Understanding the Fundamentals of Pharmaceutical Pricing
Drug pricing extends beyond a mere monetary exchange; it serves as a critical nexus within the intricate healthcare ecosystem. It influences the accessibility of essential treatments for patients, the financial stability of pharmaceutical companies that fuels future medical advancements, the operational capacities of healthcare providers, and the fiscal responsibilities of governmental bodies. The determination of a pharmaceutical product’s price involves a complex interplay of numerous factors, demanding a comprehensive understanding for any business professional aiming for market leadership.1
Setting the price of a pharmaceutical product is a multifaceted process that necessitates careful consideration of various elements. Different pricing strategies are employed within the industry, each with its own underlying logic and applicability. These strategies can range from models based on the volume of products sold to those that consider the perceived value of the treatment. Market-based pricing, for instance, involves setting prices in accordance with what competitors charge for similar products, a common tactic for smaller to medium-sized pharmaceutical companies. Value-based pricing, on the other hand, anchors the price to the drug’s perceived effectiveness and the benefits it offers. Cost-based pricing calculates the price based on the expenses incurred during production, a method often favored by generic drug manufacturers.1 The overarching goal of these diverse pricing models is to ensure that patients have access to medications they need while simultaneously generating revenue for the pharmaceutical industry to sustain operations and innovation.2 The emergence of new technologies for patient monitoring and data collection has also facilitated the use of innovative payment models, further diversifying the landscape of pharmaceutical pricing strategies.3
The methods employed to determine drug prices exhibit significant variation across the globe. Different nations have adopted distinct approaches, reflecting their unique healthcare systems, economic landscapes, and societal values. Certain countries implement stringent government regulations and engage in direct negotiations with pharmaceutical companies to control prices. Conversely, others favor market-driven mechanisms with varying degrees of governmental oversight. This global diversity underscores the absence of a one-size-fits-all solution to pharmaceutical pricing.2
For example, many countries utilize International Reference Pricing (IRP), where the price of a drug is set based on its price in other countries.4 A comparison across several nations reveals the diverse tools in use, including cost-based pricing, Health Technology Assessment (HTA), and informal IRP.4 Reports consistently indicate that the United States generally incurs substantially higher costs for prescription drugs, particularly for brand-name medications, when compared to other member countries of the Organisation for Economic Co-operation and Development (OECD).5 This significant price disparity, especially the elevated prices in the U.S. for branded drugs, presents both challenges and opportunities for businesses engaged in the global pharmaceutical market. A thorough understanding of these international differences is paramount for crafting effective pricing and market access strategies tailored to specific geographical regions. A company introducing a new drug might encounter vastly different pricing pressures and negotiation environments in the U.S. compared to a country like Canada or Germany. Therefore, business professionals must meticulously analyze these variations to optimize their global pricing strategies, ensuring profitability while maintaining market access.
Exploring the Spectrum of Drug Pricing Models
Value-Based Pricing: Linking Cost to Therapeutic Benefit
At its core, value-based pricing represents a fundamental shift in perspective, moving away from pricing based on the quantity of drugs sold towards a model that aligns cost with the actual health improvements and value delivered to patients and the broader healthcare system.1 Under this model, the price of a drug is established by carefully evaluating its effectiveness in treating a specific condition, its safety profile in comparison to existing treatment options, the extent to which it enhances patients’ quality of life, and its potential to generate cost savings within the healthcare system, such as through reducing hospital readmissions.1 This approach is frequently adopted by innovative pharmaceutical companies that have developed novel therapies demonstrating significant advantages over existing treatments.1
One of the primary advantages of value-based pricing lies in its potential to broaden patient access to groundbreaking and highly effective therapies.3 By linking payment to tangible improvements in health outcomes, these pricing models can make innovative treatments more readily available to those who stand to benefit most. Furthermore, value-based pricing can enhance affordability by mitigating the financial risks typically associated with high-cost treatments.3 Models like the mortgage model, a variation of value-based pricing, further contribute to affordability by allowing purchasers to distribute the expense of costly therapies over an extended period. This approach also fosters a stronger alignment between a drug’s price and its real-world performance, creating an incentive for the development of medications that offer genuine and substantial therapeutic advantages.3 The increasing sophistication of technology for monitoring patients and gathering comprehensive health data has further facilitated the implementation and expansion of value-based contracting and other innovative payment models within the pharmaceutical industry.3
However, the implementation of value-based pricing is not without its complexities. One significant hurdle involves the challenges associated with data sharing between the various stakeholders within the healthcare ecosystem.3 Effectively executing value-based contracts necessitates a seamless flow of information, which can be difficult to achieve given the fragmented nature of many healthcare systems. Moreover, the operational aspects of establishing and managing these often intricate agreements can present considerable logistical challenges.3 In many therapeutic areas, there may be a lack of clearly defined and easily measurable biological outcomes that can serve as reliable indicators of a drug’s performance.3 Factors related to patient behavior, such as adherence to treatment plans, can also influence outcomes in ways that are independent of the drug’s inherent efficacy, making it challenging to solely attribute results to the medication itself.3 Navigating the diverse and sometimes conflicting value assessment frameworks that exist across different global markets adds another layer of complexity for pharmaceutical companies seeking to implement value-based pricing strategies on an international scale.3
Value-based pricing, where the price of a pharmaceutical product is set based on its perceived value, is often used by innovative companies with new products.1 This strategy centers on the clinical benefit and value the drug provides to patients and the healthcare system.1 Financial risk-based contracts and health outcomes contracts are key types of value-based agreements, designed to link price to real-world performance.3 These contracts are gaining traction, especially for innovative specialty drugs and orphan products.3 The advantages include improved patient access and enhanced affordability.3 However, challenges persist in data sharing and operational hurdles.3
While value-based pricing offers a promising pathway to ensure that drug costs are justified by the tangible benefits they provide to patients and the healthcare system, its widespread adoption hinges on overcoming significant obstacles. These challenges relate to establishing robust data infrastructure, streamlining operational processes, and addressing the inherent complexities of accurately measuring and attributing value in real-world clinical settings. Businesses that can develop innovative solutions to these challenges will be well-positioned to thrive in a healthcare landscape that increasingly prioritizes value and outcomes. The successful implementation of value-based contracts requires the establishment of robust systems for the collection, secure sharing, and sophisticated analysis of patient data across different healthcare settings. Pharmaceutical companies must foster collaborative relationships with payers and healthcare providers to clearly define meaningful outcomes and develop appropriate metrics for assessing the value of their therapies. Business professionals who possess the expertise to facilitate this crucial collaboration and provide the necessary technological infrastructure will play an indispensable role in driving the broader adoption of value-based pricing models within the pharmaceutical industry.
Cost-Plus Pricing: Transparency and Profit Margins
Cost-plus pricing represents a relatively straightforward and transparent approach to determining the price of a pharmaceutical drug. In this model, the price is calculated by first summing up the total costs associated with producing the drug. These costs encompass a wide range of expenditures, including the raw materials required for manufacturing, the direct costs of the manufacturing process itself, the often substantial investments in research and development, the expenses related to navigating the complex regulatory approval process, and other operational overheads.2 Once the total cost of production is accurately determined, a predetermined percentage markup is then added to this figure. This markup represents the desired profit margin for the pharmaceutical company, ensuring that the sale of the drug not only covers all associated costs but also generates a profit.2 The fundamental principle underlying cost-plus pricing is to guarantee that all expenses incurred in bringing the drug to market are fully recovered while also securing a consistent level of profitability for each unit sold.
One of the primary benefits of cost-plus pricing lies in its inherent simplicity and the ease with which it can be calculated.13 Unlike more complex pricing models that require extensive market research and analysis, cost-plus pricing primarily relies on internal cost data, which is typically readily available to the pharmaceutical company. This model provides a clear and transparent understanding of the minimum price point required to cover all costs associated with the drug’s production and ensures a consistent rate of return on investment, making it a predictable and reliable method for financial planning and forecasting.13 Cost-plus pricing can be particularly advantageous in situations where there is limited information available about the market, such as when introducing a truly novel drug with no direct competitors, or in cases involving customized or unique pharmaceutical products where obtaining reliable competitor pricing data might be challenging.13 Furthermore, this model offers the assurance of full cost coverage, significantly reducing the risk of selling the drug at a price that is below the actual cost of its production.14
Despite its apparent simplicity, cost-plus pricing has notable limitations, particularly within the highly dynamic and value-driven pharmaceutical industry. A significant drawback is that it largely disregards the crucial factors of market demand and the perceived value of the drug from the perspective of both patients and the broader healthcare system.12 By primarily focusing on the internal costs of production, cost-plus pricing fails to adequately consider what customers might be willing to pay based on the drug’s therapeutic benefits, its potential to improve health outcomes, or the prices of alternative and competing therapies available in the market.15 This inherent limitation can lead to suboptimal pricing decisions. In some instances, the drug might be underpriced, resulting in a loss of potential revenue that could have been captured if the pricing had been more aligned with its perceived value. Conversely, the drug could be overpriced relative to its competitors or its perceived benefits, potentially hindering market access, limiting its adoption by patients and healthcare providers, and ultimately impacting sales volume.15 Moreover, cost-plus pricing does not inherently incentivize pharmaceutical companies to pursue efficiency improvements in their production processes. Since higher costs directly translate to higher prices under this model, there is less motivation to actively seek out ways to reduce expenses.17 In a competitive market environment, relying solely on a cost-plus pricing strategy can leave a company vulnerable to competitors who adopt more market-sensitive pricing approaches that better reflect customer willingness to pay and the competitive landscape.15
Cost-plus pricing is a straightforward method where price equals the cost of production plus a profit margin.2 While simple, it doesn’t account for market demand or perceived value.12 Advantages include simplicity and ensuring cost recovery.13 Disadvantages include ignoring market demand and potentially leading to under- or overpricing.15
While cost-plus pricing offers the benefits of transparency and ensures that the basic costs of drug production are covered, its fundamental neglect of market dynamics and value considerations renders it a less sophisticated strategy for maximizing profitability and ensuring broad market access in the complex pharmaceutical arena. However, the transparency inherent in this model can be particularly valuable for initiatives centered on enhancing drug affordability and containing healthcare costs, as exemplified by the Mark Cuban Cost Plus Drug Company.18 In a market increasingly driven by innovation and the perceived value of therapeutic interventions, pharmaceutical companies require pricing strategies that effectively capture these critical factors. Cost-plus pricing, by its singular focus on internal production costs, may fail to recognize the true worth of a breakthrough therapy or allow for effective competitive positioning based on prevailing market conditions. Business professionals should view cost-plus pricing as a foundational element but actively explore more dynamic and value-oriented pricing models to make optimal pricing decisions that balance profitability with market access and patient needs.
Competitive-Based Pricing: Navigating Market Dynamics
Competitive-based pricing, often referred to as market-based pricing, is a strategic approach where pharmaceutical companies primarily determine the prices of their drugs by closely monitoring and responding to the prices established by competitors for similar or alternative products already available in the market.1 The fundamental principle guiding this strategy is to align a company’s prices with the prevailing market rates to maintain a competitive edge and effectively attract customers. This often involves setting the price of a particular drug at a level comparable to those of its direct competitors. However, companies might also make adjustments to their prices based on their perception of their product’s differentiation, such as offering superior efficacy or fewer side effects, or based on their desired market positioning, aiming to be either a price leader or a value provider.
