanism-based target identification and drug discovery in cancer research. Science 287:1969–1973
- Gabor Miklos GL (2005) The human cancer genome project–One more misstep in the war on cancer. Nat Biotechnol 23:535–537
- Kotz J (2012) Phenotypic screening, take two. Sci Bus Exch doi:10.1038/scibx.2012.380
- US Food & Drug Administration (2017) New molecular entity (NME) drug and new biologic approvals. Available at https://www.fda.gov/Drugs/DevelopmentApprovalProcess/HowDrugsareDevelopedandApproved/DrugandBiologicApprovalReports/NDAandBLAApprovalReports/ucm373420.htm. Accessed April 12, 2017
- US Food & Drug Administration (2017) New drugs at FDA: CDER’s new molecular entities and new therapeutic biological products. Available at https://www.fda.gov/Drugs/DevelopmentApprovalProcess/DrugInnovation/default.htm. Accessed April 12, 2017
- US Food & Drug Administration (2017) FDA online label repository. Available at https://labels.fda.gov/. Accessed April 12, 2017
- EMBL-EBI (2017) ChEMBL. Available at https://www.ebi.ac.uk/chembl/. Accessed April 12, 2017
- National Institutes of Health (2017) Research portfolio online reporting tools (RePORTER), ExPORTER data catalog. Available at https://exporter.nih.gov/ExPORTER_Catalog.aspx. Accessed April 12, 2017
- United States Department of Labor (2017) Bureau of labor statistics: CPI-All urban consumers (current series). Available at: https://data.bls.gov/timeseries/CUUR0000SA0. Accessed April 12, 2017
- Xu Q, Boggio A, Ballabeni A (2014) Countries’ biomedical publications and attraction scores. A PubMed-based assessment. F1000 Res 3:292
- Boyack KW, Jordan P (2011) Metrics associated with NIH funding: A high-level view. J Am Med Inform Assoc 18:423–431
- National Institutes of Health (2009) NIH’s role in the American recovery and reinvestment Act (ARRA). Available at https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nihs-role-american-recovery-reinvestment-act-arra. Accessed April 12, 2017
- Collins FS (2012) NIH basics. Science 337:503
- National Research Council (2005) Assessment of Department of Defense Basic Research (The National Academies, Washington, DC), p 70
- Legal Information Institute (1952) 35 US Code § 101– Inventions patentable. Code of Federal Regulations. Available at https://www.law.cornell.edu/uscode/text/35/101. Accessed April 12, 2017
- United States Patent and Trademark Office (2017) Guidelines for examination of applications for compliance with the utility requirement [R-11.2013]. Available at https://www.uspto.gov/web/offices/pac/mpep/s2107.html. Accessed April 12, 2017
- European Patent Office (2017) Convention on the grant of European patents, article 52 – Patentable inventions. Available at www.epo.org/law-practice/legal-texts/html/epc/2016/e/ar52.html. Accessed April 12, 2017
- Pavitt K (1998) Do patents reflect the useful research output of universities? Res Eval 7:105–111
- Roach M, Cohen WM (2013) Lens or prism? Patent citations as a measure of knowledge flows from public research. Manage Sci 59:504–525
- Bishop JM, Kirschner M, Varmus H (1993) Science and the new administration. Science 259:444–445
- Kornberg A (1997) The NIH did it! Science 278:1863
- Lauer M (2016) NIH’s commitment to basic science. Extramural Nexus. Available at https://nexus.od.nih.gov/all/2016/03/25/nihs-commitment-to-basic-science/. Accessed April 12, 2017
- Santos FM (2003) The coevolution of firms and their knowledge environment: Insights from the pharmaceutical industry. Technol Forecast Soc Change 70:687–715
- Enkel E, Gassmann O, Chesbrough H (2009) Open R&D and open innovation: Exploring the phenomenon. R & D Manag 39:311–316
- Sampat BN (2012) Mission-oriented biomedical research at the NIH. Res Policy 41:1729–1741
- Research America (2016) US investments in medical and health research and development, 2013-2015. Available at https://www.researchamerica.org/sites/default/files/2016US_Invest_R%26D_report.pdf. Accessed April 12, 2017
- Reardon S, Tollefson J, Witze A, Ross E (2017) Trump budget would slash science programmes across government. Nature 546:19–20
- Matthews KR, Evans KM, Lane NF (2017) Science advice in the trump white house. Science 355:574–576
- Ioannidis JP, et al. (2014) Increasing value and reducing waste in research design, conduct, and analysis. Lancet 383:166–175
- Chalmers I, et al. (2014) How to increase value and reduce waste when research priorities are set. Lancet 383:156–165
- Ioannidis JP (2014) How to make more published research true. PLoS Med 11:e1001747
- Arora A, Belenzon S, Patacconi A (2015) Killing the golden goose? The decline of science in corporate R&D (National Bureau of Economic Research). Available at www.nber.org/papers/w20902. Accessed April 12, 2017