I. Executive Summary
The Drug Price Competition and Patent Term Restoration Act of 1984, commonly known as the Hatch-Waxman Act, stands as a landmark piece of legislation that fundamentally reshaped the pharmaceutical landscape in the United States. This Act addressed critical concerns regarding both the affordability of medicines and the incentives for pharmaceutical innovation. By establishing a clear regulatory pathway for the approval of generic drugs and by providing mechanisms for patent term restoration, the Hatch-Waxman Act spurred the rapid growth of the generic drug industry while aiming to sustain innovation in the development of new therapies. This report examines the key provisions and objectives of the Act, its profound impact on generic drug approvals, the dramatic increase in generic market share, the substantial cost savings realized by the healthcare system, and the ongoing debate surrounding its effects on pharmaceutical innovation. Furthermore, it details the crucial role of the Food and Drug Administration (FDA) in regulating the generic drug industry post-Hatch-Waxman, explores significant amendments to the Act since its inception, and analyzes current trends and future outlook, considering the emergence of biosimilars and the influence of international competition. Ultimately, the Hatch-Waxman Act has proven to be a highly successful framework in balancing pharmaceutical innovation with the accessibility of affordable medicines, although ongoing challenges necessitate continuous evaluation and adaptation.
II. Introduction: Setting the Stage – The US Pharmaceutical Landscape Before 1984
Prior to the enactment of the Hatch-Waxman Act in 1984, the landscape of the US pharmaceutical industry presented significant hurdles to the widespread availability of generic drugs.1 Generic drug manufacturers faced a regulatory environment that lacked a clear and efficient approval process, often resulting in years of delay before generic competition could emerge, even when the capacity to produce these lower-cost alternatives existed.2 This was largely because the existing regulations required generic drugs to undergo the same extensive safety and efficacy testing, including costly and time-consuming clinical trials, as their brand-name counterparts.3 This requirement created substantial financial barriers for generic drug developers, effectively limiting their ability to enter the market. Consequently, the market penetration of generic drugs was notably low, with only about 19% of all prescriptions in the United States being filled with generics.1 Furthermore, generic competition for even the top-selling pharmaceutical drugs was limited, with only approximately 35% of such drugs having generic alternatives available after their patents expired.1 The regulatory framework at the time, primarily governed by the Food, Drug, and Cosmetic Act of 1962 (Kefauver-Harris Amendments), while increasing the regulatory authority of the FDA regarding drug safety and efficacy, also contributed to regulatory inefficiencies and slow drug approval times.3 The absence of a streamlined pathway for generic approvals meant that even after the patent protection on a brand-name drug had lapsed, it often took three to five years for a generic version to enter the market.1 This situation contributed to rising healthcare costs and limited patient access to more affordable medications. The high regulatory burden on generics, equivalent to that of novel drugs, acted as a significant disincentive for their market entry, effectively shielding brand-name drugs from competition long after their patent terms should have allowed for it.
III. The Hatch-Waxman Act of 1984: Key Provisions and Objectives
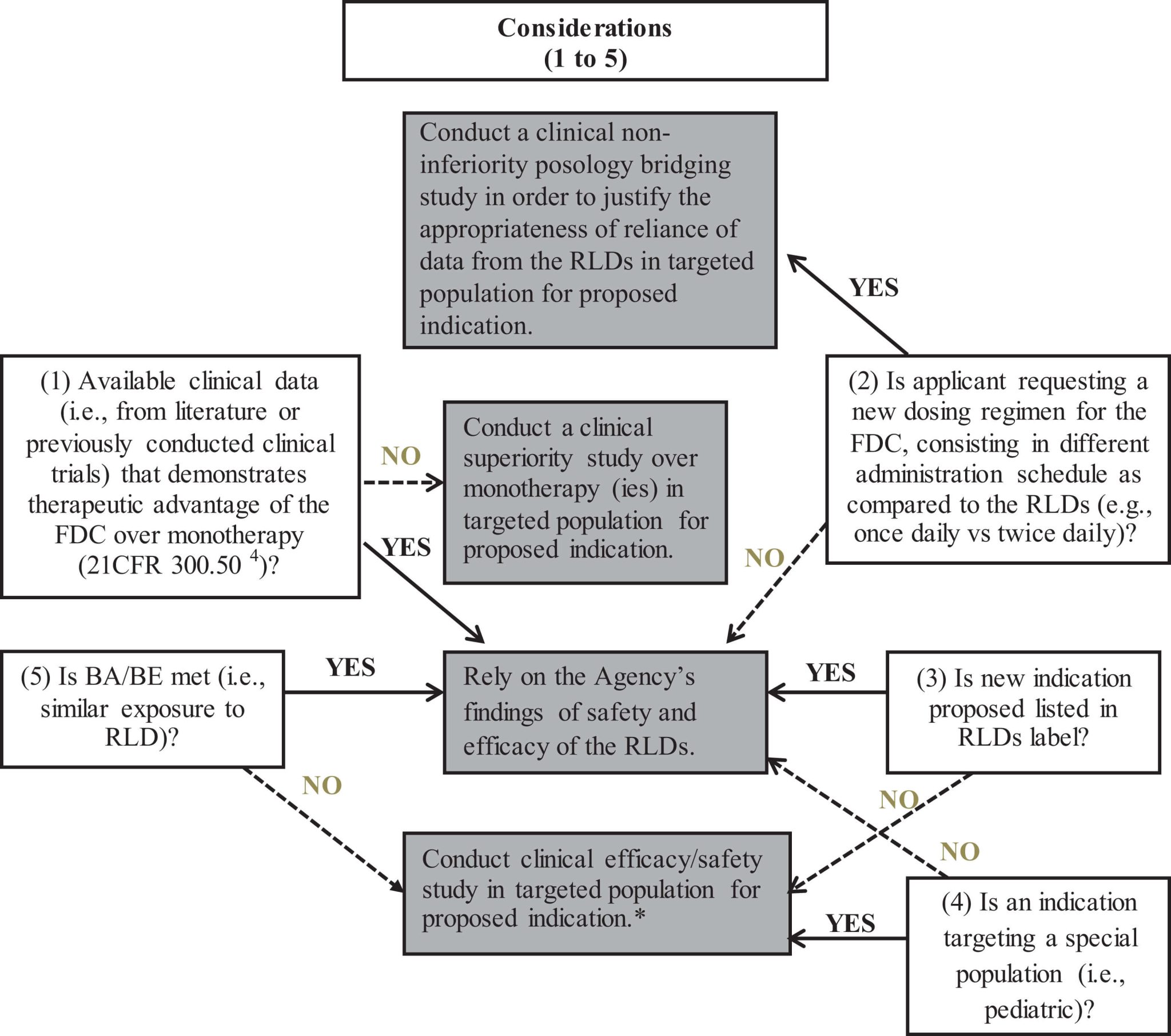
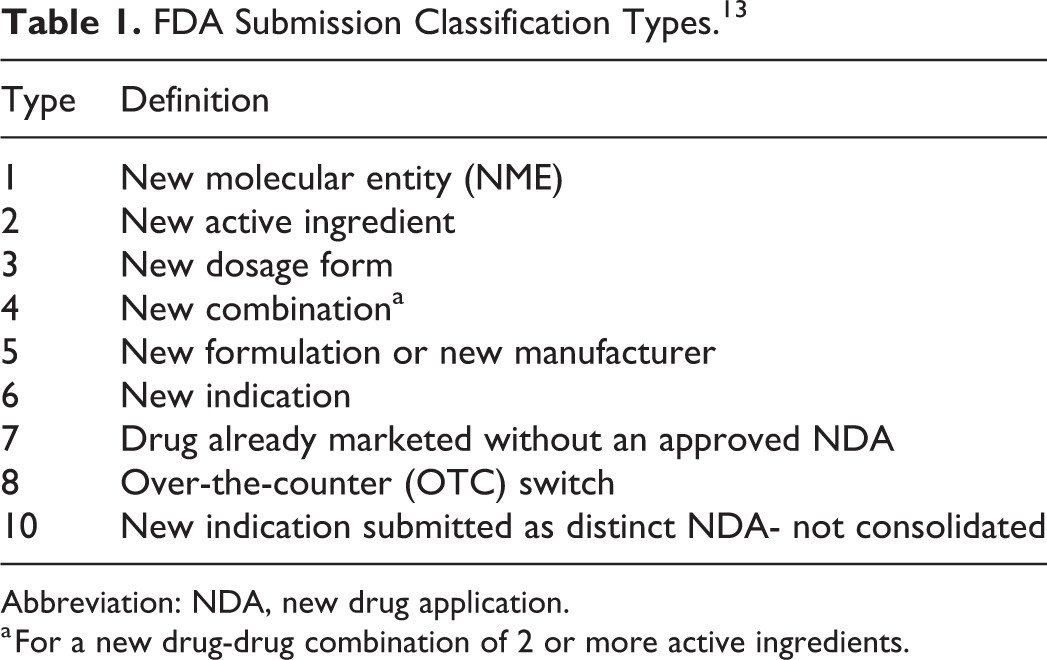
Recognizing the growing concerns around the affordability and accessibility of prescription drugs, Congress passed the Drug Price Competition and Patent Term Restoration Act in 1984.2 This bipartisan legislation, commonly known as the Hatch-Waxman Act, was the result of collaborative efforts between Senator Orrin Hatch and Representative Henry Waxman.2 The Act was designed with two primary objectives: to facilitate the more rapid entry of generic drugs into the market, thereby increasing competition and lowering drug prices, and to compensate the original drug developers for the time lost during the regulatory review process, thus sustaining incentives for pharmaceutical innovation.16 To achieve these goals, the Hatch-Waxman Act introduced several key provisions. One of the most significant was the creation of the Abbreviated New Drug Application (ANDA) pathway, outlined in Section 505(j) of the Federal Food, Drug, and Cosmetic Act.6 This pathway allowed generic manufacturers to seek FDA approval by demonstrating that their drug was bioequivalent to a previously approved brand-name drug, known as the Reference Listed Drug (RLD), without the need to repeat the extensive clinical trials that established the RLD’s safety and efficacy.1 This significantly reduced both the development costs and the time required for generic drugs to gain approval.15 The Act also established a framework for patent litigation through the Paragraph IV certification.1 This provision allowed generic companies to challenge patents held by brand-name drug manufacturers if they believed the patent was invalid or would not be infringed by their generic