One of the primary advantages of competitive pricing is its relative simplicity and straightforward implementation.22 It allows companies to swiftly enter a market by adopting a price point that is already considered acceptable and normalized by customers and payers, as it is based on the established prices of existing competitors.22 This strategy proves particularly effective in highly competitive markets where the available products are perceived as largely interchangeable by consumers, or in situations where customers exhibit a high degree of price sensitivity.22 By offering prices that are lower than those of their rivals, companies can potentially achieve several key benefits, including an increase in overall sales volume, the cultivation of stronger brand loyalty among price-conscious customers, and ultimately, an expansion of their market share.22 Furthermore, competitive pricing can be a valuable tool for new brands entering a market, as it negates the need for extensive and potentially costly market research by allowing them to leverage the pricing analysis already conducted by established competitors.22
However, a significant drawback of relying too heavily on competitive pricing is that it can lead to missed opportunities for maximizing profits, especially if a company’s product offers unique features, superior efficacy, or other differentiating factors that would justify a higher price point.15 This strategy also operates under the assumption that competitors have correctly priced their own products, which may not always be the case due to various factors such as differing cost structures or strategic objectives.24 A purely competitive approach may also overlook the specific needs and concerns of customers, as well as their willingness to pay a premium for a drug that offers demonstrably better outcomes or a more favorable side effect profile.16 Moreover, an excessive focus on matching or undercutting competitor prices can lead to a short-term orientation, potentially eroding profit margins over time and even devaluing the product in the eyes of consumers who might equate lower prices with lower quality.23 Finally, a purely competitive strategy does not inherently incentivize innovation or the effective communication of a product’s unique benefits, as the primary emphasis remains on achieving price parity or a slight price advantage over the competition.16
Competitive-based pricing sets drug prices based on competitor prices.1 It’s common for smaller companies.1 Advantages include simplicity and quick market entry.22 Disadvantages include potentially missing profit opportunities and neglecting customer value.15
While competitive pricing offers a practical route for entering a market and maintaining a competitive stance, particularly for generic drugs or those in crowded therapeutic categories, businesses should exercise caution in making it their sole pricing strategy. To achieve optimal profitability and cultivate a strong brand presence, companies need to also consider the unique value propositions of their products and adopt pricing models that accurately reflect this value, rather than simply mirroring the prices of their competitors. A balanced approach that thoughtfully integrates both a thorough analysis of the competitive landscape and a deep understanding of the value offered to patients is often the most effective way to navigate the complexities of market dynamics and achieve sustainable success. In the pharmaceutical industry, where the level of innovation and therapeutic efficacy can vary considerably among competing drugs, a singular focus on price can be counterproductive. Companies that have developed superior products or those with distinct advantages should leverage value-based messaging and pricing strategies to effectively capture the willingness of both patients and payers to pay a premium for enhanced health outcomes. Conversely, for more commoditized products, such as generic medications, competitive pricing will likely continue to be a dominant factor in market success. Business professionals must carefully assess where their products lie on this spectrum and tailor their pricing strategies accordingly to maximize their competitive advantage and achieve their strategic objectives.
Other Influential Pricing Models
Market-Based Pricing
Similar to competitive-based pricing, market-based pricing considers the prevailing conditions within the market, including the overall levels of supply and demand for a specific type of drug or treatment.1 Companies that adopt this approach will analyze what customers are generally willing to pay for a medication within a particular therapeutic area. This model often works in conjunction with a thorough analysis of competitor pricing, but it may also take into account broader economic factors, such as inflation rates and the overall economic health of the region, as well as the affordability of medications for patients in different markets.
Market-based pricing considers the prices of similar products on the market.1
Reference Pricing: Benchmarking Against Other Nations
Reference pricing involves establishing the price of a pharmaceutical drug in one country by comparing it to the price of the same or similar drugs in one or more other countries.2 This approach is frequently utilized by governments and health insurance providers as a mechanism to negotiate lower prices, particularly for brand-name medications that may lack significant competition within a specific market. The “reference” countries selected for comparison are typically those that share similar levels of economic development and have comparable healthcare systems. For instance, the International Pricing Index (IPI) model 30, which was proposed in the United States, aimed to align the payments made by Medicare for certain drugs with the prices paid for those same drugs in foreign countries.
Reference pricing sets drug prices based on prices in other countries.2 The proposed IPI model aimed to align US Medicare payments with international prices.30
International reference pricing stands as a significant policy instrument that is currently being considered and implemented in various forms as a strategy to address the issue of high drug prices, especially in countries like the United States where the cost of pharmaceuticals is notably higher than in comparable nations. Businesses that operate on a global scale need to be keenly aware of these evolving policies and understand their potential ramifications on their pricing strategies and their ability to access different markets. If a country adopts a reference pricing policy, a pharmaceutical company might be compelled to lower the price of its drug to align with the average or the lowest price observed in a selected group of reference countries. This could have a substantial impact on the company’s revenue projections and overall profitability, thereby necessitating a careful re-evaluation of its global pricing strategies.
Subscription and Indication-Specific Models
Subscription models, sometimes likened to the “Netflix model” for accessing content, involve payers, such as government agencies or insurance companies, remitting a fixed annual fee to a pharmaceutical company. In return, these payers gain unlimited access to a specific drug or a range of drugs for a defined population of patients.12 This model has been explored as a potential solution for curative therapies, such as those for Hepatitis C.12 Indication-specific pricing, on the other hand, involves setting different prices for the same drug depending on the specific disease or medical condition that it is approved to treat.12 This approach acknowledges that the therapeutic value of a drug can vary significantly depending on its effectiveness in treating different indications.
Subscription models involve a fixed fee for unlimited access.12 Indication-specific pricing sets different prices for the same drug for different conditions.12
These alternative pricing models are gaining momentum as potential solutions for enhancing patient access to costly, innovative therapies and for better aligning drug prices with the specific value they offer for different medical uses. Businesses should carefully consider the applicability of these models, particularly for novel therapies or for drugs that have received approval for multiple distinct indications. For a curative therapy, a subscription model can offer budget predictability for payers and ensure broad access for patients without the constraints of per-patient costs. For a drug with multiple approved uses, indication-specific pricing allows the manufacturer to charge a price that more accurately reflects the value provided for each specific indication, potentially maximizing overall revenue while maintaining affordability for less critical uses.
PBM Pricing Models: Spread vs. Pass-Through
In the United States, Pharmacy Benefit Managers (PBMs) play a pivotal role in managing prescription drug benefits on behalf of health plans, employers, and other payers. Two primary pricing models employed by PBMs are traditional (spread) pricing and transparent (pass-through) pricing.32 Under the traditional spread pricing model, the PBM negotiates discounts and rebates with drug manufacturers and pharmacies. However, the PBM then charges its clients a negotiated price for prescription drugs while paying the pharmacy a different, typically lower, price. The difference between what the PBM charges its client and what it pays the pharmacy is known as the “spread,” and this spread represents a significant source of profit for the PBM.32 In contrast, the transparent pass-through pricing model offers greater visibility into the actual costs associated with managing pharmacy benefits. With this model, PBMs pass on all discounts, rebates, and fees received from drug manufacturers and pharmacies directly to their clients, effectively eliminating the profit “spread” that is characteristic of the traditional model. Transparent PBMs primarily generate revenue by charging their clients a separate, fixed administrative fee for the services they provide on each prescription claim.32
Traditional PBM pricing involves the PBM profiting from the “spread” between what they charge clients and pay pharmacies.32 Transparent PBM pricing passes through all discounts and rebates to the client, with the PBM charging an administrative fee.32
The increasing demand for greater transparency from self-funded employers and other payers is driving a notable shift towards the adoption of pass-through pricing models. A thorough understanding of these distinct PBM models is crucial for pharmaceutical companies, as they directly influence how their drugs are priced and how rebates are managed, which can ultimately impact formulary placement and overall market access. Under a spread pricing model, PBMs might have a financial incentive to favor higher-cost drugs that offer larger rebates, even if lower-cost therapeutic alternatives are readily available. In contrast, under a pass-through model, the PBM’s revenue is directly tied to administrative fees, potentially leading to a greater emphasis on overall cost management and the selection of the most clinically effective and cost-efficient therapies for inclusion on the formulary. Pharmaceutical companies must be acutely aware of these differing dynamics to effectively negotiate with PBMs and ensure optimal access for their medications within the complex landscape of prescription drug benefits.
Key Determinants Shaping Pharmaceutical Drug Prices
The Role of Research and Development (R&D) Expenditures
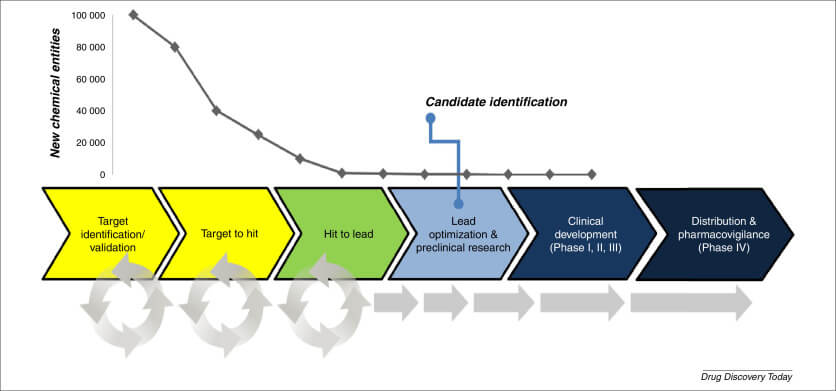
The pharmaceutical industry is distinguished by the substantial initial investments required for the extensive and intricate process of discovering, developing, and ultimately bringing new medications to market. These Research and Development (R&D) expenditures encompass a wide array of costs, including the expenses associated with fundamental laboratory research, comprehensive preclinical testing in animal models, the often lengthy and complex series of clinical trials in human subjects, and the considerable resources needed to navigate the stringent regulatory approval processes mandated by agencies like the FDA.12 Adding to the financial burden is the high rate of failure inherent in pharmaceutical R&D, where many promising drug candidates do not ultimately prove to be safe and effective enough to gain regulatory approval. This significant attrition rate further contributes to the overall R&D costs that pharmaceutical companies must attempt to recoup through the pricing of the relatively few drugs that successfully reach the market.
Research and development costs are a major factor influencing drug prices.12 The need to recoup these costs largely determines drug prices.34
While the argument that high R&D costs necessitate high drug prices is a common refrain within the pharmaceutical industry, there is an ongoing and often contentious debate regarding the transparency of these costs and whether the current pricing models fairly distribute this financial burden across all stakeholders. Business professionals should recognize that while investment in R&D is undeniably a critical driver of medical innovation and the development of new therapies, solely relying on this justification for maintaining high drug prices may face increasing scrutiny and skepticism from payers, policymakers, and the public at large. Payers and patients are increasingly demanding greater transparency concerning the actual costs incurred during the various stages of drug development. Pharmaceutical companies may find it necessary to provide more detailed and granular breakdowns of their R&D investments, clearly demonstrating the specific costs associated with bringing a particular drug to market. Furthermore, they may need to more effectively articulate and quantify the value that their innovative therapies bring to patients, such as improvements in clinical outcomes, enhancements in quality of life, and potential long-term cost savings for the healthcare system through the prevention of more expensive interventions. This increased transparency and focus on demonstrable value could be crucial in justifying their pricing strategies in an environment where affordability and access are paramount concerns.
Navigating Regulatory and Approval Processes
The journey of a pharmaceutical drug from its initial conception in a research laboratory to its availability for patients is heavily governed by a complex web of regulations overseen by government agencies, most notably the Food and Drug Administration (FDA) in the United States. These regulatory and approval processes are absolutely essential to ensure the safety, efficacy, and overall quality of all pharmaceutical products that reach the market.34 However, these processes can also be exceptionally time-consuming and financially demanding, often involving multiple phases of extensive clinical trials, the meticulous preparation and submission of vast amounts of scientific data, and rigorous reviews conducted by regulatory authorities.12 The considerable time and financial resources required to successfully navigate these intricate regulatory hurdles can significantly increase the total cost of drug development and, consequently, exert a substantial influence on the pricing decisions ultimately made by pharmaceutical companies.
