Drug Repositioning in Rare/Orphan and Neglected Diseases: A Beacon of Hope for Underserved Patients
In the vast landscape of medical research and drug development, certain diseases often fall through the cracks. Rare or orphan diseases, which affect a small percentage of the population, and neglected diseases, which primarily impact developing countries, have long been overlooked by traditional pharmaceutical research. However, a promising approach called drug repositioning is emerging as a beacon of hope for patients suffering from these conditions.
Understanding Drug Repositioning
Drug repositioning, also known as drug repurposing, is the process of identifying new therapeutic uses for existing drugs. This innovative approach has gained significant traction in recent years, particularly in the realm of rare/orphan and neglected diseases.
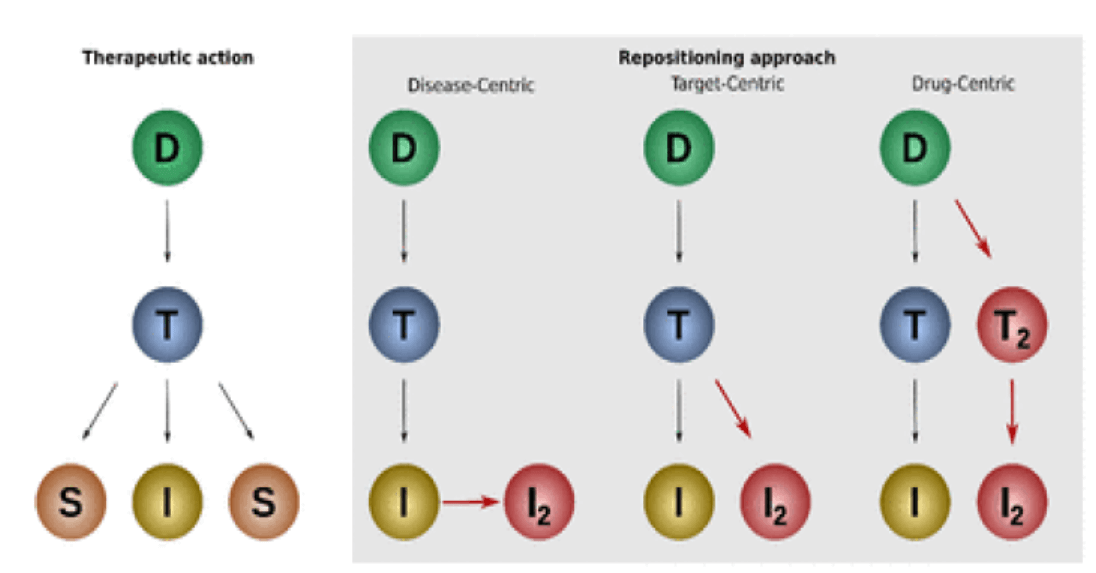
The Concept of Drug Repositioning
At its core, drug repositioning is about finding new applications for drugs that have already been approved for other conditions. This strategy leverages the wealth of knowledge and data accumulated during the original drug development process, including safety profiles and pharmacokinetic properties.
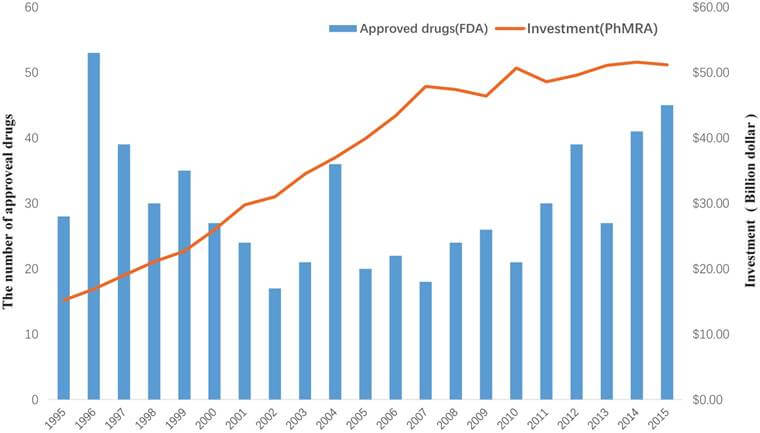
Why Drug Repositioning Matters
Drug repositioning offers several advantages over traditional drug discovery methods:
- Reduced time to market
- Lower development costs
- Improved safety profiles
- Increased success rates
These benefits are particularly crucial when addressing rare/orphan and neglected diseases, where traditional drug development often falls short due to limited financial incentives and market size.
The Landscape of Rare/Orphan Diseases
Rare or orphan diseases present unique challenges in the world of medical research and drug development.