product.1 Filing a Paragraph IV certification could trigger a 30-month stay on the FDA’s approval of the generic drug if the brand-name company filed a patent infringement lawsuit.15 Furthermore, the Hatch-Waxman Act included a “safe harbor” provision that exempted generic manufacturers from patent infringement liability for activities undertaken to prepare an ANDA before the expiration of the brand-name drug’s patents.1 To further incentivize the entry of generics, the Act granted a 180-day market exclusivity period to the first generic manufacturer that successfully challenged a patent by filing a Paragraph IV certification and received FDA approval.1 In parallel with facilitating generic entry, the Act also aimed to incentivize pharmaceutical innovation. It provided for the restoration of a portion of the patent term that was lost due to the time taken for regulatory review by the FDA.1 Additionally, the Act introduced periods of market exclusivity for brand-name drugs, including a five-year exclusivity for new chemical entities 1, a three-year exclusivity for improved versions of previously approved drugs that required new clinical studies 1, and pediatric exclusivity.19 Finally, the Act mandated the creation of the FDA’s “Orange Book,” a publication that lists approved drug products along with information about their therapeutic equivalence and any associated patents.6 The Hatch-Waxman Act was a carefully constructed compromise aimed at achieving a balance between fostering a competitive generic drug market to drive down prices and preserving incentives for pharmaceutical companies to continue investing in the research and development of innovative new medicines.
IV. The Immediate and Long-Term Impact on Generic Drug Approvals in the US
The enactment of the Hatch-Waxman Act in 1984 had an immediate and profound impact on the number of generic drug approvals in the United States.13 In the year following its passage, the FDA received approximately 1,050 applications for new generic drugs, signaling a significant shift in the industry’s approach to market entry.13 The median annual number of generic drugs approved by the FDA rose substantially after 1984, indicating the Act’s effectiveness in streamlining the approval process.55 Over the long term, the trend of generic drug approvals continued to climb dramatically.10 In fiscal year 2019, for example, the FDA issued a record high of 1,171 generic drug approvals, including 935 full approvals and 236 tentative approvals.56 This represents a 20.5% increase over the previous year and a 134% increase since 2014.56 The number of Abbreviated New Drug Application (ANDA) submissions and subsequent approvals has shown a consistent upward trajectory over the decades, demonstrating the Act’s lasting influence on facilitating generic market access.10 The ANDA pathway, created by the Hatch-Waxman Act, has become the primary route for generic drug approval, enabling manufacturers to bring lower-cost alternatives to market more efficiently.6 This transformation of the generic drug approval landscape has been crucial in fostering a more competitive pharmaceutical market, ultimately benefiting patients through increased access to affordable medications.
V. The Ascendancy of Generics: Growth of Market Share Since 1984
Since the passage of the Hatch-Waxman Act, the United States has witnessed a remarkable surge in the utilization of generic drugs. The percentage of prescriptions filled with generic medications has increased dramatically from approximately 19% in 1984 to over 90% today.1 This growth positions the US as a global leader in generic uptake compared to other countries within the Organization for Economic Cooperation and Development (OECD).12 Generic drugs now constitute a significant portion of the total pharmaceutical market by volume.2 However, due to their substantially lower prices compared to brand-name drugs, generics account for a considerably smaller share of the total pharmaceutical spending.9 This dynamic underscores the profound impact of the Hatch-Waxman Act in facilitating the widespread use of more affordable medications.
VI. Economic Benefits: Cost Savings Attributed to Generic Drugs Post-Hatch-Waxman
The availability and use of generic drugs in the US healthcare system following the Hatch-Waxman Act have generated substantial cost savings for both the healthcare system and individual consumers.1 Over the past decades, these savings have amounted to trillions of dollars.3 In more recent years, the annual savings have been in the hundreds of billions; for instance, in 2023 alone, generic and biosimilar competition saved over $445 billion for American consumers.3 In 2021, the US health care system saved $373 billion through the use of FDA-approved generic and biosimilar drugs, with $119 billion in savings for Medicare and $48.5 billion for Medicaid in 2019.60 Generic drugs are typically much more affordable than their brand-name counterparts, often costing 30% to 80% less.4 The average copay for generic drugs is also significantly lower than that for brand-name drugs.3 Furthermore, the prices of generic drugs tend to decline even further as more generic manufacturers enter the market, increasing competition.5 The increased availability and affordability of generic drugs have played a crucial role in making essential medications more accessible to a wider population, thereby contributing to improved public health outcomes.