Regulatory and approval processes impact drug pricing.34 The FDA’s review process can be lengthy and costly, contributing to higher prices.36
The regulatory environment plays a pivotal role in shaping the prices of pharmaceutical drugs by significantly contributing to the overall costs and timelines associated with their development and market entry. Business professionals operating within the pharmaceutical industry must possess a deep and nuanced understanding of these regulatory processes and carefully factor them into their strategic planning and pricing considerations. Achieving efficiency in navigating these complex regulatory pathways can potentially lead to significant cost savings and a more rapid time to market for new therapies, providing a crucial competitive advantage. Understanding the specific requirements and expectations of regulatory bodies in different geographical regions is absolutely essential for gaining access to global markets. Pharmaceutical companies that can effectively streamline their regulatory submissions, proactively address potential concerns, and efficiently manage the entire approval process may be able to bring their innovative drugs to market more quickly and potentially at a lower overall cost, thereby enhancing their competitive position and improving patient access to needed treatments.
The Impact of Market Competition and Patent Exclusivity
Market competition, or the absence thereof, stands as a critical determinant in the pricing of pharmaceutical drugs. When a new drug is initially introduced to the market, it is often protected by patents, which grant the company that developed it exclusive rights to manufacture and sell the drug for a specified period of time.12 This period of patent exclusivity effectively creates a temporary monopoly, allowing the company to set a higher price for the drug without the immediate pressure of direct competition. This pricing power is intended to enable the company to recoup its substantial investments in research and development and to generate profits that can be reinvested in future innovation. However, once the patent on a drug expires, generic manufacturers are then permitted to enter the market, producing and selling equivalent versions of the original brand-name drug, typically at significantly lower prices.12 This introduction of generic competition usually results in a dramatic decrease in the price of the medication, making it more affordable and accessible to a wider range of patients.
Market competition and patent exclusivity significantly influence drug prices.1 Patent exclusivity allows higher prices, while generic competition drives them down.12
The dynamic interplay between the period of patent protection granted to a new pharmaceutical drug and the subsequent entry of generic competitors into the market is a fundamental driver of drug pricing within the pharmaceutical industry. Business professionals must strategically manage their patent portfolios to maximize the duration of market exclusivity for their innovative products and proactively anticipate the potential impact of generic competition on their future revenue streams. A thorough understanding of this product lifecycle is absolutely crucial for long-term financial planning and for the development of effective strategies to maintain market share and profitability even after the original patent has expired. Pharmaceutical companies often employ a variety of tactics to either extend their market exclusivity or to mitigate the negative financial consequences of generic entry. These strategies can include developing new formulations of the drug, creating combination therapies that incorporate the original active ingredient, or securing additional patents that cover new uses or delivery methods for the medication. Business professionals need to carefully analyze these competitive tactics and develop their own comprehensive strategies for navigating the evolving competitive landscape throughout the entire lifecycle of their pharmaceutical products, from initial launch through the eventual entry of generic alternatives.
Influence of Government Policies and Price Controls
Government policies and regulations exert a considerable influence on the pricing of pharmaceutical drugs in countries around the world. Many nations implement various forms of price controls as a means to manage overall healthcare expenditures and to ensure that patients have access to essential medications at affordable prices.2 These control mechanisms can range from the imposition of direct price caps on specific medications and government negotiation of drug prices with manufacturers to the utilization of international reference pricing, where a drug’s price is benchmarked against its price in other countries with comparable economies and healthcare systems. In contrast to the approach taken by many other developed nations, the United States has historically maintained a system with fewer direct government price controls on pharmaceuticals. However, this landscape is currently undergoing changes with the recent enactment of legislation such as the Inflation Reduction Act.33
Government policies and regulations significantly influence drug prices.2 Many countries use price controls.12 The US has historically had fewer controls, but this is changing.33
The growing trend towards increased government involvement in the pricing of pharmaceutical drugs, particularly in major markets like the United States, signifies a substantial shift in the dynamics of the pharmaceutical market landscape. Business professionals operating within this industry must closely monitor these evolving policy changes and thoroughly understand their potential ramifications on their pricing strategies, their ability to access key markets, and their overall profitability. Adapting proactively to this evolving regulatory environment will be absolutely crucial for achieving long-term success and sustainability in the pharmaceutical industry. As governments worldwide continue to grapple with the challenges of rising healthcare costs and the imperative to ensure affordable access to essential medicines for their populations, pharmaceutical companies will likely face increasing pressure to justify their pricing decisions and potentially engage in direct price negotiations with government payers. Business professionals need to develop comprehensive strategies for effectively engaging with policymakers, gaining a deep understanding of the nuances of different regulatory frameworks across various regions, and adapting their pricing models to ensure compliance with evolving regulations while still maintaining a viable and profitable business.
Ethical Considerations in Pricing Decisions
The pricing of pharmaceutical drugs gives rise to significant ethical considerations, as it directly affects patients’ ability to access treatments that can be essential for their health and even their survival.12 Pharmaceutical companies face a constant ethical dilemma: balancing their fundamental fiduciary responsibility to their shareholders, which often includes the objective of maximizing profits, with their broader social responsibility to ensure that essential medicines are affordable and readily accessible to all individuals who need them. When drug prices are set at levels that are prohibitively high, patients may be forced to make agonizing choices between purchasing necessary medications and meeting other basic needs, such as food, housing, or utilities. This can lead to adverse health outcomes, a decline in overall well-being, and the exacerbation of existing health inequities within society.
Ethical considerations are crucial in drug pricing.12 Companies must balance profit with patient access.12
Ethical considerations are becoming increasingly central to the public discourse and policy debates surrounding the pricing of pharmaceutical drugs. Pharmaceutical companies that demonstrate a clear and consistent commitment to ethical pricing practices and prioritize the critical importance of patient access to their medications may find that they enhance their overall reputation and build greater trust among their various stakeholders, including patients, healthcare providers, and the broader community. Business professionals should carefully consider the long-term ethical implications of their pricing strategies and actively explore alternative pricing models that strive to promote both continued innovation in the development of new therapies and the widespread affordability of essential medicines. Public perception and a demonstrated commitment to social responsibility are increasingly important factors for businesses in all sectors, and the pharmaceutical industry is no exception. Companies that are perceived as engaging in practices such as price gouging or prioritizing short-term profits over the fundamental well-being of patients may face significant negative consequences in terms of their brand image, increased regulatory scrutiny from government agencies, and the potential for legislative action aimed at curbing perceived abuses. Conversely, by adopting ethical pricing frameworks and clearly demonstrating a genuine commitment to affordability and patient access, pharmaceutical companies can contribute to a more sustainable and responsible pharmaceutical market, fostering greater trust and goodwill among all stakeholders.
Supply Chain Dynamics and Distribution Costs
The pharmaceutical supply chain is an intricate and often opaque network that involves a multitude of intermediaries playing distinct roles in getting medications from the manufacturer to the patient. These key players typically include the pharmaceutical manufacturers themselves, wholesale distributors who purchase drugs in bulk, retail pharmacies that dispense medications directly to patients, and in the United States, Pharmacy Benefit Managers (PBMs) who manage drug benefits for insurance companies and employers.26 Each step in this complex chain can contribute to the final price that patients ultimately pay for their medications. These added costs can include the initial expenses of manufacturing the drug, the costs associated with transportation, secure storage, and careful handling of the pharmaceuticals, insurance costs to protect against loss or damage, and the various markups applied by each entity involved in the distribution process to cover their operational expenses and generate a profit. Additionally, factors such as tariffs and taxes imposed by governments, as well as dispensing fees charged by pharmacies for their services, further contribute to the overall cost of prescription drugs.
Supply chain dynamics and distribution costs affect drug prices.26 Multiple intermediaries add markups.26
Inefficiencies and a general lack of transparency within the pharmaceutical supply chain can significantly contribute to the higher prices that patients ultimately face. Business professionals should conduct a thorough analysis of the supply chain for their specific pharmaceutical products to identify potential areas where costs can be optimized and overall efficiency can be improved. Furthermore, promoting greater transparency in pricing throughout the entire supply chain could help to build trust among patients, payers, and policymakers and address concerns about potentially excessive markups applied by various intermediaries. By streamlining distribution processes, negotiating more favorable terms with suppliers and partners, and potentially reducing the number of unnecessary intermediaries involved in the chain, pharmaceutical companies and other stakeholders in the supply chain may be able to lower the overall cost of medications. This could lead to more affordable prices for patients without necessarily requiring a sacrifice in the profitability of the pharmaceutical manufacturers. Exploring innovative distribution models, such as direct-to-consumer options that bypass some traditional intermediaries, or establishing strategic partnerships with highly efficient distributors, could also yield significant cost savings that could ultimately benefit patients through lower drug prices.
The Ripple Effect: How Drug Pricing Impacts Stakeholders
Patients: Access, Affordability, and Adherence
Elevated prescription drug prices exert a significant and direct impact on patients, frequently establishing substantial obstacles to accessing necessary medications.11 When the cost of medications becomes prohibitively high, individuals may be compelled to make difficult and often detrimental choices, such as skipping prescribed doses to make their supply last longer, taking less medication than directed by their doctor, delaying the filling of new prescriptions, or, in the most severe cases, forgoing treatment altogether due to financial constraints. This cost-related non-adherence to prescribed medication regimens can lead to a deterioration of underlying health conditions, an increased likelihood of hospitalizations and emergency room visits, and ultimately, higher overall healthcare costs in the long term.48 Studies have indicated that a considerable percentage of adults in the United States report engaging in these cost-saving behaviors due to the high price of their medications 48, and this issue disproportionately affects vulnerable segments of the population, including senior citizens, individuals living with disabilities, and those who lack adequate health insurance coverage.48
High drug prices create barriers to patient access and can lead to non-adherence.11 Many Americans report not taking medication as prescribed due to cost.48
The overwhelming evidence clearly demonstrates that the elevated cost of prescription drugs in the United States represents a major crisis that significantly impacts patient health and overall well-being. Business professionals operating within the healthcare sector bear a crucial responsibility to actively participate in the development and implementation of effective solutions aimed at improving medication affordability and ensuring equitable access to essential treatments for all patients. Addressing this critical issue not only directly benefits patients by improving their health outcomes and quality of life but can also contribute to the establishment of a more sustainable and efficient healthcare system overall. When patients are unable to afford the medications they need to manage their health conditions, it sets in motion a cascade of negative consequences that extend far beyond the individual. These consequences include poorer overall health outcomes for the affected individuals, an increase in preventable emergency room visits and hospitalizations, and ultimately, higher total healthcare expenditures for the system as a whole. By prioritizing and effectively addressing the issue of medication affordability, businesses can play a vital role in fostering better patient health, reducing the overall burden on the healthcare system, and potentially creating new market opportunities for the development and delivery of more affordable treatment options and comprehensive patient support programs.
