A revolutionary force is reshaping the way we approach drug discovery and medical advancements. This force, known as deep learning, is a subset of artificial intelligence that has the potential to revolutionize the entire healthcare industry. From accelerating drug development processes to enhancing diagnostic accuracy, deep learning is proving to be an indispensable tool in the hands of researchers and medical professionals alike.
The Dawn of Deep Learning in Healthcare
Deep learning, a sophisticated branch of machine learning, has emerged as a game-changer in the realm of drug discovery and medicine. This powerful technology mimics the intricate workings of the human brain, utilizing artificial neural networks to process vast amounts of data and extract meaningful patterns. As we delve into the world of deep learning in healthcare, we’ll uncover its transformative potential and the myriad ways it’s reshaping the landscape of medical research and patient care.
Understanding Deep Learning: A Brief Overview
Before we dive deeper into its applications in drug discovery and medicine, let’s take a moment to understand what deep learning really is. At its core, deep learning is a subset of machine learning that employs artificial neural networks with multiple layers. These networks are designed to automatically learn and improve from experience, much like the human brain.
“Deep learning is making major advances in solving problems that have resisted the best attempts of the artificial intelligence community for many years.” – Geoffrey Hinton, University of Toronto
The key difference between deep learning and traditional machine learning lies in its ability to automatically learn features from raw data. While traditional machine learning algorithms require human experts to define the features to be learned, deep learning algorithms can discover these features on their own, making them particularly suited for complex tasks in healthcare and drug discovery.
The Intersection of Deep Learning and Healthcare
The marriage of deep learning and healthcare has given birth to a new era of possibilities. From analyzing medical images with unprecedented accuracy to predicting patient outcomes based on complex datasets, deep learning is revolutionizing every aspect of the healthcare industry.
In the realm of drug discovery, deep learning algorithms are capable of sifting through vast libraries of chemical compounds, identifying potential drug candidates with remarkable speed and accuracy. This not only accelerates the drug discovery process but also has the potential to significantly reduce the costs associated with bringing new drugs to market.
Deep Learning in Drug Discovery: A Paradigm Shift
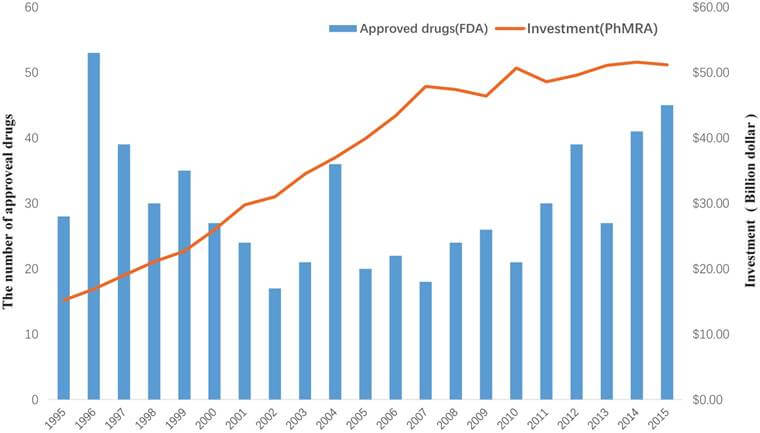
The pharmaceutical industry has long been plagued by the high costs and lengthy timelines associated with drug discovery. Traditional methods of drug development can take up to 15 years and cost billions of dollars, with no guarantee of success. Enter deep learning, a technology that promises to revolutionize this process, making it faster, more efficient, and potentially more successful.
Accelerating the Drug Discovery Pipeline
One of the most significant impacts of deep learning in drug discovery is its ability to dramatically speed up the initial stages of the process. By analyzing vast databases of chemical compounds and their properties, deep learning algorithms can identify potential drug candidates in a fraction of the time it would take human researchers.
These algorithms can predict how different molecules might interact with specific targets in the body, helping researchers focus their efforts on the most promising compounds. This targeted approach not only saves time but also reduces the likelihood of late-stage failures in clinical trials, which are often the most expensive part of the drug development process.