VII. Balancing Innovation and Affordability: The Act’s Impact on Pharmaceutical Innovation
The Hatch-Waxman Act was crafted to strike a balance between encouraging the development of innovative new drugs and promoting the availability of lower-cost generic alternatives. Proponents argue that the Act provides necessary incentives for pharmaceutical innovation through patent term extensions and periods of market exclusivity, allowing brand-name companies to recoup their significant R&D investments.1 The United States has indeed become a global leader in biopharmaceutical innovation since the Act’s passage 3, with biopharmaceutical companies bringing numerous new medicines to patients.2 However, critics contend that the Act’s facilitation of generic competition may reduce the financial returns for innovator companies, potentially diminishing the incentive to invest in the discovery and marketing of novel therapies.18 Concerns have also been raised about a perceived slowdown in the development of new small-molecule products in recent years 4, with some suggesting a shift towards reformulations of existing drugs rather than the creation of truly innovative treatments.4 Furthermore, brand-name companies have been observed employing various strategies to delay or even prevent generic market entry, such as building “patent thickets,” engaging in “reverse payment” settlements with generic challengers, and “product hopping” (making minor modifications to a drug to extend market exclusivity).19 These tactics, while potentially legal under the current framework, raise questions about whether the Act’s intended balance between innovation and affordability is being consistently maintained.
VIII. The FDA’s Role in Regulating the Post-Hatch-Waxman Generic Drug Industry
The Food and Drug Administration (FDA) plays a critical role in regulating the generic drug industry in the United States following the implementation of the Hatch-Waxman Act. The FDA is responsible for ensuring that all approved generic drugs meet stringent standards for safety, efficacy, and quality.1 A primary function of the FDA is managing the Abbreviated New Drug Application (ANDA) approval process.1 This involves a rigorous review to ensure bioequivalence between the generic drug and the brand-name drug it seeks to replicate.4 The FDA also publishes the “Orange Book,” which serves as a comprehensive resource listing approved drugs and their therapeutic equivalence evaluations, aiding in the substitution of generic drugs for brand-name products.6 Beyond the initial approval, the FDA conducts post-market surveillance to monitor the quality and safety of generic drugs already on the market.76 Recognizing the importance of generic competition in lowering drug prices, the FDA has also implemented initiatives like the Drug Competition Action Plan (DCAP) to help remove barriers to generic drug development and market entry, thereby addressing drug shortages.56 Furthermore, the FDA plays a role in the patent certification process outlined in the Hatch-Waxman Act, reviewing patent information submitted by brand-name companies and managing the certifications provided by generic applicants, which can lead to patent disputes and litigation.15
IX. Evolution Through Amendments: Significant Updates to the Act and Their Consequences
Since its enactment in 1984, the Hatch-Waxman Act has been subject to several significant amendments and updates to address evolving issues within the pharmaceutical industry. One notable amendment was the Generic Drug Enforcement Act of 1992.10 This legislation introduced debarment penalties for individuals and companies convicted of felonies or misdemeanors related to the development or approval of generic drugs, aiming to ensure the integrity of the ANDA approval process. Another key update was the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA).13 The MMA sought to close perceived loopholes in the Hatch-Waxman Act that were being used to delay the market entry of generic drugs. It addressed issues such as the listing of multiple patents in the Orange Book to trigger successive 30-month stays on generic approvals and aimed to prevent anti-competitive agreements between brand-name and generic drug manufacturers. More recently, the Generic Drug User Fee Amendments (GDUFA) of 2012 and its subsequent reauthorizations (GDUFA II in 2017 and GDUFA III in 2022) have had a significant impact on the generic drug industry.6 GDUFA provided the FDA with additional resources, funded through user fees paid by the generic drug industry, to enhance the efficiency and predictability of the review process for generic drug applications. This has led to a notable reduction in ANDA review times and an increase in the number of generic drug approvals.56 These amendments collectively reflect the ongoing efforts to refine the Hatch-Waxman framework and ensure its continued effectiveness in promoting both generic drug access and pharmaceutical innovation.
X. The Present and the Horizon: Current Trends, Challenges, and Future Outlook
The US generic drug industry today is characterized by several key trends. Generic drug utilization rates remain exceptionally high, exceeding 90% of all prescriptions filled.1 There is a persistent focus on cost containment within the healthcare system, further driving the demand for affordable generic options.1 The biosimilars market, inspired by the framework of the Hatch-Waxman Act, is also experiencing significant growth.2 The industry faces increasing international competition, particularly from manufacturers in India and China.15 Market consolidation among both generic drug manufacturers and buyers is also a notable trend.19 Furthermore, there is a growing focus on the development and approval of complex generics and value-added generic products.6 Despite these trends, the industry faces several challenges. Unchecked price deflation and low profit margins are creating economic pressures on manufacturers 19, leading to an increased risk of drug shortages due to economic unsustainability and vulnerabilities in the global supply chain.19 The adoption of biosimilars in the US has been slower than anticipated due to various economic and non-economic barriers.19 The complex regulatory landscape and evolving FDA requirements also pose ongoing challenges for generic drug manufacturers.10 Furthermore, strategies employed by brand-name companies, such as patent thickets, continue to present obstacles to timely generic market entry.19 Looking ahead, the generic drug industry is expected to continue to grow, driven by the ongoing expiration of patents on blockbuster drugs and the persistent demand for more affordable medications.73 Biosimilars are anticipated to play an increasingly significant role in the pharmaceutical market.19 There is also potential for further policy adjustments and legislative reforms aimed at addressing the current challenges and ensuring the long-term sustainability of generic drug access and pharmaceutical innovation.19 The impact of international drug pricing and global trade policies will also continue to shape the dynamics of the US generic drug market.19
XI. Conclusion: Reflecting on Four Decades of the Hatch-Waxman Act
The Hatch-Waxman Act of 1984 has played a transformative role in the development of the US generic drug industry. It established the essential legal and regulatory framework that enabled the widespread availability of affordable generic medicines, leading to significant cost savings for patients and the healthcare system. The Act successfully fostered a competitive pharmaceutical market by creating a streamlined approval pathway for generics while simultaneously providing incentives for the innovation of new brand-name drugs. Over the past four decades, generic drug utilization has soared, and the US has become a global leader in this sector. However, the industry continues to face challenges related to pricing pressures, supply chain vulnerabilities, and the evolving landscape of pharmaceutical innovation, including the rise of biosimilars and the influence of international competition. Addressing these challenges will require ongoing adaptation, policy adjustments, and a continued commitment to the core principles of the Hatch-Waxman Act: balancing access to affordable medicines with the need to incentivize the development of innovative therapies. The Act’s lasting legacy lies in its fundamental contribution to public health by making essential medicines more accessible and affordable for millions of Americans.