Pharmaceutical Companies: Balancing Innovation and Profitability
The drug pricing models that are adopted within the pharmaceutical industry have a direct and substantial impact on the financial health and the future innovative capacity of pharmaceutical companies.12 The revenue generated from the sales of pharmaceutical products serves as the primary source of funding for the crucial research and development (R&D) activities that are essential for the discovery and creation of new and improved therapies for a wide range of medical conditions.59 Pharmaceutical companies often argue that they must set the prices of their drugs at a level that allows them to adequately recoup their significant investments in R&D, cover the costs associated with manufacturing and distribution, and generate sufficient profits to incentivize continued innovation and the pursuit of future medical breakthroughs.44 However, these companies also face increasing pressure from patients, payers, and policymakers to ensure that their medications are accessible and affordable to all individuals who need them.12 This creates a persistent tension and a delicate balancing act between the fundamental need to maintain profitability to sustain operations and fuel innovation and the ethical and societal imperative to ensure broad access to essential medicines. Furthermore, government regulations regarding drug pricing, direct price negotiations with payers, and the ever-present threat of competition from generic drug manufacturers once patents expire add further layers of complexity to the pricing strategies that pharmaceutical companies must carefully navigate.60
Drug pricing models impact pharmaceutical companies’ financial health and innovation.12 Revenue from sales funds R&D.59 Companies need to balance profitability with access.12
Pharmaceutical companies operate within a highly complex and dynamic environment where they must skillfully navigate the often-competing demands of fostering medical innovation, maintaining financial profitability, and ensuring broad patient affordability of their products. Business professionals within this sector must develop sophisticated and nuanced pricing strategies that not only guarantee the long-term financial sustainability of their organizations but also proactively address the growing societal concerns surrounding the cost of prescription drugs and equitable access to them. This may involve actively exploring and adopting innovative pricing models that move beyond traditional volume-based approaches, focusing on clearly articulating and demonstrating the value proposition of their drugs in terms of improved patient outcomes, and engaging in proactive and constructive dialogue with policymakers, payers, and patient advocacy groups to find mutually acceptable solutions to the challenges of drug pricing. The long-term success of pharmaceutical companies is fundamentally dependent on their ability to maintain a robust pipeline of truly innovative drugs that address unmet medical needs. This requires significant and sustained investment in research and development across a wide range of therapeutic areas. However, if the pricing strategies adopted by these companies result in restricted patient access to essential medicines or contribute to unsustainable increases in overall healthcare costs, they may face increased regulatory scrutiny from government agencies, negative public perception that can damage their brand and reputation, and ultimately, a less favorable and more challenging market environment in which to operate. Therefore, finding a sustainable balance between the imperative of maintaining profitability to fuel future innovation and the critical need to ensure the affordability and accessibility of medications for all patients is absolutely crucial for the long-term viability and the social license to operate of the pharmaceutical industry as a whole.
Healthcare Providers: Navigating Costs and Treatment Options
Healthcare providers, encompassing physicians, hospitals, clinics, and other medical facilities, find themselves on the front lines of the ongoing challenges associated with pharmaceutical drug pricing.48 These professionals are becoming increasingly aware of the significant financial burden that the high cost of prescription drugs places on their patients. As a result, they often dedicate considerable time and effort to identifying more affordable treatment options, such as prescribing generic alternatives whenever clinically appropriate or guiding patients towards online discount pharmacies that may offer lower prices.48 The escalating costs of medications can also strain the budgets of hospitals and healthcare systems, potentially forcing them to make difficult decisions such as delaying necessary infrastructure investments, reducing staffing levels in certain areas, or seeking out alternative, and possibly less optimal, therapies for their patients.50 Furthermore, the increasingly frequent occurrence of drug shortages adds another layer of complexity to the challenges faced by healthcare providers. These shortages can disrupt established work patterns within medical facilities and negatively impact the quality of patient care. Addressing drug shortages often requires significant time and resources from healthcare staff to locate and procure alternative medications.50 Reimbursement policies and the often cumbersome prior authorization requirements imposed by insurance companies and Pharmacy Benefit Managers (PBMs), which are frequently influenced by drug pricing regulations, can also significantly affect providers’ prescribing practices and create additional administrative burdens that detract from direct patient care.54
Drug pricing models affect healthcare providers by influencing treatment options and costs.48 Rising prices strain hospital budgets.50
Healthcare providers are increasingly voicing their concerns about the pressing need for more affordable prescription drug options and greater transparency in the way drug prices are determined. Business professionals operating in the healthcare sector can play a vital role in supporting these providers by developing innovative tools and easily accessible resources that provide accurate and up-to-date drug cost data at the point of care. This information can empower providers to make more informed prescribing decisions and facilitate the selection of the most clinically effective and cost-effective medications for their patients. Additionally, businesses can contribute by streamlining administrative processes related to insurance coverage verification and prior authorization requirements, reducing the burden on healthcare providers and allowing them to focus more directly on patient care. Collaborating with healthcare providers to implement value-based care models can also help to align financial incentives with the ultimate goal of achieving positive patient outcomes while also promoting cost efficiency within the healthcare system. By offering solutions that address both the clinical and economic aspects of drug prescribing, businesses can become invaluable partners to healthcare providers, working together to create a more sustainable and patient-centered healthcare system.
Government Payers: Managing Budgets and Ensuring Access
Government payers, such as Medicare and Medicaid in the United States, are among the largest purchasers of prescription drugs, and the continuous increase in the cost of medications places a substantial strain on public budgets at both the federal and state levels.28 These governmental entities are entrusted with the dual responsibility of carefully managing healthcare expenditures to ensure the efficient use of taxpayer dollars while simultaneously guaranteeing that eligible beneficiaries have timely access to the prescription medications they require.53 To address the escalating costs of prescription drugs, governments employ a variety of strategies aimed at controlling prices and promoting affordability. These strategies can include engaging in direct negotiations with pharmaceutical companies to secure lower prices (as exemplified by the drug price negotiation provisions included in the Inflation Reduction Act in the US 40), implementing rebate systems that require manufacturers to provide refunds if their drug prices increase at a rate faster than the general rate of inflation 40, and exploring the adoption of international reference pricing models, which benchmark domestic drug prices against those in other developed nations.4 Additionally, government payers often utilize tools such as formularies, which are lists of covered medications, and prior authorization requirements, which necessitate pre-approval for certain medications, as mechanisms to manage drug utilization and contain overall costs.36 The effectiveness of these various policies and their potential consequences on pharmaceutical innovation and the accessibility of medications for patients are subjects of ongoing and often intense debate among policymakers, industry stakeholders, and patient advocacy groups.40
Drug pricing models significantly impact government payers like Medicare and Medicaid.28 Rising costs strain public budgets.40 Governments use negotiation, rebates, and reference pricing to manage costs.4
Government payers are actively pursuing various avenues to control the escalating costs of prescription drugs while ensuring that their beneficiaries maintain access to the medications they need. Business professionals operating within the pharmaceutical industry must develop a thorough understanding of the priorities and strategies of these government payers and be prepared to engage in constructive discussions regarding drug pricing and the overall value proposition of their products. This includes being transparent about the rationale behind their pricing decisions, effectively demonstrating the clinical and economic value offered by their medications, and potentially exploring innovative payment models that align with the government payers’ overarching goals of achieving both affordability and broad patient access. As government payers represent a substantial portion of the pharmaceutical market, their policies and purchasing decisions exert a significant influence on the entire industry. Pharmaceutical companies that can proactively address the concerns of government payers and offer solutions that provide demonstrable value for the public investment are more likely to achieve success in this evolving and increasingly regulated landscape. This might involve actively participating in government-sponsored value assessment programs, offering discounts or rebates on their medications, or developing risk-sharing agreements that tie payment to patient outcomes.
Emerging Trends and Pressing Challenges in Drug Pricing
The Escalating Costs of Novel and Specialty Therapies
The pharmaceutical industry is currently experiencing a notable increase in the development and regulatory approval of novel and specialty therapies, particularly targeted towards the treatment of complex and often life-threatening conditions such as various forms of cancer, rare genetic disorders, and chronic autoimmune diseases.36 While these cutting-edge therapies frequently offer significant clinical benefits and provide renewed hope for patients who previously had limited or no effective treatment options, they often come with extraordinarily high price tags. The annual cost for some of these innovative medications can reach hundreds of thousands or even millions of dollars per patient.36 This escalating cost of novel medicines presents a considerable challenge to the sustainability of healthcare systems, the financial stability of payers, and the affordability of treatment for patients, raising significant concerns about equitable access to these potentially life-saving advancements. Specialty drugs now constitute a substantial and rapidly growing proportion of the overall spending on prescription medications.68
Novel and specialty therapies have escalating costs.36 Some can cost hundreds of thousands or millions annually.36
The increasing availability of high-cost novel and specialty therapies necessitates a critical re-evaluation of current drug pricing models and the urgent development of sustainable financing mechanisms to ensure patient access. Business professionals operating in the pharmaceutical and healthcare sectors need to carefully consider the long-term implications of these escalating costs and actively explore alternative pricing strategies, such as value-based pricing that aligns cost with therapeutic outcomes, risk-sharing agreements that distribute financial responsibility between payers and manufacturers, and other innovative approaches aimed at ensuring that these potentially life-changing treatments are accessible to patients who need them without jeopardizing the financial stability of the broader healthcare system. The traditional pricing models that have historically been used for more conventional medications may not be appropriate or sustainable for these ultra-expensive therapies. Payers are increasingly scrutinizing the value proposition of these high-cost drugs and demanding robust evidence of significant clinical benefit to justify their use and reimbursement. Pharmaceutical companies, in turn, need to engage in proactive and transparent dialogue with payers, healthcare providers, and patient advocacy groups to develop pricing strategies that clearly demonstrate the value of their innovative treatments and ensure patient access through flexible payment options, outcomes-based agreements, or other mechanisms that address the affordability challenge.
The Growing Demand for Price Transparency
There is an increasingly vocal and widespread demand from patients, policymakers, healthcare payers, and even some segments of the pharmaceutical industry itself for greater transparency in the complex process of how pharmaceutical drug prices are determined.2 The current lack of clarity and readily available information surrounding the various factors that influence the final price of a drug, including the often-debated costs of research and development, the actual expenses associated with manufacturing, the significant expenditures on marketing and advertising, and the intricate role of rebates and discounts within the pharmaceutical supply chain, erodes public trust in the system and makes it exceedingly difficult for patients and payers to make informed decisions about treatment options and healthcare spending. Advocates for enhanced price transparency argue that shedding light on these currently opaque aspects of drug pricing would foster greater accountability among all stakeholders, potentially help to curb excessive and unjustified price increases, and empower patients to compare the costs of different medications and choose more affordable alternatives when appropriate. Some policy initiatives are already underway, pushing for greater disclosure of both the list prices of drugs and the net prices after all discounts and rebates have been applied.28
There is a growing demand for transparency in drug pricing.2 The lack of clarity erodes public trust.12
The demand for greater price transparency within the pharmaceutical industry is a trend that is highly likely to continue and even intensify in the coming years. Business professionals operating in this sector should recognize this growing expectation and consider proactively adopting more transparent pricing practices. This could involve providing clearer and more detailed explanations of the various factors that influence the prices of their drugs, including a breakdown of relevant costs and the role of any discounts or rebates offered. Engaging in open and honest dialogue with all stakeholders, including patients, healthcare providers, payers, and policymakers, about the value that their products offer and the rationale behind their pricing strategies can also be a crucial step in building trust and mitigating the negative perceptions that often arise from the current lack of transparency surrounding high drug costs. Embracing a culture of transparency can not only help to improve the industry’s overall reputation but may also potentially provide a competitive advantage by fostering stronger and more trusting relationships with customers and other key stakeholders.
The Influence of International Pricing Comparisons
The persistent and often substantial price differences observed between prescription drugs in the United States and those in other developed countries continue to be a major source of public debate and a significant driver of policy discussions aimed at lowering drug costs in the U.S..5 Numerous independent studies and comprehensive reports have consistently demonstrated that the United States pays significantly more for brand-name prescription medications compared to other nations with similar levels of economic development and comparable healthcare systems. For example, a recent 2024 study conducted by the RAND Corporation found that, across all types of prescription drugs, the prices in the U.S. were on average 2.78 times as high as the prices in 33 other developed countries in 2022.9 This price gap is even more pronounced for brand-name drugs, with U.S. prices averaging 4.22 times as high as those in the studied nations, even after accounting for rebates funded by the manufacturers.5 Interestingly, the U.S. generally pays less for unbranded generic drugs when compared to these same international markets.5 This stark disparity in drug prices between the U.S. and other developed nations continues to fuel calls for significant policy reforms within the U.S., such as allowing the federal Medicare program to directly negotiate drug prices with manufacturers and implementing some form of international reference pricing, with the ultimate goal of bringing U.S. drug costs more in line with the levels observed in other developed countries.