Defining Rare/Orphan Diseases
A rare disease, also known as an orphan disease, is typically defined as a condition that affects fewer than 200,000 people in the United States or less than 1 in 2,000 people in Europe. Despite their individual rarity, collectively, these diseases impact millions of people worldwide.
Challenges in Rare Disease Drug Development
Developing treatments for rare diseases faces several obstacles:
- Limited patient populations for clinical trials
- High costs relative to potential market size
- Lack of understanding of disease mechanisms
- Regulatory hurdles
These challenges often result in a lack of approved treatments for many rare diseases, leaving patients with few options.
The Burden of Neglected Diseases
Neglected diseases, primarily affecting developing countries, pose a significant global health challenge.
Understanding Neglected Diseases
Neglected diseases are a group of tropical infections that are especially endemic in low-income populations in developing regions of Africa, Asia, and the Americas. These diseases often receive little attention from the pharmaceutical industry due to limited profit potential.
The Global Impact of Neglected Diseases
Neglected diseases affect over a billion people worldwide and contribute to a cycle of poverty in many developing countries. Despite their widespread impact, research and development for these diseases remain underfunded.
Drug Repositioning: A Game-Changer for Rare and Neglected Diseases
Drug repositioning offers a promising solution to the challenges faced in developing treatments for rare/orphan and neglected diseases.
Advantages of Drug Repositioning in Rare Diseases
For rare diseases, drug repositioning provides several benefits:
- Faster development timelines
- Reduced costs
- Improved understanding of disease mechanisms
- Potential for multiple treatment options
These advantages make drug repositioning an attractive option for addressing the unmet needs of rare disease patients.
The Promise of Drug Repositioning in Neglected Diseases
In the context of neglected diseases, drug repositioning offers:
- Cost-effective treatment options
- Rapid deployment of therapies
- Improved access to medications in resource-limited settings
- Potential for combination therapies
By leveraging existing drugs, researchers can quickly identify potential treatments for neglected diseases, potentially saving millions of lives.
Success Stories in Drug Repositioning
Several notable success stories highlight the potential of drug repositioning in rare/orphan and neglected diseases.
Thalidomide: From Tragedy to Treatment
Thalidomide, originally developed as a sedative, gained notoriety in the 1960s due to its severe side effects on fetal development. However, it has since been repositioned as a treatment for multiple myeloma and leprosy, demonstrating the potential for drugs to find new life in unexpected areas.
Sildenafil: Beyond Erectile Dysfunction
Sildenafil, better known by its brand name Viagra, was initially developed to treat angina. While it proved ineffective for its original purpose, it became a blockbuster drug for erectile dysfunction. More recently, it has been repositioned to treat pulmonary arterial hypertension, a rare disease.
Ivermectin: A Neglected Disease Success Story
Ivermectin, originally developed as an antiparasitic for livestock, has been repositioned to treat various neglected tropical diseases, including river blindness and lymphatic filariasis. This repositioning has had a significant impact on global health, particularly in developing countries.
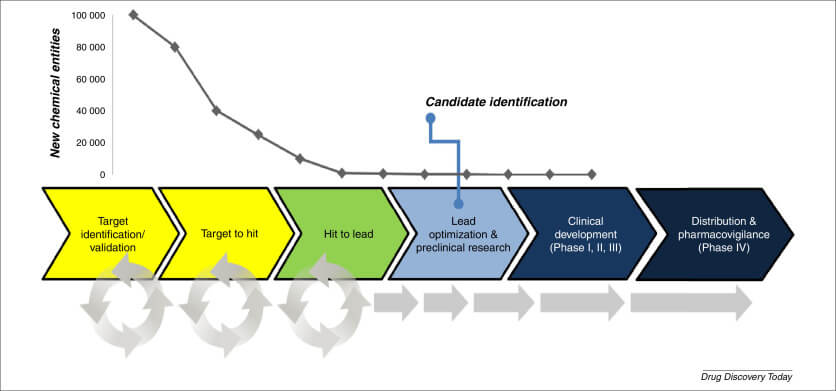
The Drug Repositioning Process
Drug repositioning involves a systematic approach to identifying potential new uses for existing drugs.