Works cited
- WHAT IS HATCH-WAXMAN? – PhRMA, accessed April 10, 2025, https://www.phrma.org/-/media/Project/PhRMA/PhRMA-Org/PhRMA-Org/PDF/D-F/Fact-Sheet_What-is-Hatch-Waxman_June-2018.pdf
- 40 Years of Hatch-Waxman: What is the Hatch-Waxman Act? | PhRMA, accessed April 10, 2025, https://phrma.org/blog/40-years-of-hatch-waxman-what-is-the-hatch-waxman-act
- A Bipartisan Success: Celebrating 40 Years of the Hatch-Waxman Act, accessed April 10, 2025, https://www2.itif.org/2025-hatch-waxman-act-article.pdf
- Seizing the Opportunity – PMC, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4115321/
- The Hatch-Waxman 180-Day Exclusivity Incentive Accelerates Patient Access to First Generics, accessed April 10, 2025, https://accessiblemeds.org/resources/fact-sheets/the-hatch-waxman-180-day-exclusivity-incentive-accelerates-patient-access-to-first-generics/
- 40th Anniversary of the Generic Drug Approval Pathway – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/cder-conversations/40th-anniversary-generic-drug-approval-pathway
- IP Explained: How Hatch-Waxman successfully balances affordability and innovation, accessed April 10, 2025, https://phrma.org/blog/ip-explained-how-hatch-waxman-successfully-balances-affordability-and-innovation
- Thirty years of generics in the US, accessed April 10, 2025, https://www.gabionline.net/generics/general/Thirty-years-of-generics-in-the-US
- GENERIC DRUGS IN THE UNITED STATES: POLICIES TO ADDRESS PRICING AND COMPETITION, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6355356/
- 30-Years-Generics – C&EN – American Chemical Society, accessed April 10, 2025, https://cen.acs.org/articles/92/i39/30-Years-Generics.html
- HOW INCREASED COMPETITION FROM GENERIC DRUGS HAS AFFECTED PRICES AND RETURNS IN THE PHARMACEUTICAL INDUSTRY JULY 1998 – Congressional Budget Office, accessed April 10, 2025, https://www.cbo.gov/sites/default/files/105th-congress-1997-1998/reports/pharm.pdf
- 40 Years of Hatch-Waxman: How does the Hatch-Waxman Act help patients? | PhRMA, accessed April 10, 2025, https://phrma.org/blog/40-years-of-hatch-waxman-how-does-the-hatch-waxman-act-help-patients
- Timeline: Generic medicines in the US | USP, accessed April 10, 2025, https://www.usp.org/our-impact/generics/timeline-of-generics-in-us
- A Bipartisan Success: Celebrating 40 Years of the Hatch-Waxman Act | ITIF, accessed April 10, 2025, https://itif.org/publications/2025/02/03/a-bipartisan-success-celebrating-40-years-of-the-hatch-waxman-act/
- What is Hatch-Waxman Act? – DDReg Pharma, accessed April 10, 2025, https://www.ddregpharma.com/what-is-hatch-waxman-act
- Drug Price Competition and Patent Term Restoration Act – Wikipedia, accessed April 10, 2025, https://en.wikipedia.org/wiki/Drug_Price_Competition_and_Patent_Term_Restoration_Act
- crsreports.congress.gov, accessed April 10, 2025, https://crsreports.congress.gov/product/pdf/R/R44643#:~:text=Through%20amendments%20to%20both%20the,firms%20with%20incentives%20to%20innovate.
- Breakthrough Therapy and the Hatch-Waxman Act – U.S. Pharmacist, accessed April 10, 2025, https://www.uspharmacist.com/article/breakthrough-therapy-and-the-hatchwaxman-act
- The Hatch-Waxman Act Turns 40: The Law That Made Biosimilars Possible, accessed April 10, 2025, https://www.centerforbiosimilars.com/view/the-hatch-waxman-act-turns-40-the-law-that-made-biosimilars-possible
- The Hatch-Waxman Act–25 Years Later: Keeping the Pharmaceutical Scales Balanced, accessed April 10, 2025, https://www.pharmacytimes.com/view/generic-hatchwaxman-0809
- Hatch-Waxman Letters – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/abbreviated-new-drug-application-anda/hatch-waxman-letters
- Drug Price Competition and Patent Term Restoration Act – Taylor & Francis, accessed April 10, 2025, https://taylorandfrancis.com/knowledge/Medicine_and_healthcare/Pharmaceutical_medicine/Drug_Price_Competition_and_Patent_Term_Restoration_Act/
- H.R.3605 – 98th Congress (1983-1984): Drug Price Competition and Patent Term Restoration Act of 1984, accessed April 10, 2025, https://www.congress.gov/bill/98th-congress/house-bill/3605
- A Closer Look at the Hatch-Waxman Act’s Impact on Drug Approval – The Knowledge Group, accessed April 10, 2025, https://knowledgewebcasts.com/a-closer-look-at-the-hatch-waxman-acts-impact-on-drug-approval/
- (PDF) EVALUATING THE HATCH-WAXMAN AMENDMENT’S INFLUENCE ON FDA’S GENERIC MEDICATION APPROVAL PROCESS – ResearchGate, accessed April 10, 2025, https://www.researchgate.net/publication/365356211_EVALUATING_THE_HATCH-WAXMAN_AMENDMENT’S_INFLUENCE_ON_FDA’S_GENERIC_MEDICATION_APPROVAL_PROCESS
- Generic Drugs: History, Approval Process, and Current Challenges – U.S. Pharmacist, accessed April 10, 2025, https://www.uspharmacist.com/article/generic-drugs-history-approval-process-and-current-challenges
- SUMMARY OF FEDERAL LAWS WITH PARTICULAR EFFECTS ON THE U.S. GENERIC DRUG INDUSTRY, accessed April 10, 2025, http://fbaum.unc.edu/lobby/002_Patent_Extension/Organizational_Statements/NAPM/Summary_of_Federal_Laws.htm
- Steven Adamson* Generic drugs have provided considerable cost-savings to consumers. The Hatch-Waxman Act provides economic incen, accessed April 10, 2025, https://www.luc.edu/media/lucedu/law/students/publications/clr/pdfs/30-2/15.Adamson(ed.2)%20copy.pdf
- COST OF GENERIC DRUG DEVELOPMENT AND APPROVAL FINAL – ASPE, accessed April 10, 2025, https://aspe.hhs.gov/sites/default/files/documents/20e14b66420440b9e726c61d281cc5a5/cost-of-generic-drugs-erg.pdf
- The Benefits and Effects of Hatch- Waxman Act Four Decades Later | Patexia, accessed April 10, 2025, https://patexia.com/feed/the-benefits-and-effects-of-hatch-waxman-act-four-decades-later-20220727
- Hatch-Waxman Related Provisions of the Medicare Prescription Drug Bills (H.R. 1 and S. 1) – UM Carey Law, accessed April 10, 2025, https://www2.law.umaryland.edu/marshall/crsreports/crsdocuments/RL32003.pdf
- The Hatch-Waxman Act: A Primer – CRS Products from the Library of Congress, accessed April 10, 2025, https://crsreports.congress.gov/product/pdf/R/R44643
- Hatch-Waxman 101 – Fish & Richardson, accessed April 10, 2025, https://www.fr.com/insights/thought-leadership/blogs/hatch-waxman-101-3/
- THE SINKING SHIP OF THE HATCH-WAXMAN ACT “SAFE HARBOR” PATENT INFRINGEMENT DEFENSE: AN ARGUMENT FOR INCLUDING RESEARCH TOOLS – Law Review, accessed April 10, 2025, https://lawreview.syr.edu/wp-content/uploads/2024/07/Sullivan.pdf
- Hatch-Waxman Act – US Laws, Litigations and Benefits – Copperpod IP, accessed April 10, 2025, https://www.copperpodip.com/post/hatch-waxman-act-us-laws-litigations-and-benefits
- Earning Exclusivity: Generic Drug Incentives and the Hatch-‐Waxman Act1 C. Scott – Stanford Law School, accessed April 10, 2025, https://law.stanford.edu/index.php?webauth-document=publication/259458/doc/slspublic/ssrn-id1736822.pdf
- Small Business Assistance | 180-Day Generic Drug Exclusivity – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/cder-small-business-industry-assistance-sbia/small-business-assistance-180-day-generic-drug-exclusivity
- evaluating the hatch-waxman amendment’s influence on fda’s generic medication approval – Journal of Pharmaceutical Negative Results, accessed April 10, 2025, https://www.pnrjournal.com/index.php/home/article/download/2501/2149/3024
- Drug Price Competition and Patent Term Restoration Act – Corporate Counsel – FindLaw, accessed April 10, 2025, https://corporate.findlaw.com/intellectual-property/drug-price-competition-and-patent-term-restoration-act.html
- Approved Drug Products with Therapeutic Equivalence Evaluations | Orange Book – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/drug-approvals-and-databases/approved-drug-products-therapeutic-equivalence-evaluations-orange-book
- Orange Book Preface – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/development-approval-process-drugs/orange-book-preface
- Electronic Orange Book – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/fda-drug-info-rounds-video/electronic-orange-book
- Generic Drugs and The Orange Book – FDA, accessed April 10, 2025, https://www.fda.gov/media/94801/download
- Orange Book 101 | The FDA’s Official Register of Drugs, accessed April 10, 2025, https://www.fr.com/insights/ip-law-essentials/orange-book-101/
- Orange Book Data Files – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/drug-approvals-and-databases/orange-book-data-files
- Frequently Asked Questions on The Orange Book – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/drug-approvals-and-databases/frequently-asked-questions-orange-book
- Orange Book: 101 An Overview (11of27) Generic Drugs Forum 2018 – YouTube, accessed April 10, 2025, https://www.youtube.com/watch?v=Ru1xAPs8iFs
- Generic Drugs: Stakeholder Views on Improving FDA’s Information on Patents | U.S. GAO, accessed April 10, 2025, https://www.gao.gov/products/gao-23-105477
- An Overview of FDA’s Orange Book – YouTube, accessed April 10, 2025, https://www.youtube.com/watch?v=DYYWZxfWB9o
- www.fda.gov, accessed April 10, 2025, https://www.fda.gov/media/94801/download#:~:text=Who%20Utilizes%20the%20Orange%20Book%3F&text=Generic%20drugs%20now%20represent%2088,dispensed%20in%20the%20United%20States.&text=The%20Orange%20Book%20is%20particularly,for%20the%20brand%20name%20product.