US drug prices are significantly higher than in other developed nations.5 This influences policy discussions.28
The substantial price gap that exists between prescription drugs in the United States and those in other developed nations is highly likely to continue to exert significant pressure on U.S. policymakers to implement measures aimed at lowering drug costs. Business professionals operating within the pharmaceutical industry need to proactively anticipate these potential policy changes and carefully evaluate how they might impact their current pricing strategies and their overall access to the U.S. market. Gaining a thorough understanding of the pricing mechanisms and negotiation processes that are employed in other countries can provide valuable insights for adapting to a potentially more regulated U.S. market in the future. The fact that the U.S. pays considerably more for prescription drugs, particularly for brand-name medications, suggests that there may be underlying inefficiencies or unique market dynamics at play. Business professionals should meticulously analyze these factors to identify potential areas for innovation in pricing and market access that could lead to more competitive and sustainable offerings in the U.S. market.
Addressing Drug Shortages and Their Economic Impact
Drug shortages have become an increasingly worrisome issue within the pharmaceutical supply chain, with the potential to negatively impact patient care and drive up healthcare costs.50 When essential medications become unavailable, healthcare providers are often forced to seek out alternative therapies for their patients. These alternatives may be less effective in treating the condition, may have a higher incidence of adverse side effects, or may be significantly more expensive than the first-line treatment that is in short supply.50 The occurrence of drug shortages can also disrupt the established workflows within hospitals and pharmacies, requiring healthcare professionals to dedicate significant time and resources to managing the shortage and attempting to procure alternative supplies through less conventional channels.50 Generic drugs, which often have lower profit margins for manufacturers compared to their brand-name counterparts, are particularly vulnerable to shortages due to various factors such as manufacturing difficulties, vulnerabilities within the global supply chain, or a lack of strong economic incentives for manufacturers to continue producing these lower-margin medications.39 These shortages can ultimately lead to increased spending for both hospitals and patients, as they may be compelled to pay higher prices for any available alternative medications.52
Drug shortages are a growing concern with economic impact.50 They can lead to higher costs and impact patient care.50 Generic drugs are often affected.39
Drug shortages represent a significant challenge that necessitates a comprehensive and multi-faceted approach involving collaboration among pharmaceutical manufacturers, regulatory agencies, and healthcare providers. Business professionals within the pharmaceutical industry can play a crucial role in addressing this issue by investing in the development of robust and diversified supply chains that are less susceptible to disruption. Ensuring reliable and high-quality manufacturing processes is also paramount. Furthermore, businesses could explore strategies to make the continued production of essential generic drugs more economically sustainable, perhaps through government incentives or innovative contracting models. The application of emerging technologies, such as blockchain, could also be investigated as a means to enhance transparency and build greater resilience within the complex pharmaceutical supply chain. Ensuring a stable and reliable supply of medications is absolutely crucial for maintaining consistent patient access to needed treatments and preventing potentially dangerous disruptions in care. By proactively addressing the underlying causes of drug shortages, businesses can contribute to a more stable and predictable pharmaceutical market, ultimately benefiting both patients and the healthcare system as a whole. This might involve fostering greater collaboration among all stakeholders to identify potential vulnerabilities within the supply chain and working collectively to develop effective strategies for mitigating these risks.
Expert Perspectives on the Drug Pricing Debate
Insights from Pharmaceutical Industry Leaders
Leaders within the pharmaceutical industry frequently emphasize the essential role that the revenue generated from high drug prices plays in funding the incredibly costly and inherently risky process of research and development (R&D) that is absolutely necessary to discover, develop, and ultimately bring innovative new medicines to patients.3 They often argue that any substantial reduction in drug prices could severely jeopardize the industry’s ability to invest in future innovation by making pharmaceutical R&D less financially attractive to investors.59 Furthermore, they highlight the significant value that their medicines provide to patients and the healthcare system as a whole, such as preventing the need for more invasive and costly interventions or significantly improving patients’ overall quality of life.44 Some leaders within the pharmaceutical sector are also actively exploring and advocating for the broader adoption of value-based pricing models as a more equitable and sustainable way to better align the cost of drugs with the actual therapeutic benefits they deliver to patients.3
Pharmaceutical industry leaders argue that high prices fund R&D.3 They also highlight the value of their medicines 44 and explore value-based pricing.3
Pharmaceutical industry leaders generally hold the perspective that a robust pricing environment is indispensable for sustaining the high levels of financial investment required to drive continued pharmaceutical innovation. Business professionals should take this viewpoint into account when participating in discussions and debates surrounding drug pricing policies and consider how to strike a balance between the critical need to ensure that medicines are affordable and accessible to patients and the equally important imperative to incentivize the development of new and better treatments for a wide range of medical conditions. While the pharmaceutical industry’s argument regarding the necessity of high prices to fund R&D is a central component of the ongoing drug pricing debate, it is also crucial to acknowledge the valid counterarguments that have been raised concerning the transparency of these costs and the fundamental need to ensure that patients have affordable access to essential medications. A nuanced and comprehensive understanding of the pharmaceutical industry’s perspective is therefore essential for developing balanced and effective solutions to the complex challenges associated with pharmaceutical drug pricing.
Analyses from Healthcare Economists
Healthcare economists bring a critical and analytical perspective to the complex issue of drug pricing, meticulously examining the various economic forces that shape pharmaceutical markets and rigorously evaluating the efficiency and equity of different pricing models.29 Many economists point to the unique characteristics inherent in the pharmaceutical market, such as the relatively inelastic demand for essential medicines (meaning that patients’ need for these drugs is not significantly affected by price changes) and the information asymmetry that often exists between patients and the healthcare professionals who prescribe medications, as significant contributing factors to the prevalence of high drug prices.45 They frequently draw comparisons between the drug pricing system in the United States and those in other developed countries, highlighting the relative lack of centralized negotiation power and direct price controls in the U.S. as key reasons for the higher prices observed in this market.29 Healthcare economists also conduct in-depth analyses of the potential impact of various policy interventions that have been proposed or implemented, such as value-based pricing models, international reference pricing, and government negotiation of drug prices, on both the cost of medications and the level of pharmaceutical innovation.29
Healthcare economists analyze the economic forces shaping drug pricing.29 They often compare the US system to others, noting the lack of negotiation and price controls.29
The analyses provided by healthcare economists offer valuable data-driven insights into the multifaceted complexities of drug pricing and the potential consequences, both intended and unintended, of different policy choices that are being considered or implemented. Business professionals operating within the pharmaceutical and healthcare sectors can greatly benefit from understanding these economic analyses to inform their own strategic decision-making processes and to better navigate the constantly evolving landscape of pharmaceutical pricing and regulation. The rigorous analyses conducted by healthcare economists can help to identify the fundamental root causes of high drug prices and to evaluate the potential effectiveness, as well as the potential drawbacks and unintended consequences, of various proposed solutions aimed at addressing these issues. This deep understanding can be particularly crucial for pharmaceutical companies in developing sustainable and responsible pricing strategies for their products and for policymakers in designing effective regulations that promote both affordability and continued innovation within the pharmaceutical industry.
The Stance of Patient Advocacy Groups
Patient advocacy groups fulfill a vital role in representing the interests and amplifying the voices of patients, actively advocating for policies that aim to ensure affordable access to the medications that individuals need to manage their health conditions.75 These organizations frequently highlight the significant challenges and hardships faced by patients who struggle to afford their prescription drugs, including having to make difficult and often life-altering choices between purchasing essential medications and meeting other fundamental needs such as food, housing, and utilities.56 Patient advocacy groups generally express strong support for measures that are intended to lower the cost of prescription drugs, such as allowing government negotiation of prices, implementing price caps on certain medications, and increasing the overall transparency of drug pricing mechanisms throughout the supply chain.76 While these groups recognize the critical importance of continued pharmaceutical innovation in developing new and better treatments, they consistently emphasize that the potential benefits of these new medicines cannot be realized if patients are unable to afford them and therefore cannot access the care they need.65 Some patient advocacy organizations also voice concerns regarding certain proposed pricing models, such as indication-based pricing, fearing that these approaches could inadvertently lead to discrimination against patients with specific medical conditions or those requiring treatment for less common diseases.76
Patient advocacy groups advocate for affordable access to medications.75 They often support government negotiation and price caps.76
Patient advocacy groups serve as powerful and influential voices in the ongoing drug pricing debate, and their perspectives, experiences, and concerns are increasingly shaping the direction of policy discussions at both the legislative and regulatory levels. Business professionals operating within the pharmaceutical industry should actively engage with these advocacy groups, strive to understand their key priorities and concerns, and carefully consider how their own business practices and policies can be better aligned with the needs of the patient community they ultimately serve. Building trust and demonstrating a genuine commitment to improving medication affordability and accessibility can foster stronger and more positive relationships with the patient community, which is a critical stakeholder in the healthcare ecosystem. By listening to and addressing the concerns raised by patient advocacy groups, pharmaceutical companies can not only enhance their public image and corporate reputation but also potentially identify valuable opportunities to develop more patient-centric pricing and access strategies that better meet the needs of the individuals who rely on their medications.
Illustrating the Landscape: Key Statistics on Drug Pricing
US Prescription Drug Spending: Trends and Figures
The United States stands out among developed nations for its consistently higher per capita spending on prescription drugs. In 2021, the total expenditure on prescription drugs in the US reached approximately $603 billion 69, with the majority of this spending occurring in the retail sector. This figure represents a substantial increase in overall drug spending over the past decade.68 Notably, while specialty drugs account for a smaller proportion of the total number of prescriptions filled, they now represent over 50% of the total drug spending in the US, with significant growth observed in therapeutic areas such as immunology and oncology.68 Medicare Part D, a major government-funded program that helps beneficiaries with the cost of prescription drugs, covered more than 3,500 different prescription drug products in 2021, with total gross expenditures amounting to $216 billion.68
US prescription drug spending is the highest per capita among developed nations.74 Total spending reached $603 billion in 2021.69 Specialty drugs account for over 50% of spending.68
The sheer magnitude and the continued upward trajectory of prescription drug spending in the United States underscore the significant economic impact of this sector and the pressing need for effective strategies aimed at managing and potentially reducing these costs. Business professionals should carefully analyze these spending trends to identify emerging market opportunities in areas such as the development and production of generic and biosimilar medications, the implementation of value-based care solutions that focus on outcomes and cost-effectiveness, and the development of innovative strategies to improve patient adherence to prescribed medication regimens. A thorough understanding of where the financial resources are being allocated within the pharmaceutical market can help businesses to strategically focus their efforts and investments in areas that offer the greatest potential for future growth and positive impact on the healthcare system. The increasing dominance of spending on specialty drugs, for instance, suggests a growing demand for the development of novel pricing and reimbursement models that are specifically tailored to these high-cost therapies, ensuring both patient access and financial sustainability.
Table 1: Trends in US Prescription Drug Spending (2016-2021)
| Year | Total Spending (Billions) | Retail Spending (Billions) | Non-Retail Spending (Billions) | % Change from 2016 |
| 2016 | $520 | $368 | $152 | 0% |
| 2017 | $535 | $377 | $158 | 2.9% |
| 2018 | $562 | $394 | $168 | 8.1% |
| 2019 | $580 | $405 | $175 | 11.5% |
| 2020 | $590 | $412 | $178 | 13.5% |
| 2021 | $603 | $421 | $182 | 16.0% |
Data Source: ASPE 69 (Inflation-adjusted expenditures)
This table provides a clear, year-over-year overview of the growth in total, retail, and non-retail prescription drug spending in the US, allowing business professionals to quickly grasp the overall trend and the relative contributions of different sectors.