Predicting Drug-Target Interactions
Understanding how a drug interacts with its target in the body is crucial for predicting its efficacy and potential side effects. Deep learning models have shown remarkable accuracy in predicting these drug-target interactions, often outperforming traditional computational methods.
By analyzing the structural and chemical properties of both drugs and their targets, these models can predict binding affinities and potential off-target effects. This capability is particularly valuable in the early stages of drug discovery, helping researchers identify and prioritize the most promising candidates for further investigation.
De Novo Drug Design
Perhaps one of the most exciting applications of deep learning in drug discovery is in the field of de novo drug design. This approach involves using AI to design entirely new molecules with desired properties, rather than screening existing compounds.
Deep learning models can be trained on vast libraries of known drugs and their properties, learning the underlying patterns that make a molecule effective. These models can then generate novel molecular structures that are optimized for specific targets or properties, potentially leading to the discovery of entirely new classes of drugs.
Deep Learning in Medical Imaging: Enhancing Diagnostic Accuracy
Medical imaging is another area where deep learning is making significant strides. From X-rays to MRIs, deep learning algorithms are enhancing the accuracy and speed of image analysis, potentially leading to earlier and more accurate diagnoses.
Revolutionizing Radiology
In the field of radiology, deep learning algorithms have shown remarkable ability in detecting and classifying various abnormalities in medical images. These algorithms can analyze images with a level of detail and consistency that surpasses human capabilities, potentially catching subtle signs of disease that might be missed by even experienced radiologists.
For example, deep learning models have been developed that can detect early signs of breast cancer in mammograms with accuracy comparable to human experts. These models can analyze thousands of images in a fraction of the time it would take a human radiologist, potentially leading to earlier diagnoses and improved patient outcomes.
Enhancing Brain Imaging
In the realm of neurology, deep learning is revolutionizing the analysis of brain scans. Advanced algorithms can detect subtle changes in brain structure and function that may indicate the early stages of neurodegenerative diseases like Alzheimer’s or Parkinson’s.
These algorithms can also assist in the planning and execution of complex neurosurgeries. By analyzing brain scans and other patient data, deep learning models can help surgeons identify the safest and most effective approach for procedures, potentially improving outcomes and reducing complications.
Personalized Medicine: Tailoring Treatments with Deep Learning
One of the most promising applications of deep learning in medicine is in the field of personalized medicine. By analyzing vast amounts of patient data, including genetic information, lifestyle factors, and treatment histories, deep learning algorithms can help predict which treatments are likely to be most effective for individual patients.
Predicting Treatment Responses
Deep learning models can analyze a patient’s genetic profile, along with other relevant data, to predict how they might respond to different treatments. This capability is particularly valuable in oncology, where the effectiveness of cancer treatments can vary widely between patients.
For example, researchers have developed deep learning models that can predict patient responses to immunotherapy based on their genetic profiles and other clinical data. These models could help oncologists make more informed decisions about treatment plans, potentially improving outcomes and reducing unnecessary side effects.
Optimizing Drug Dosages
Another application of deep learning in personalized medicine is in optimizing drug dosages. By analyzing patient data and treatment responses, deep learning algorithms can help determine the optimal dosage for individual patients, balancing efficacy with the risk of side effects.
This approach is particularly valuable for drugs with narrow therapeutic windows, where the difference between an effective dose and a toxic one is small. By tailoring dosages to individual patients, deep learning could help improve treatment outcomes while minimizing adverse effects.
Challenges and Ethical Considerations
While the potential of deep learning in drug discovery and medicine is immense, it’s not without its challenges and ethical considerations. As we continue to integrate these powerful technologies into healthcare, it’s crucial that we address these issues head-on.
Data Privacy and Security
One of the primary concerns surrounding the use of deep learning in healthcare is data privacy and security. These algorithms require vast amounts of patient data to train effectively, raising questions about how this data is collected, stored, and used.