- Orange Book: What it is and how it Works – Investopedia, accessed April 10, 2025, https://www.investopedia.com/terms/o/orange-book.asp
- 4 Interesting Facts About the Orange Book – Pharmacy Times, accessed April 10, 2025, https://www.pharmacytimes.com/view/4-interesting-facts-about-the-orange-book
- Orange Book Questions and Answers – FDA, accessed April 10, 2025, https://www.fda.gov/media/160167/download
- Everything You Wanted to Know About the Orange Book But Were Too Afraid To Ask, accessed April 10, 2025, https://www.thefdalawblog.com/2022/07/everything-you-wanted-to-know-about-the-orange-book-but-were-too-afraid-to-ask/
- FDA Approval and Regulation of Pharmaceuticals, 1983-2018 – PubMed, accessed April 10, 2025, https://pubmed.ncbi.nlm.nih.gov/31935033/
- Where We Stand with Generic Drug Approvals and Authorized Generics | Avalere, accessed April 10, 2025, https://avalere.com/insights/where-we-stand-with-generic-drug-approvals-and-authorized-generics-in-2019
- Prioritizing Public Health: The FDA’s Role in the Generic Drug Marketplace – 09/26/2016, accessed April 10, 2025, https://www.fda.gov/news-events/congressional-testimony/prioritizing-public-health-fdas-role-generic-drug-marketplace-09262016
- What’s Trending: Generic Drugs by the Numbers & Key Market Developments, accessed April 10, 2025, https://www.dcatvci.org/features/whats-trending-generic-drugs-by-the-numbers-key-market-developments/
- The 180-Day Rule Supports Generic Competition. Here’s How., accessed April 10, 2025, https://accessiblemeds.org/resources/blog/180-day-rule-supports-generic-competition-heres-how/
- Generic and Biosimilar Drugs Generate A Record $373 Billion For America’s Patients and Healthcare System in 2021 | Association for Accessible Medicines, accessed April 10, 2025, https://accessiblemeds.org/resources/press-releases/generic-and-biosimilar-drugs-generate-record-373-billion-americas-patients/
- Office of Generic Drugs 2022 Annual Report – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/generic-drugs/office-generic-drugs-2022-annual-report
- Generic Drugs – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/buying-using-medicine-safely/generic-drugs
- Report: 2022 U.S. Generic and Biosimilar Medicines Savings Report, accessed April 10, 2025, https://accessiblemeds.org/resources/reports/2022-savings-report/
- Ensuring Access To Generic Medications In The US | Health Affairs Forefront, accessed April 10, 2025, https://www.healthaffairs.org/content/forefront/ensuring-access-generic-medications-us
- U.S. Consumers Overpay for Generic Drugs – May 31, 2022 – USC Schaeffer, accessed April 10, 2025, https://schaeffer.usc.edu/research/u-s-consumers-overpay-for-generic-drugs/
- Prescription Drug Prices in the U.S. Are 2.78 Times Those in Other Countries – RAND, accessed April 10, 2025, https://www.rand.org/news/press/2024/02/01.html
- Variations in Patients’ Perceptions and Use of Generic Drugs: Results of a National Survey, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4870419/
- Generic Drug Utilization and Spending Among Medicare Part D Enrollees in 2022 – ASPE, accessed April 10, 2025, https://aspe.hhs.gov/sites/default/files/documents/920ec8349c53a362b27e3b10669dafd4/generic-drug-landscape-ib.pdf
- GAO-12-371R, Drug Pricing: Research on Savings from Generic Drug Use, accessed April 10, 2025, https://www.gao.gov/assets/gao-12-371r.pdf
- Generic and Biosimilar Drugs Generate $408 Billion in Savings For America’s Patients and Health-Care System in 2022, accessed April 10, 2025, https://accessiblemeds.org/resources/press-releases/generic-biosimilar-drugs-generate-408-billion-savings-2022/
- atch center – Information Technology and Innovation Foundation, accessed April 10, 2025, https://www2.itif.org/2025-hatch-waxman-act-volume.pdf
- Hatch-Waxman Amendments Turn 40 – PharmTech, accessed April 10, 2025, https://www.pharmtech.com/view/hatch-waxman-amendments-turn-40
- Generic Pharmaceutical Manufacturing in the US – Market Research Report (2015-2030), accessed April 10, 2025, https://www.ibisworld.com/united-states/industry/generic-pharmaceutical-manufacturing/488/
- The U.S. Generic & Biosimilar Medicines Savings Report, accessed April 10, 2025, https://accessiblemeds.org/wp-content/uploads/2025/01/AAM-2024-Generic-Biosimilar-Medicines-Savings-Report.pdf
- U.S. Generic Drugs Market Size to Surpass USD 188.44 Bn by 2032 – BioSpace, accessed April 10, 2025, https://www.biospace.com/u-s-generic-drugs-market-size-to-surpass-usd-188-44-bn-by-2032
- The Evolution of Supply and Demand in Markets for Generic Drugs – PMC, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8452364/
- Generic Competition and Drug Prices | FDA, accessed April 10, 2025, https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/generic-competition-and-drug-prices
- Global Generic Drug Markets: Opportunities and Challenges – WPRX, accessed April 10, 2025, https://www.wprx.com/news/global-generic-drug-markets-opportunities-and-challenges
- Drug Competition Series – Analysis of New Generic Markets Effect of Market Entry on Generic Drug Prices – ASPE, accessed April 10, 2025, https://aspe.hhs.gov/sites/default/files/documents/510e964dc7b7f00763a7f8a1dbc5ae7b/aspe-ib-generic-drugs-competition.pdf
- International Prescription Drug Price Comparisons: Estimates Using 2022 Data – PMC, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11147645/
- Analyzing U.S. Pharmaceutical Statistics – Kutest Kids, accessed April 10, 2025, https://www.kutestkids.com/blog/u-s-pharmaceutical-statistics
- U.S. Pharmaceutical Statistics – Mastermind Behavior Services, accessed April 10, 2025, https://www.mastermindbehavior.com/post/u-s-pharmaceutical-statistics-f78c9
- Generic Drugs Market Size & Share Report, 2033, accessed April 10, 2025, https://www.marketdataforecast.com/market-reports/global-generic-drugs-market
- us generics market- evolution of indian players – iqvia, accessed April 10, 2025, https://www.iqvia.com/-/media/iqvia/pdfs/india/us-generics-market-evolution-of-indian-players.pdf
- Recent trends in brand-name and generic drug competition – Duke University, accessed April 10, 2025, https://fds.duke.edu/db/attachment/2575
- FastStats – Therapeutic Drug Use – CDC, accessed April 10, 2025, https://www.cdc.gov/nchs/fastats/drug-use-therapeutic.htm
- The Economic Impact of Generic Drugs on the Healthcare System – East Street Pharmacy, accessed April 10, 2025, https://eaststreetpharmacy.com/the-economic-impact-of-generic-drugs-on-the-healthcare-system.html
- The Impact of Health Economics on Generic Drug Development – DrugPatentWatch, accessed April 10, 2025, https://www.drugpatentwatch.com/blog/the-impact-of-health-economics-on-generic-drug-development/