Comparative Drug Prices: US vs. Other Developed Nations
Numerous studies have consistently demonstrated a significant disparity in prescription drug prices, with the United States exhibiting substantially higher costs compared to other high-income industrialized countries. A comprehensive 2024 study conducted by the RAND Corporation revealed that, across all categories of prescription drugs, the prices in the U.S. were on average 2.78 times as high as the prices in 33 other developed nations in 2022.9 This price gap becomes even more pronounced when specifically examining brand-name drugs, where U.S. prices averaged an astonishing 4.22 times as high as those in the studied nations, even after taking into account rebates provided by the manufacturers.5 Interestingly, in contrast to this trend, the U.S. generally benefits from lower prices for unbranded generic drugs when compared to these same international markets.5
US prices are 2.78 times higher than in 33 other countries.9 Brand-name drugs are 4.22 times higher.5 Generic drugs are generally cheaper in the US.5
The substantial price differential that exists between the United States and other developed nations presents both a significant challenge and a potential area of opportunity for businesses operating within the U.S. pharmaceutical market. For these businesses, gaining a deep understanding of the underlying reasons for these higher prices and closely monitoring the various policy efforts aimed at addressing this disparity is absolutely crucial for effective strategic planning. This price gap also highlights the considerable potential for cost savings if U.S. drug prices were to align more closely with the international levels observed in comparable countries. The fact that the U.S. incurs significantly higher costs for prescription drugs, particularly for brand-name medications, suggests that there may be inherent inefficiencies or unique market dynamics at play within the U.S. healthcare system. Business professionals should meticulously analyze these contributing factors to identify potential areas for innovation in both pricing strategies and market access approaches that could ultimately lead to the development of more competitive and sustainable pharmaceutical offerings within the U.S. market.
Table 2: US Prescription Drug Prices as a Percentage of Other Countries’ Prices (2022)
| Drug Category | US Price as Percentage of Other Countries’ Prices |
| All Drugs | 278% |
| Brand-Name Originator Drugs | 422% |
| Unbranded Generic Drugs | 67% |
Data Source: RAND Corporation 7
This concise table directly illustrates the magnitude of the price difference across key drug categories, providing a powerful visual representation of the US’s outlier status in drug pricing.
The Affordability Crisis: Impact on Patients
The elevated cost of prescription drugs in the United States has precipitated a significant affordability crisis for a substantial portion of the patient population. In 2021, a concerning 8.2% of adults aged 18 to 64 who were prescribed medication reported that they did not take their medication as directed by their healthcare provider due to financial constraints.58 This alarming statistic translates to over 9 million adults in this age group who were forced to ration their medications in an attempt to make them last longer.57 Notably, certain demographic groups were even more likely to report cost-related non-adherence, including women and adults living with disabilities.58 Furthermore, nearly 30% of all Americans report that they have not taken their medication as prescribed at some point due to the high cost, and estimates suggest that over 1.1 million Medicare patients alone could face premature death over the next decade simply because they cannot afford to pay for the medications they desperately need.52
8.2% of US adults aged 18-64 didn’t take medication as prescribed due to cost in 2021.58 Over 9 million adults rationed medications.57 Nearly 30% of all Americans have skipped medication due to cost.52
These statistics paint a stark and sobering picture of the profound human cost associated with the high prices of prescription drugs in the United States. Business professionals operating within the healthcare and pharmaceutical sectors should recognize the urgent need to address this crisis and prioritize the development and implementation of effective solutions that improve medication affordability and ensure equitable access to essential treatments for all patients who need them. Addressing this critical societal issue not only directly alleviates the burden on individuals and improves public health outcomes but also represents a significant market opportunity for companies that can successfully offer more affordable alternatives or innovative payment solutions that help patients manage the financial challenges of accessing necessary medications. The widespread issue of medication non-adherence due to cost has far-reaching implications for both individual well-being and the overall efficiency and effectiveness of the healthcare system. By focusing on improving affordability, businesses can contribute to better patient health outcomes, reduce the incidence of preventable emergency room visits and hospitalizations, and ultimately lower the total burden of healthcare expenditures. Moreover, by meeting this critical unmet need in the market, companies that prioritize affordability can potentially gain a significant competitive advantage and build lasting relationships with patients and payers alike.
Table 3: Percentage of Adults Aged 18-64 Not Taking Prescription Medication as Prescribed Due to Cost (US, 2021)
| Demographic Group | Percentage |
| Overall | 8.2% |
| Women | 9.1% |
| Men | 7.0% |
| Adults with Disabilities | 20.0% |
| Uninsured | 18.1% |
Data Source: CDC 58
This table clearly shows the disparities in medication affordability across different demographic groups, highlighting the disproportionate impact on vulnerable populations and underscoring the need for targeted solutions.
Trends in Drug Price Inflation
While there has been some indication of moderation in recent years, the historical trend in the United States has been that prescription drug prices increase at a rate that consistently surpasses the general rate of inflation in the economy.11 Between January 2022 and January 2023, a significant number of drug products, totaling over 4,200, experienced price increases, with nearly half of these increases exceeding the rate of inflation during that period.79 The average price increase across all of these drugs was a substantial 15.2%, which translates to an average increase of $590 per individual drug product.52 Although recent data from early 2025 suggest a median price increase of around 4.5% for branded drugs 80, the long-term trend of rising drug prices remains a significant concern for both healthcare payers and patients who are struggling to afford their medications. Furthermore, new pharmaceutical drugs continue to be launched onto the market at record-high prices, with the median annual price for newly introduced drugs reaching $300,000 in 2023, representing a significant 35% increase compared to the prices of drugs launched in the previous year.52
Drug prices in the US have historically increased faster than general inflation.11 Over 4,200 drugs had price increases from Jan 2022 to Jan 2023, averaging 15.2%.79 New drugs are launched at record high prices.52
Despite some recent indications of a potential slowdown in the rate of price growth for certain prescription drugs, the overarching trend of increasing drug prices, particularly for innovative and specialty therapies, continues to pose a significant challenge to the long-term sustainability of the healthcare system and the affordability of essential medications for patients. Business professionals operating within the pharmaceutical and healthcare sectors need to remain keenly aware of these ongoing inflationary trends and carefully consider their potential implications for market access, negotiations with payers regarding reimbursement, and long-term financial planning. Monitoring these trends will be absolutely crucial for anticipating future dynamics within the pharmaceutical market and for adapting business strategies proactively to navigate the evolving landscape of drug pricing and reimbursement. The continued upward pressure on drug prices necessitates a proactive and strategic approach from businesses to effectively manage their own costs, clearly demonstrate the value that their products provide to patients and the healthcare system, and engage in constructive dialogue with policymakers and payers to explore and implement sustainable pricing solutions that ensure both innovation and affordability.
Real-World Applications: Case Studies in Drug Pricing
Value-Based Agreements: Examples and Outcomes
Value-based agreements are increasingly being adopted within the pharmaceutical industry as a mechanism to link the payment for a drug to its actual performance and the health outcomes it achieves in real-world clinical settings. One prominent example of this approach involves the cholesterol-lowering medication Praluent (alirocumab). The manufacturers of Praluent, Sanofi and Regeneron, made the strategic decision to lower the drug’s price in exchange for securing exclusive formulary placement with a major pharmacy benefit manager (PBM) after an independent analysis suggested that the initial price of the drug was not appropriately aligned with the clinical value it provided to patients.81 Another notable example involves the use of financial risk-based contracts, where the reimbursement a pharmaceutical company receives is directly tied to the achievement of predetermined financial outcomes, such as successfully treating a patient at a lower overall cost compared to a competing therapy.3 The adoption and implementation of these types of value-based contracts have been on the rise, particularly for innovative specialty drugs and medications that target rare diseases and are often referred to as orphan products.3 Furthermore, outcomes-based pricing, a specific type of value-based approach where the cost of a drug is directly linked to its observed clinical outcomes in real-world use, is also gaining increasing traction within the healthcare industry.82
Value-based agreements link payment to real-world performance.81 Example: Praluent’s price was lowered for better formulary placement.81 Financial risk-based contracts tie reimbursement to financial outcomes.3
These real-world case studies clearly demonstrate the potential benefits of implementing value-based agreements within the pharmaceutical industry. These agreements can lead to improved patient access to effective treatments by making them more affordable and can also foster a stronger alignment between the cost of a medication and the actual therapeutic value it delivers to patients and the healthcare system. However, these examples also highlight the inherent complexities involved in the successful establishment and ongoing management of these types of contracts. These complexities include the critical need for robust systems to collect, analyze, and share comprehensive patient data across different healthcare settings. Business professionals operating in the pharmaceutical sector should carefully explore the feasibility and potential benefits of implementing value-based agreements for their own products, particularly for medications that have high costs and the potential to significantly improve patient health outcomes. Value-based agreements can represent a mutually beneficial arrangement for both healthcare payers and pharmaceutical companies. Payers can mitigate the financial risk associated with investing in high-cost therapies by only paying when the drug achieves the anticipated positive outcomes. On the other hand, pharmaceutical companies can potentially gain better market access for their innovative products and may even be able to justify higher prices if they can clearly demonstrate the superior therapeutic value and positive impact of their medications on patient health and the overall healthcare system.
The Cost-Plus Model in Action: A Disruptive Approach
The Mark Cuban Cost Plus Drug Company (MCCPDC) stands as a prominent and compelling real-world example of the cost-plus pricing model being applied within the healthcare industry.18 Founded with a clear mission to provide patients with access to affordable generic medications, MCCPDC operates as an online pharmacy that adheres to a transparent pricing strategy. They charge a standard markup of only 15% over the actual cost of manufacturing the drug, and they add a nominal $5 fee to cover pharmacy labor costs as well as a $5 fee for shipping the medication directly to the patient.18 By strategically bypassing traditional pharmacy benefit managers (PBMs) and negotiating directly with drug manufacturers to secure lower acquisition prices for generic medications, MCCPDC has been able to offer a wide range of prescription drugs at significantly lower prices compared to those typically found at traditional brick-and-mortar pharmacies and even the contracted rates negotiated by the Medicare Part D program.18 Several studies have already demonstrated the substantial potential for cost savings for patients who utilize the MCCPDC model to obtain their medications, particularly for commonly prescribed generic drugs used to treat a variety of conditions.20
Mark Cuban Cost Plus Drug Company uses a cost-plus model.18 They charge a 15% markup plus fees.18 This model offers significantly lower prices than traditional pharmacies and Medicare.18
The success and growing popularity of the Mark Cuban Cost Plus Drug Company clearly demonstrate a significant demand within the healthcare market for more transparent and affordable models of drug pricing. This disruptive approach directly challenges the traditional pharmaceutical supply chain and the established pricing structures that have long been in place, suggesting a potential shift towards greater price transparency and significantly lower markups on prescription medications. Business professionals operating in the pharmaceutical and healthcare sectors should carefully consider the broader implications of such models for the future of drug pricing and actively explore opportunities to adopt more transparent and value-driven pricing strategies for their own products and services. The MCCPDC model has clearly resonated with patients and healthcare payers who have grown increasingly frustrated with the complexity and the often-prohibitive costs associated with prescription drugs in the traditional system. The company’s commitment to transparency and its focus on applying a low, fixed markup to the cost of medications have helped to build trust with consumers and offer a clear and compelling alternative to the often-opaque pricing practices of the established pharmaceutical supply chain. This example underscores the potential for businesses to gain a significant competitive advantage by prioritizing affordability and transparency in their pricing strategies, ultimately benefiting patients and potentially reshaping the future of the pharmaceutical market.
Competitive Dynamics: The Impact of Generic Entry
The entry of generic pharmaceutical drugs into the market following the expiration of patents on their brand-name counterparts provides a clear and well-documented case study of competitive pricing in action within the pharmaceutical industry.39 The introduction of generic competition typically leads to significant price reductions for the medication, often occurring within a relatively short period after the first generic version becomes available to patients.39 These substantially lower prices for generic drugs play a crucial role in increasing the overall affordability and accessibility of essential medicines for a wider segment of the population.39 However, the dynamics of competition within the pharmaceutical market can be quite complex and are not always straightforward. In some instances, even after multiple generic manufacturers have entered the market, the prices of both the original brand-name drug and the newly introduced generic versions may not decrease as dramatically as might be expected. In other cases, the prices of existing brand-name drugs have even been observed to increase following the introduction of brand-name competition for the same therapeutic indication.83 These seemingly counterintuitive pricing behaviors can be attributed to a variety of factors, including the specific market dynamics for that particular drug, the marketing strategies employed by both the original manufacturer and the generic competitors, and the inherent complexities of the pharmaceutical supply chain, including the role of PBMs and insurance formularies.