Ensuring the privacy and security of patient data is paramount. Healthcare organizations and researchers must implement robust security measures and adhere to strict ethical guidelines to protect patient information. This includes using techniques like federated learning, which allows models to be trained on decentralized data without compromising privacy.
Algorithmic Bias
Another significant challenge is the potential for algorithmic bias. If the data used to train deep learning models is not diverse or representative, it could lead to biased outcomes that disproportionately affect certain populations.
For example, if a model is trained primarily on data from one ethnic group, it may not perform as well when analyzing data from other groups. This could lead to disparities in diagnosis and treatment recommendations. To address this, it’s crucial that researchers use diverse, representative datasets and regularly audit their models for bias.
Interpretability and Explainability
The “black box” nature of many deep learning models poses another challenge, particularly in healthcare where understanding the reasoning behind a diagnosis or treatment recommendation is crucial. Efforts are underway to develop more interpretable deep learning models, but this remains an active area of research.
The Future of Deep Learning in Healthcare
As we look to the future, the potential applications of deep learning in drug discovery and medicine seem boundless. From developing new antibiotics to combat drug-resistant bacteria to creating personalized treatment plans based on an individual’s genetic profile, the possibilities are truly exciting.
Integrating Multi-Modal Data
One promising direction is the integration of multi-modal data in deep learning models. By combining data from various sources – genomics, imaging, electronic health records, and even wearable devices – we can create more comprehensive and accurate models of human health and disease.
Federated Learning and Privacy-Preserving AI
As concerns about data privacy continue to grow, techniques like federated learning are likely to become more prevalent. These approaches allow models to be trained on decentralized data, potentially enabling collaboration between institutions without compromising patient privacy.
AI-Augmented Healthcare Professionals
Rather than replacing healthcare professionals, the future of deep learning in medicine is likely to be one of augmentation. AI systems will work alongside doctors and researchers, enhancing their capabilities and allowing them to focus on the most complex and nuanced aspects of patient care.
Key Takeaways
- Deep learning is revolutionizing drug discovery and medicine, offering the potential to accelerate research, enhance diagnostic accuracy, and personalize treatments.
- In drug discovery, deep learning is speeding up the identification of potential drug candidates, predicting drug-target interactions, and even designing entirely new molecules.
- Medical imaging is being transformed by deep learning, with algorithms capable of analyzing images with unprecedented speed and accuracy.
- Personalized medicine is benefiting from deep learning’s ability to analyze vast amounts of patient data and predict treatment responses.
- While the potential is immense, challenges such as data privacy, algorithmic bias, and model interpretability must be addressed.
- The future of deep learning in healthcare is likely to involve the integration of multi-modal data, privacy-preserving techniques, and AI-augmented healthcare professionals.
FAQs
- What is deep learning and how does it differ from traditional machine learning?
Deep learning is a subset of machine learning that uses artificial neural networks with multiple layers. Unlike traditional machine learning, deep learning can automatically learn features from raw data without human intervention, making it particularly suited for complex tasks in healthcare and drug discovery. - How is deep learning accelerating the drug discovery process?
Deep learning accelerates drug discovery by rapidly analyzing vast databases of chemical compounds, predicting drug-target interactions, and even designing new molecules. This can significantly reduce the time and cost associated with identifying potential drug candidates. - What are some ethical concerns surrounding the use of deep learning in healthcare?
Key ethical concerns include data privacy and security, the potential for algorithmic bias, and the “black box” nature of some deep learning models which can make it difficult to understand how decisions are made. - Can deep learning replace healthcare professionals?
Rather than replacing healthcare professionals, deep learning is more likely to augment their capabilities. AI systems can handle routine tasks and data analysis, allowing healthcare professionals to focus on complex decision-making and patient care. - What is federated learning and why is it important in healthcare AI?
Federated learning is a technique that allows AI models to be trained on decentralized data without compromising privacy. This is particularly important in healthcare, where patient data privacy is crucial. It enables collaboration between institutions while keeping sensitive data secure.