- 40 Years of Hatch-Waxman – Trillions in Savings for Patients, accessed April 10, 2025, https://accessiblemeds.org/resources/press-releases/40-years-hatch-waxman-trillions-savings-patients/
- $734 Billion in Health Care Savings – SEFAP, accessed April 10, 2025, http://www.sefap.it/economiasanitaria_news_200905/734_Billion_in_Generic_Savings_GPhA.pdf
- Potential Clinical and Economic Impact of Switching Branded Medications to Generics, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5417581/
- 2020 Generic Drug & Biosimilars Access and Savings in the U.S. Report, accessed April 10, 2025, https://accessiblemeds.org/resources/reports/2020-generic-drug-biosimilars-access-and-savings-us-report/
- 40 Years of Hatch-Waxman: How Can We Secure its Legacy? | PhRMA, accessed April 10, 2025, https://phrma.org/blog/40-years-of-hatch-waxman-how-can-we-secure-its-legacy
- Abuse of the Hatch-Waxman Act: Mylan’s Ability to Monopolize Reflects Weaknesses – BrooklynWorks, accessed April 10, 2025, https://brooklynworks.brooklaw.edu/cgi/viewcontent.cgi?article=1241&context=bjcfcl
- Decreasing Drug Costs Through Generics and Biosimilars – National Conference of State Legislatures, accessed April 10, 2025, https://www.ncsl.org/health/decreasing-drug-costs-through-generics-and-biosimilars
- AAM Report: Generics and Biosimilars Savings Reach $445 Billion in 2023, Part 1, accessed April 10, 2025, https://www.centerforbiosimilars.com/view/aam-report-generics-and-biosimilars-savings-reach-445-billion-in-2023-part-1
- Report: 2023 U.S. Generic and Biosimilar Medicines Savings Report, accessed April 10, 2025, https://accessiblemeds.org/resources/reports/2023-savings-report-2/
- Why Are Biosimilars Not Living up to Their Promise in the US? – AMA Journal of Ethics, accessed April 10, 2025, https://journalofethics.ama-assn.org/article/why-are-biosimilars-not-living-their-promise-us/2019-08
- Complete Guide to NDA vs. ANDA: Differences, Processes, and Requirements, accessed April 10, 2025, https://synergbiopharma.com/nda-vs-anda/
- Competition in Generic Drug Markets | NBER, accessed April 10, 2025, https://www.nber.org/digest/nov17/competition-generic-drug-markets
- An Empirical Review of Major Legislation Affecting Drug Development: Past Experiences, Effects, and Unintended Consequences – PubMed Central, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3214718/
- The Myth of Generic Pharmaceutical Competition Under the Hatch-Waxman Act – FLASH: The Fordham Law Archive of Scholarship and History, accessed April 10, 2025, https://ir.lawnet.fordham.edu/cgi/viewcontent.cgi?article=1507&context=iplj
- Reformation of the Hatch-Waxman Act, an Unnecessary Resolution – NSUWorks, accessed April 10, 2025, https://nsuworks.nova.edu/cgi/viewcontent.cgi?article=1305&context=nlr
- Strategies that delay or prevent the timely availability of affordable generic drugs in the United States, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4915805/
- Ensuring the Safety of FDA-Approved Generic Drugs, accessed April 10, 2025, https://www.fda.gov/drugs/cder-conversations/ensuring-safety-fda-approved-generic-drugs
- The Generic Drug Approval Process – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/cder-conversations/generic-drug-approval-process
- Generic Drugs – FDA – Regulations.gov, accessed April 10, 2025, https://downloads.regulations.gov/EPA-HQ-OAR-2024-0196-0003/attachment_87.pdf
- What Is the Approval Process for Generic Drugs? – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/generic-drugs/what-approval-process-generic-drugs
- The Regulatory Pathway for Generic Drugs Explained – DrugPatentWatch, accessed April 10, 2025, https://www.drugpatentwatch.com/blog/the-regulatory-pathway-for-generic-drugs-explained/
- Development & Approval Process | Drugs – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/development-approval-process-drugs
- How the FDA Ensures High-Quality Generic Drugs – AAFP, accessed April 10, 2025, https://www.aafp.org/pubs/afp/issues/2018/0601/p696.html
- A Review of First-Time Generic Drug Approvals – U.S. Pharmacist, accessed April 10, 2025, https://www.uspharmacist.com/article/a-review-of-firsttime-generic-drug-approvals
- Generic Drug Development | FDA, accessed April 10, 2025, https://www.fda.gov/drugs/abbreviated-new-drug-application-anda/generic-drug-development
- Hatch-Waxman Amendments Anniversary – BioPharm International, accessed April 10, 2025, https://www.biopharminternational.com/view/hatch-waxman-amendments-anniversary
- Top 10 Challenges in Generic Drug Development – DrugPatentWatch, accessed April 10, 2025, https://www.drugpatentwatch.com/blog/top-10-challenges-in-generic-drug-development/
- US Generic Drugs Market Size To Hit USD 189.77 Bn By 2033 – Precedence Research, accessed April 10, 2025, https://www.precedenceresearch.com/us-generic-drug-market
- FDA Drug Competition Action Plan, accessed April 10, 2025, https://www.fda.gov/drugs/guidance-compliance-regulatory-information/fda-drug-competition-action-plan
- The ANDA Process: A Guide to FDA Submission & Approval – Excedr, accessed April 10, 2025, https://www.excedr.com/blog/what-is-abbreviated-new-drug-application
- Essential ANDA Checklist: Key Steps to Streamline Your Filing Process, accessed April 10, 2025, https://vicihealthsciences.com/anda-checklist-for-filing-process/
- Abbreviated New Drug Application (ANDA) Approval Process – FDA, accessed April 10, 2025, https://www.fda.gov/media/166141/download
- Abbreviated New Drug Application (ANDA) – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/types-applications/abbreviated-new-drug-application-anda
- Abbreviated New Drug Application (ANDA) Forms and Submission Requirements – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/abbreviated-new-drug-application-anda/abbreviated-new-drug-application-anda-forms-and-submission-requirements
- Abbreviated New Drug Applications (ANDA) Explained: A Quick-Guide – The FDA Group, accessed April 10, 2025, https://www.thefdagroup.com/blog/abbreviated-new-drug-applications-anda
- Drug Application Process for Nonprescription Drugs – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/types-applications/drug-application-process-nonprescription-drugs
- Requirements and Resources for Approved ANDAs – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/abbreviated-new-drug-application-anda/requirements-and-resources-approved-andas
- ANDA Submissions—Amendments and Requests for Final Approval to Tentatively Approved ANDAs – FDA, accessed April 10, 2025, https://www.fda.gov/media/119718/download
- The Generic Drug User Fee Amendments (GDUFA): Background and Reauthorization, accessed April 10, 2025, https://www.congress.gov/crs-product/R46778