Generic entry typically leads to significant price reductions 39, increasing affordability.39 However, competitive dynamics can be complex, with prices sometimes not falling as expected.83
While the introduction of generic competition is generally an effective mechanism for lowering the prices of pharmaceutical drugs and increasing patient access, the extent of the price reduction and the specific competitive strategies employed by both the original brand-name manufacturers and the generic drug companies can vary considerably depending on the specific drug and the prevailing market conditions. Business professionals operating in the pharmaceutical sector need to develop a thorough understanding of these complex dynamics when assessing the market potential for generic drugs and when formulating strategies to effectively compete with generic versions of their own products once they lose patent protection. Various factors can influence pricing and market share in the generic drug market, including the number of generic competitors that ultimately enter the market, the complexity of the manufacturing process for the drug, and the presence of any remaining market advantages or brand loyalty associated with the original brand-name product. By carefully analyzing these factors, businesses can make more informed decisions regarding their strategies for both entering the generic market and for managing the lifecycle of their branded pharmaceutical products in the face of increasing generic competition.
International Reference Pricing: Successes and Challenges
A number of countries around the world have adopted the policy of international reference pricing (IRP) as a tool to exert control over the cost of prescription drugs within their healthcare systems.4 This approach involves setting the price of a particular drug based on the average or the lowest price at which that same drug, or a very similar one, is sold in a selected basket of other countries that are considered to be economically comparable. Countries such as Germany, France, and Canada have all implemented various forms of reference pricing over the years.4 Proponents of IRP argue that it has the potential to significantly reduce a country’s overall spending on prescription drugs by effectively leveraging the often lower prices that are negotiated or regulated in other international markets.4 However, there are also notable challenges and potential drawbacks associated with the widespread adoption of this pricing strategy. Pharmaceutical companies, for example, may argue that referencing drug prices in countries that have fundamentally different healthcare systems, economic conditions, and regulatory environments is not an appropriate or fair approach and could ultimately stifle innovation in the development of new medicines.28 Additionally, there are concerns that the implementation of IRP in certain countries could lead to delays in the launch of new drugs in those markets where prices are set lower, or that it could even inadvertently cause manufacturers to raise their prices in the reference countries to offset potential losses in other markets.28
Several countries use international reference pricing (IRP).4 It can lower drug spending.4 Challenges include potential impact on innovation and drug launch delays.28
International reference pricing represents a complex policy instrument that offers the potential to lower drug costs for participating countries but also carries significant implications for pharmaceutical innovation and the dynamics of global pharmaceutical markets. Business professionals operating within the pharmaceutical industry need to closely monitor policy developments related to the adoption and expansion of IRP, particularly in major markets such as the United States, and thoroughly understand how this pricing approach might affect their global pricing strategies and their ability to access key markets around the world. A careful and comprehensive evaluation of the potential benefits and the inherent drawbacks of international reference pricing is absolutely essential for both policymakers who are considering its implementation and for pharmaceutical companies that need to adapt their business models to navigate a world where IRP is becoming an increasingly discussed and, in some regions, implemented policy. While IRP could potentially lead to lower drug prices in countries like the United States, pharmaceutical companies might respond strategically by adjusting their pricing in other markets or by prioritizing the launch of their newest and most innovative drugs in countries that offer more favorable pricing environments. Understanding these potential reactions and strategic shifts is crucial for businesses to develop effective global pricing strategies in an increasingly interconnected world where international reference pricing is playing a more prominent role in shaping pharmaceutical markets.
Strategic Implications: Leveraging Drug Pricing Insights for Business Advantage
Understanding Pricing Models for Market Entry and Negotiation
For business professionals striving to achieve market dominance in the pharmaceutical industry, a comprehensive understanding of the various drug pricing models employed globally is absolutely essential. When contemplating market entry into a new region or for a new product, companies must meticulously analyze which pricing models are most prevalent in their target markets and which are most likely to be accepted by both healthcare payers and patients. For instance, entering a market characterized by strong government price controls and direct negotiation might necessitate the adoption of a cost-plus or a reference pricing strategy to align with regulatory expectations. Conversely, a more market-driven environment with less government intervention might afford greater flexibility, allowing for the implementation of value-based or competitive pricing models that are more responsive to market dynamics. This in-depth knowledge of different pricing models is equally critical during negotiations with various stakeholders, including healthcare payers (such as insurance companies and government agencies), Pharmacy Benefit Managers (PBMs), and governmental entities responsible for drug reimbursement policies. Being able to clearly articulate the value proposition of a particular drug within the framework of different pricing models can significantly enhance a company’s negotiating power and increase the likelihood of achieving favorable pricing and reimbursement agreements. A thorough understanding of the payer’s preferred pricing models, as well as the underlying rationale and data that support those preferences, enables companies to develop pricing proposals that are more likely to be successful and ensure optimal market access for their products.
Identifying Opportunities for Cost Optimization and Value Creation
A thorough understanding of the intricacies of different drug pricing models can also uncover valuable opportunities for businesses to achieve cost optimization within their own operations and to create enhanced value for patients and the healthcare system. For example, a detailed analysis of the cost-plus pricing model might highlight specific areas within a company’s supply chain or its manufacturing processes where efficiencies can be gained and costs can be reduced. These reductions in production costs can then potentially translate into more competitive pricing for the drug, making it more attractive to payers and patients. Similarly, a deep understanding of the core principles of value-based pricing can guide a company’s research and development (R&D) efforts towards focusing on the development of drugs that offer significant therapeutic benefits and demonstrably improved patient outcomes. By prioritizing the development of such high-value medications, companies can then more effectively justify a higher price point for their products based on the tangible value they deliver to patients and the overall healthcare system. By strategically focusing on creating clear and measurable value for all stakeholders, businesses can position themselves for long-term success in an increasingly value-driven pharmaceutical market.
Navigating the Evolving Regulatory and Competitive Landscape
The regulatory and competitive landscape surrounding pharmaceutical drug pricing is in a constant state of flux, with new policies and market dynamics emerging regularly. Recent legislative changes, such as the Inflation Reduction Act in the United States, and the growing global pressure for increased price transparency are significantly reshaping the dynamics of the pharmaceutical market. It is therefore imperative for businesses to stay well-informed about these ongoing changes and to thoroughly understand their potential impact on their current pricing strategies and their ability to access key markets around the world. In addition to monitoring the regulatory environment, it is equally essential for businesses to keep a close watch on the competitive landscape. This includes continuously analyzing the pricing strategies of their direct competitors, as well as anticipating the potential entry of generic and biosimilar versions of their own products and those of their competitors. By proactively adapting to these changes in both the regulatory and competitive environments and by developing flexible and responsive pricing models, businesses can effectively mitigate potential risks to their profitability and capitalize on emerging opportunities within the dynamic pharmaceutical market.
Works cited
- Pharma Pricing Strategies – Supra, accessed April 9, 2025, https://supra.tools/pharma-pricing-strategies
- Drug pricing mechanisms | Wiki – FreedomGPT, accessed April 9, 2025, https://www.freedomgpt.com/wiki/drug-pricing-mechanisms
- Six drug pricing models have emerged to improve product access and affordability – PwC, accessed April 9, 2025, https://www.pwc.com/us/en/industries/health-industries/library/6-drug-pricing-models.html
- International reference pricing for prescription drugs: a landscape analysis – PMC, accessed April 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10391192/
- International Prescription Drug Price Comparisons: Estimates Using 2022 Data – NCBI, accessed April 9, 2025, https://www.ncbi.nlm.nih.gov/books/n/aspehpcomparerx/international/?report=reader
- Comparing Prescription Drugs in the U.S. and Other Countries: Prices and Availability, accessed April 9, 2025, https://aspe.hhs.gov/reports/comparing-prescription-drugs
- International Prescription Drug Price Comparisons – RAND Corporation, accessed April 9, 2025, https://www.rand.org/pubs/research_reports/RRA788-3.html
- International Prescription Drug Price Comparisons: Estimates Using 2022 Data – PMC, accessed April 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11147645/
- Biden Is Right. The US Generally Pays Double That of Other Countries for Rx Drugs., accessed April 9, 2025, https://kffhealthnews.org/news/article/fact-check-biden-prescription-drug-prices-nation-comparison/
- International Drug Pricing | ASPE – HHS.gov, accessed April 9, 2025, https://aspe.hhs.gov/topics/prescription-drugs-other-medical-products/international-drug-pricing
- Value-Based Pricing of Prescription Drugs Benefits Patients and Promotes Innovation, accessed April 9, 2025, https://www.americanprogress.org/article/value-based-pricing-prescription-drugs-benefits-patients-promotes-innovation/
- Deconstructing Drug Pricing Strategy for Big Pharma …, accessed April 9, 2025, https://www.drugpatentwatch.com/blog/deconstructing-drug-pricing-strategy-for-big-pharma/
- Cost-Plus Pricing Expert Guide – NetSuite, accessed April 9, 2025, https://www.netsuite.com/portal/resource/articles/financial-management/cost-plus-pricing.shtml
- What is cost-plus pricing? Definition, Formula, & Examples – Paddle, accessed April 9, 2025, https://www.paddle.com/blog/cost-plus-pricing
- What Is Cost Plus Pricing? How Do You Use It In Sales? – Salesforce, accessed April 9, 2025, https://www.salesforce.com/blog/cost-plus-pricing/
- The 6 Disadvantages of Cost-Plus Pricing – Blog – BlackCurve, accessed April 9, 2025, https://blog.blackcurve.com/6-reasons-why-cost-plus-pricing-is-harming-your-company
- The Advantages and Disadvantages of Cost-Plus Pricing – GoCardless, accessed April 9, 2025, https://gocardless.com/guides/posts/the-advantages-and-disadvantages-of-cost-plus-pricing/
- Cost Plus Drugs: Prescription for Success – Ivey Business Review, accessed April 9, 2025, https://www.iveybusinessreview.ca/magazine/articles/cost-plus-drugs-prescription-for-success
- Health Cost IQ and Cost Plus Team Up to Address Soaring Medical Costs – Business Wire, accessed April 9, 2025, https://www.businesswire.com/news/home/20250408959745/en/Health-Cost-IQ-and-Cost-Plus-Team-Up-to-Address-Soaring-Medical-Costs
- exploring the impact of the Mark Cuban Cost Plus Drug Company model on Medicare savings – Journal of Men’s Health, accessed April 9, 2025, https://oss.jomh.org/files/article/20241230-446/pdf/JOMH2024092701.pdf
- Mark Cuban is making medication costs an easier pill to swallow | Graduate Studies | MUSC, accessed April 9, 2025, https://gradstudies.musc.edu/about/blog/2024/09/easier-pill-to-swallow
- Competition-Based Pricing: Advantages & Disadvantages – Flintfox, accessed April 9, 2025, https://www.flintfox.com/resources/articles/competition-based-pricing-guide/
- Competitor-Based Pricing Expert Guide – NetSuite, accessed April 9, 2025, https://www.netsuite.com/portal/resource/articles/business-strategy/competitor-based-pricing.shtml
- Competitive Pricing Strategy Explained: The Pros & Cons – Pricefx, accessed April 9, 2025, https://www.pricefx.com/learning-center/competitive-pricing-strategy-explained-the-pros-cons
- Market-based Pricing | Pros & Cons | SBI Growth, accessed April 9, 2025, https://sbigrowth.com/insights/market-based-pricing
- Factors Impacting Pharmaceutical Prices and Affordability: Narrative Review – PMC, accessed April 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7838942/
- Does Pharmaceutical Reference Pricing Have a Future in the U.S.? | Commonwealth Fund, accessed April 9, 2025, https://www.commonwealthfund.org/publications/issue-briefs/2018/sep/pharmaceutical-reference-pricing-future
- What Should US Policymakers Learn From International Drug Pricing Transparency Strategies? – AMA Journal of Ethics, accessed April 9, 2025, https://journalofethics.ama-assn.org/article/what-should-us-policymakers-learn-international-drug-pricing-transparency-strategies/2022-11
- What Other Countries Could Teach the U.S. About Bringing Down Drug Prices, accessed April 9, 2025, https://www.gsb.stanford.edu/insights/what-other-countries-could-teach-us-about-bringing-down-drug-prices
- International Pricing Index (IPI) Model – CMS, accessed April 9, 2025, https://www.cms.gov/priorities/innovation/innovation-models/ipi-model
- Creating a stable drug pricing strategy in an unstable global market – PwC, accessed April 9, 2025, https://www.pwc.com/us/en/industries/health-industries/health-research-institute/creating-a-stable-drug-pricing-strategy.html
- PBM 101: PBM Pricing Models – Innovative Rx Strategies, accessed April 9, 2025, https://innovativerxstrategies.com/pbm-pricing-models/
- How Pharmaceutical Companies Price Their Drugs – Investopedia, accessed April 9, 2025, https://www.investopedia.com/articles/investing/020316/how-pharmaceutical-companies-price-their-drugs.asp
- 5 Factors That Affect Drug Pricing – Healthcare Weekly, accessed April 9, 2025, https://healthcareweekly.com/5-factors-that-affect-drug-pricing/
- The Rising Cost of Prescriptions: Unveiling the Causes and Potential Solutions, accessed April 9, 2025, https://www.nomihealth.com/blog/the-rising-cost-of-prescriptions
- Prescription Drug Spending in the U.S. Health Care System, accessed April 9, 2025, https://www.actuary.org/content/prescription-drug-spending-us-health-care-system
- Factors Influencing Affordability – Making Medicines Affordable – NCBI Bookshelf, accessed April 9, 2025, https://www.ncbi.nlm.nih.gov/books/NBK493090/
- Selected Issues in Pharmaceutical Drug Pricing – CRS Products from the Library of Congress, accessed April 9, 2025, https://crsreports.congress.gov/product/pdf/IF/IF12272
- Generic Competition and Drug Prices | FDA, accessed April 9, 2025, https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/generic-competition-and-drug-prices
- Explaining the Prescription Drug Provisions in the Inflation Reduction Act – KFF, accessed April 9, 2025, https://www.kff.org/medicare/issue-brief/explaining-the-prescription-drug-provisions-in-the-inflation-reduction-act/
- Affordability is about more than drug prices – AmerisourceBergen, accessed April 9, 2025, https://www.amerisourcebergen.com/-/media/assets/xcenda/english/content-assets/white-papers-issue-briefs-studies-pdf/xcenda-payer-reaction-to-govt-price-regulation-july-2021.pdf
- Policy Options to Reduce Prescription Drug Costs | Department of Medicine News, accessed April 9, 2025, https://medicine.stanford.edu/news/current-news/standard-news/policy-options-white-paper.html
- Government regulated or negotiated drug prices: Key design considerations, accessed April 9, 2025, https://www.brookings.edu/articles/government-regulated-or-negotiated-drug-prices-key-design-considerations/
- Balancing Ethical and Fiduciary Responsibilities in Drug Pricing – Pharma’s Almanac, accessed April 9, 2025, https://www.pharmasalmanac.com/articles/balancing-ethical-and-fiduciary-responsibilities-in-drug-pricing
- Ethical Drug Pricing – The Hastings Center, accessed April 9, 2025, https://www.thehastingscenter.org/briefingbook/ethical-drug-pricing/
- Understanding Drug Pricing – U.S. Pharmacist, accessed April 9, 2025, https://www.uspharmacist.com/article/understanding-drug-pricing
- How are prescription drug prices determined? – American Medical Association, accessed April 9, 2025, https://www.ama-assn.org/delivering-care/public-health/how-are-prescription-drug-prices-determined
- Drug Costs and Their Impact on Care | Arnold Ventures, accessed April 9, 2025, https://www.arnoldventures.org/stories/drug-costs-and-their-impact-on-care
- How Patient Cost-Sharing Trends Affect Adherence and Outcomes: A Literature Review, accessed April 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3278192/
- New Report Shows Impact of Rising Drug Prices and Drug Shortages on Patients and Hospitals | AHA, accessed April 9, 2025, https://www.aha.org/press-releases/2019-01-15-new-report-shows-impact-rising-drug-prices-and-drug-shortages-patients
- High Drug Prices and Patient Costs: Millions of Lives and Billions of Dollars Lost – CIDSA, accessed April 9, 2025, https://www.cidsa.org/publications/xcenda-summary
- Drug Prices and Shortages Jeopardize Patient Access to Quality Hospital Care | AHA News, accessed April 9, 2025, https://www.aha.org/news/blog/2024-05-22-drug-prices-and-shortages-jeopardize-patient-access-quality-hospital-care
- The Effect of Drug Pricing Policies on Healthcare Equity and Affordability, accessed April 9, 2025, https://www.jbclinpharm.org/articles/the-effect-of-drug-pricing-policies-on-healthcare-equity-and-affordability-13081.html
- The Impact of Drug Pricing Policies on Patient Access in 2025 – Drugzone Pharmaceuticals, accessed April 9, 2025, https://www.drugzone.com/blog/the-impact-of-drug-pricing-policies-on-patient-access-in-2025
- Effect of Value-Based Drug Pricing on Patient Health Outcomes – Lyfegen, accessed April 9, 2025, https://www.lyfegen.com/post/the-effect-of-value-based-drug-pricing-on-patient-health-outcomes-more-of-whats-needed-efficacy-access-and-affordability
- Prescription Drug Costs | Pros, Cons, Debate, Arguments, Economy, Laws, Government, & Regulation | Britannica, accessed April 9, 2025, https://www.britannica.com/procon/prescription-drug-costs-debate
- CDC Report: 9 Million Americans Not Taking Medications as Prescribed Due to Cost, accessed April 9, 2025, https://www.health.com/drug-costs-united-states-cdc-7509659
- Characteristics of Adults Aged 18–64 Who Did Not Take Medication as Prescribed to Reduce Costs: United States, 2021 – CDC, accessed April 9, 2025, https://www.cdc.gov/nchs/data/databriefs/db470.pdf
- The Effect of Reference Pricing on Pharmaceutical Innovation – CSIS, accessed April 9, 2025, https://www.csis.org/blogs/perspectives-innovation/effect-reference-pricing-pharmaceutical-innovation
- Regulated drug pricing in the US | Roland Berger, accessed April 9, 2025, https://www.rolandberger.com/en/Insights/Publications/US-pharmaceutical-pricing-at-a-crossroads.html
- Full article: Pharmaceutical price regulation and its impact on drug innovation: mitigating the trade-offs – Taylor & Francis Online, accessed April 9, 2025, https://www.tandfonline.com/doi/full/10.1080/13543776.2021.1876029
- Drug Pricing Transparency: The New Retail Revolution – PMC, accessed April 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5345916/
- Why It Is Critical to Include Dynamic Drug Pricing in Cost-Effectiveness Analysis in a Post-IRA World | National Pharmaceutical Council, accessed April 9, 2025, https://www.npcnow.org/resources/why-it-critical-include-dynamic-drug-pricing-cost-effectiveness-analysis-post-ira-world
- Navigating the Inflation Reduction Act’s Impact on Drug Pricing and Innovation – Boston Consulting Group, accessed April 9, 2025, https://www.bcg.com/publications/2023/navigating-inflation-reduction-act-impact-on-drug-pricing-innovation
- The Truth About Innovation & Drug Prices, accessed April 9, 2025, https://www.patientsforaffordabledrugs.org/wp-content/uploads/2021/02/P4AD-Report-Innovation.V33.pdf
- The complexity of drug pricing requires a refreshed healthcare data strategy, accessed April 9, 2025, https://www.wolterskluwer.com/en/expert-insights/complexity-of-drug-pricing-requires-refreshed-healthcare-data-strategy
- US Drug Pricing and Reimbursement: Players, Payers, PBMs, and Prospects – A Conversation with Two Experts – DIA Global Forum, accessed April 9, 2025, https://globalforum.diaglobal.org/issue/february-2024/us-drug-pricing-and-reimbursement-players-payers-pbms-and-prospects-a-conversation-with-two-experts/
- Concentration of spending and share of specialty drug spending in Medicare Part D over a 10-year period, accessed April 9, 2025, https://www.jmcp.org/doi/10.18553/jmcp.2024.30.12.1355
- Trends in Prescription Drug Spending, 2016-2021 – ASPE, accessed April 9, 2025, https://aspe.hhs.gov/sites/default/files/documents/88c547c976e915fc31fe2c6903ac0bc9/sdp-trends-prescription-drug-spending.pdf
- The Price We Pay | Summary, Quotes, FAQ, Audio – SoBrief, accessed April 9, 2025, https://sobrief.com/books/the-price-we-pay
- International Prescription Drug Price Comparisons: Estimates Using 2022 Data, accessed April 9, 2025, https://aspe.hhs.gov/sites/default/files/documents/277371265a705c356c968977e87446ae/international-price-comparisons.pdf
- How Medicare Negotiated Drug Prices Compare to Other Countries – KFF, accessed April 9, 2025, https://www.kff.org/health-costs/issue-brief/how-medicare-negotiated-drug-prices-compare-to-other-countries/
- How Medicare negotiated drug prices compare to other countries, accessed April 9, 2025, https://www.healthsystemtracker.org/brief/how-medicare-negotiated-drug-prices-compare-to-other-countries/
- Prescription Drug Spending | U.S. GAO, accessed April 9, 2025, https://www.gao.gov/prescription-drug-spending
- Top Patient and Advocate Quotes for Pharma from eyeforpharma ’18, accessed April 9, 2025, https://syneoshealthcommunications.com/blog/top-patient-and-advocate-quotes-for-pharma-from-eyeforpharma-18
- Views Conflict on Trump’s Drug-Pricing Blueprint: Most Actions Face Political, Legal, and Technical Roadblocks – PubMed Central, accessed April 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6152698/
- Should Price or Product Be the Determinant in Pharmaceutical Competition?, accessed April 9, 2025, https://www.drugpatentwatch.com/blog/price-product-determinant-pharmaceutical-competition/
- National patient advocacy organizations come together to respond to the HHS blueprint to lower drug prices and reduce out-of-pocket (OOP) Costs – PAN Foundation, accessed April 9, 2025, https://www.panfoundation.org/national-patient-advocacy-organizations-come-together-to-respond-to-the-hhs-blueprint-to-lower-drug-prices-and-reduce-out-of-pocket-oop-costs/
- Changes in the List Prices of Prescription Drugs, 2017-2023 | ASPE, accessed April 9, 2025, https://aspe.hhs.gov/reports/changes-list-prices-prescription-drugs
- Pharma to raise prices on more than 250 drugs in the US from January 2025, accessed April 9, 2025, https://www.pharmaceutical-technology.com/analyst-comment/pharma-prices-more-than-250-drugs-us-january-2025/
- A Value-Based Approach to America’s Costly Prescription Drug Problem, accessed April 9, 2025, https://www.commonwealthfund.org/blog/2022/value-based-approach-americas-costly-prescription-drug-problem
- Case Study: Pharmaceutical Pricing and Innovation – July 18, 2018 – USC Schaeffer Center, accessed April 9, 2025, https://schaeffer.usc.edu/research/case-study-pharmaceutical-pricing-and-innovation/
- Competition and price among brand-name drugs in the same class: A systematic review of the evidence – PubMed Central, accessed April 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6667132/
- Small Molecule Drug Reimbursement Case Study PHARMACON Company – NIH’s Seed, accessed April 9, 2025, https://seed.nih.gov/sites/default/files/2023-12/Drug-Reimbursement-Case-Study-1-Small-Molecule.pdf