- The Generic Drug User Fee Amendments (GDUFA): Background and Reauthorization – CRS Reports, accessed April 10, 2025, https://crsreports.congress.gov/product/pdf/R/R46778/3
- Impact of Tariffs on the Generic Drug Market – Pharmaceutical Commerce, accessed April 10, 2025, https://www.pharmaceuticalcommerce.com/view/impact-of-tariffs-on-the-generic-drug-market
- Will pharmaceutical tariffs achieve their goals? – Brookings Institution, accessed April 10, 2025, https://www.brookings.edu/articles/pharmaceutical-tariffs-how-they-play-out/
- What Other Countries Could Teach the U.S. About Bringing Down Drug Prices, accessed April 10, 2025, https://www.gsb.stanford.edu/insights/what-other-countries-could-teach-us-about-bringing-down-drug-prices
- U.S. Patients Rely On Generic Medicines But Increases In Drug Shortages Reflect Challenges To Their Long-Term Sustainability, accessed April 10, 2025, https://accessiblemeds.org/resources/blog/generic-medicines-drug-shortages-challenges-sustainability/
- Industrial Policy To Reduce Prescription Generic Drug Shortages, accessed April 10, 2025, https://www.americanprogress.org/article/industrial-policy-to-reduce-prescription-generic-drug-shortages/
- Patent Certifications and Suitability Petitions – FDA, accessed April 10, 2025, https://www.fda.gov/drugs/abbreviated-new-drug-application-anda/patent-certifications-and-suitability-petitions
- www.congress.gov, accessed April 10, 2025, https://www.congress.gov/bill/102nd-congress/house-bill/2454#:~:text=Generic%20Drug%20Enforcement%20Act%20of%201992%20%2D%20Amends%20the%20Federal%20Food,for%20development%20or%20approval%2C%20of
- H.R.2454 – Generic Drug Enforcement Act of 1992 – Congress.gov, accessed April 10, 2025, https://www.congress.gov/bill/102nd-congress/house-bill/2454
- FDA “failures allowing criminals into drug approval process” – PharmaTimes, accessed April 10, 2025, https://pharmatimes.com/news/fda_failures_allowing_criminals_into_drug_approval_process_987679/
- Generic Drug Enforcement Act of 1992 : – Berkeley Law, accessed April 10, 2025, https://lawcat.berkeley.edu/record/370912
- Generic Drug Enforcement Act imposed debarment and other penalties for illegal acts involving abbreviated drug applications – LifeScienceHistory.com, accessed April 10, 2025, https://www.lifesciencehistory.com/generic-drug-enforcement-act-imposed-debarment-and-other-penalties-for-illegal-acts-involving-abbreviated-drug-applications/
- 11/08/1994 – FDA, accessed April 10, 2025, https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/fda-debarment-list-drug-product-applications/11081994
- 21 U.S. Code § 335a – Debarment, temporary denial of approval, and suspension, accessed April 10, 2025, https://www.law.cornell.edu/uscode/text/21/335a
- STAT. 149 Public Law 102-282 102d Congress An Act, accessed April 10, 2025, https://www.congress.gov/102/statute/STATUTE-106/STATUTE-106-Pg149.pdf
- The Food and Drug Administration (FDA) is issuing an was convicted of a felony under Federal law for conduct relating has failed, accessed April 10, 2025, https://downloads.regulations.gov/FDA-1992-N-0399-0002/attachment_1.pdf
- Submitting Debarment Certification Statements October 1998 – FDA, accessed April 10, 2025, https://www.fda.gov/regulatory-information/search-fda-guidance-documents/submitting-debarment-certification-statements
- Generic Drug Enforcement Act of 1992 | TOPN: Table of Popular Names | US Law, accessed April 10, 2025, https://www.law.cornell.edu/topn/generic_drug_enforcement_act_of_1992
- A prescription for change: How the Medicare Act revises Hatch-Waxman to speed market entry of generic drugs – eScholarship@BC, accessed April 10, 2025, https://boots.bc.edu/islandora/object/bc-ir:100267/datastream/PDF/download/citation.pdf
- Continuing Abuse of the Hatch-Waxman Act by Pharmaceutical Patent Holders and the Failure of the 2003 Amendments – UC Law SF Scholarship Repository, accessed April 10, 2025, https://repository.uclawsf.edu/cgi/viewcontent.cgi?article=3715&context=hastings_law_journal
- Changes to Hatch-Waxman.indd – Alston & Bird, accessed April 10, 2025, https://www.alston.com/-/media/files/insights/publications/2004/03/ilife-sciences-advisoryi-changes-to-hatchwaxman-un/files/changes-to-hatchwaxman/fileattachment/changes-to-hatchwaxman.pdf
- Medicare’s New Price-Setting Powers Are Historic – Penn LDI – Leonard Davis Institute, accessed April 10, 2025, https://ldi.upenn.edu/our-work/research-updates/medicares-new-price-setting-powers-are-historic-but-could-harm-innovation-an-ldi-fellow-warns/
- The balance between innovation and competition: the Hatch-Waxman Act, the 2003 Amendments, and beyond – PubMed, accessed April 10, 2025, https://pubmed.ncbi.nlm.nih.gov/24505856/
- The Medicare Prescription Drug, Improvement, & Modernization Act of 2003: Are We Playing the Lottery With Healthcare Reform? – Duke Law Scholarship Repository, accessed April 10, 2025, https://scholarship.law.duke.edu/cgi/viewcontent.cgi?article=1115&context=dltr
- FDA Rule Changes: The Impact on Hatch-Waxman Litigation, accessed April 10, 2025, https://www.finnegan.com/en/insights/events/webinar-fda-rule-changes-the-impact-on-hatch-waxman-litigation.html
- Medicare Modernization Act (MMA) – Federal Trade Commission, accessed April 10, 2025, https://www.ftc.gov/terms/medicare-modernization-act-mma
- Generic Drug User Fee Amendments – FDA, accessed April 10, 2025, https://www.fda.gov/industry/fda-user-fee-programs/generic-drug-user-fee-amendments
- GAO-17-452, GENERIC DRUG USER FEES: Application Review Times Declined, but FDA Should Develop a Plan for Administering Its Unobl, accessed April 10, 2025, https://www.gao.gov/assets/gao-17-452.pdf
- The generic drug user fee amendments: an economic perspective – Oxford Academic, accessed April 10, 2025, https://academic.oup.com/jlb/article/5/1/103/4968039
- Economic Impacts of the Generic Drug User Fee Act Fee Structure – PubMed, accessed April 10, 2025, https://pubmed.ncbi.nlm.nih.gov/28577697/
- GDUFA III Reauthorization – FDA, accessed April 10, 2025, https://www.fda.gov/industry/generic-drug-user-fee-amendments/gdufa-iii-reauthorization
- The Generic Drug User Fee Amendments: An Economic Perspective | NBER, accessed April 10, 2025, https://www.nber.org/papers/w23642
- The generic drug user fee amendments: an economic perspective – DSpace@MIT, accessed April 10, 2025, https://dspace.mit.edu/handle/1721.1/120507
- Generic drug user fees come into effect, accessed April 10, 2025, https://gabionline.net/policies-legislation/Generic-drug-user-fees-come-into-effect
- The Generic Industry Faces External Challenges – Lachman Consultants, accessed April 10, 2025, https://www.lachmanconsultants.com/2024/02/the-generic-industry-faces-external-challenges/
- Generic Drugs Market 2024-2035: Trends, Innovations, and Future Growth, accessed April 10, 2025, https://www.pharmiweb.com/press-release/2025-02-12/generic-drugs-market-2024-2035-trends-innovations-and-future-growth
- Generic Pharmaceuticals Contract Manufacturing Market to Surpass Valuation of US$ 135.43 Billion By 2033 | Astute Analytica – GlobeNewswire, accessed April 10, 2025, https://www.globenewswire.com/news-release/2025/02/21/3030487/0/en/Generic-Pharmaceuticals-Contract-Manufacturing-Market-to-Surpass-Valuation-of-US-135-43-Billion-By-2033-Astute-Analytica.html
- The Future of Generic Drug Development in Emerging Markets – DrugPatentWatch, accessed April 10, 2025, https://www.drugpatentwatch.com/blog/the-future-of-generic-drug-development-in-emerging-markets/
- Biosimilar Disruption: Taking the Temperature of Drugmakers | American Century, accessed April 10, 2025, https://www.americancentury.com/insights/biosimilar-disruption-taking-the-temperature-of-drugmakers/
- Expected Impact of Biosimilars on the Pharmaceutical Companies – PMC, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8438344/
- The Economics of Biosimilars – PMC, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4031732/
- Biosimilars in the United States 2023-2027 – IQVIA, accessed April 10, 2025, https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/biosimilars-in-the-united-states-2023-2027
- US Election: Impacts on Biosimilars and Generics : Parsity Group LTD, accessed April 10, 2025, https://www.parsitygroup.com/blog/us-election-impacts-on-biosimilars-and-generics
- Strategies for Overcoming Barriers to Adopting Biosimilars and Achieving Goals of the Biologics Price Competition and Innovation Act: A Survey of Managed Care and Specialty Pharmacy Professionals – PMC, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10397695/
- Biosimilar Uptake Lags in US Despite Potential Cost Savings, accessed April 10, 2025, https://www.ajmc.com/view/biosimilar-uptake-lags-in-us-despite-potential-cost-savings
- Overcoming Barriers to Biosimilar Adoption – American Journal of Managed Care, accessed April 10, 2025, https://www.ajmc.com/view/overcoming-barriers-to-biosimilar-adoption
- Breaking Down Barriers: Why Biosimilars Face Resistance in the US Market – HCPLive, accessed April 10, 2025, https://www.hcplive.com/view/breaking-down-barriers-why-biosimilars-face-resistance-us-market
- Overcoming Economic, Noneconomic Barriers to Biosimilar Adoption in Oncology, accessed April 10, 2025, https://www.centerforbiosimilars.com/view/overcoming-economic-noneconomic-barriers-to-biosimilar-adoption-in-oncology
- US Biosimilar Uptake Challenges and the Quest for Cost-Savings – RxC International, accessed April 10, 2025, https://www.rxcinternational.com/white-papers-and-articles/us-biosimilar-uptake-challenges
- Understanding the Barriers to US Biosimilars: Navigating Challenges for Market Success, accessed April 10, 2025, https://www.drugpatentwatch.com/blog/understanding-barriers-us-biosimilars/
- A Multistakeholder Consensus on Challenges and Solutions to the Adoption of Biosimilars, accessed April 10, 2025, https://ahdbonline.com/supplements/a-multistakeholder-consensus-on-challenges-and-solutions-to-the-adoption-of-biosimilars
- Biosimilar Adoption & Barriers to Success: Current and Future Considerations – FDA, accessed April 10, 2025, https://www.fda.gov/media/143990/download
- Generics 2030 – KPMG International, accessed April 10, 2025, https://kpmg.com/kpmg-us/content/dam/kpmg/pdf/2023/generics-2030.pdf
- US Generic Pharmaceutical Industry Economic Instability – API Innovation Center, accessed April 10, 2025, https://apicenter.org/wp-content/uploads/2023/07/US-Generic-Pharmaceutical-Industry-Economic-Instability.pdf
- Competition in International Generic Drug Markets – PMC, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11470386/
- Competition in International Generic Drug Markets – PubMed, accessed April 10, 2025, https://pubmed.ncbi.nlm.nih.gov/39392640/
- Competition in International Generic Drug Markets – ODPRN, accessed April 10, 2025, https://odprn.ca/research/publications/competition-in-international-generic-drug-markets/
- Competition in generic drug markets: international progress and room for improvement, 2010-2021 – Canada.ca, accessed April 10, 2025, https://www.canada.ca/en/patented-medicine-prices-review/services/npduis/analytical-studies/posters/competition-generic-international.html
- Competition And Vulnerabilities In The Global Supply Chain For US Generic Active Pharmaceutical Ingredients | Health Affairs, accessed April 10, 2025, https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2022.01120?journalCode=hlthaff
- How Tariffs Could Affect Generic Drug Prices and the Global Pharmaceutical Market, accessed April 10, 2025, https://www.pharmaceuticalcommerce.com/view/tariffs-generic-drug-prices-global-pharmaceutical-market
- Comparing Prescription Drugs in the U.S. and Other Countries: Prices and Availability, accessed April 10, 2025, https://aspe.hhs.gov/reports/comparing-prescription-drugs
- What Should US Policymakers Learn From International Drug Pricing Transparency Strategies? – AMA Journal of Ethics, accessed April 10, 2025, https://journalofethics.ama-assn.org/article/what-should-us-policymakers-learn-international-drug-pricing-transparency-strategies/2022-11
- Schaeffer White Paper Highlights Failures in Generic Drug Market That Cost Patients, accessed April 10, 2025, https://schaeffer.usc.edu/research/paper-highlights-failures-in-the-generic-drug-market-that-are-costing-patients/
- The Impact of Pharmaceutical Wholesalers on U.S. Drug Spending | Commonwealth Fund, accessed April 10, 2025, https://www.commonwealthfund.org/publications/issue-briefs/2022/jul/impact-pharmaceutical-wholesalers-drug-spending
- Generics 2030: Three strategies to curb the downward spiral – KPMG International, accessed April 10, 2025, https://kpmg.com/us/en/articles/2023/generics-2030-curb-downward-spiral.html
- Regulatory Affairs: The Generic Industry Faces External Challenges – Contract Pharma, accessed April 10, 2025, https://www.contractpharma.com/exclusives/regulatory-affairs-the-generic-industry-faces-external-challenges/
- Generic Drugs Market Size to Hit USD 775.61 Billion by 2033 – BioSpace, accessed April 10, 2025, https://www.biospace.com/press-releases/generic-drugs-market-size-to-hit-usd-775-61-billion-by-2033
- International reference pricing of pharmaceuticals in the United States: Implications for potentially curative treatments – PMC, accessed April 10, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10373031/