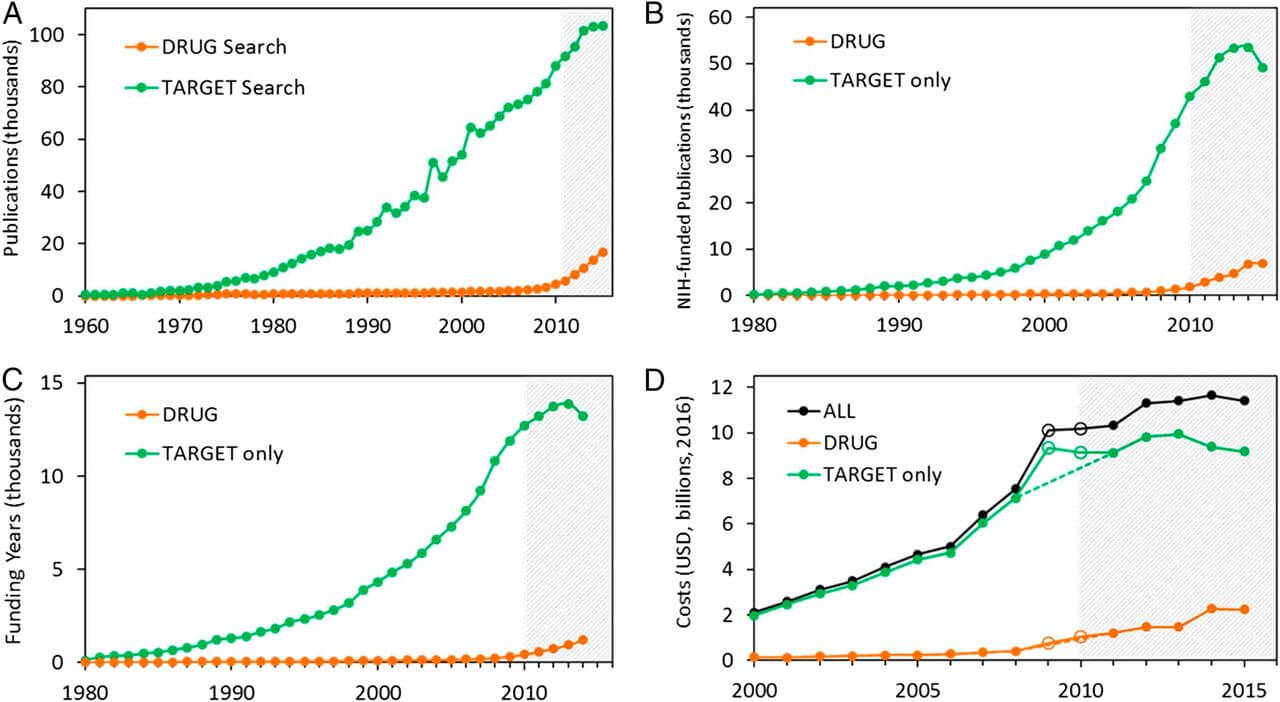
Computational Methods in Drug Repositioning
Advances in computational biology and artificial intelligence have revolutionized the drug repositioning process. These methods include:
- Network-based approaches
- Machine learning algorithms
- Text mining of scientific literature
- Molecular docking simulations
These computational tools allow researchers to rapidly screen thousands of compounds against potential disease targets, significantly accelerating the drug discovery process.
Experimental Validation
While computational methods provide valuable leads, experimental validation remains crucial. This typically involves:
- In vitro studies to confirm drug-target interactions
- Animal models to assess efficacy and safety
- Clinical trials to evaluate the drug in human patients
This multi-step process ensures that repositioned drugs meet the same rigorous standards as newly developed compounds.
Challenges in Drug Repositioning
Despite its promise, drug repositioning faces several challenges that must be addressed.
Intellectual Property Considerations
One of the main hurdles in drug repositioning is navigating the complex landscape of intellectual property rights. Existing patents may limit the commercial viability of repositioned drugs, requiring creative legal solutions.
Regulatory Hurdles
While repositioned drugs may have established safety profiles, they still need to undergo regulatory approval for new indications. This process can be time-consuming and costly, potentially offsetting some of the advantages of repositioning.
Scientific Challenges
Identifying the molecular mechanisms underlying a drug’s potential new use can be challenging. Additionally, drugs may behave differently in the context of a new disease, requiring careful evaluation of efficacy and safety.
The Role of Collaboration in Drug Repositioning
Successful drug repositioning often requires collaboration between various stakeholders.
Academic-Industry Partnerships
Collaborations between academic researchers and pharmaceutical companies can accelerate the drug repositioning process. These partnerships combine the innovative research of academia with the resources and expertise of industry.
Patient Advocacy Groups
Patient advocacy groups play a crucial role in drug repositioning for rare diseases. These organizations can provide valuable insights into patient needs, help recruit for clinical trials, and advocate for regulatory approval.
International Collaborations
For neglected diseases, international collaborations are essential. Organizations like the Drugs for Neglected Diseases initiative (DNDi) bring together researchers, pharmaceutical companies, and governments to address global health challenges through drug repositioning.
The Future of Drug Repositioning
As technology advances and our understanding of disease mechanisms improves, the future of drug repositioning looks promising.
Emerging Technologies
New technologies are set to revolutionize drug repositioning:
- CRISPR gene editing for target validation
- Organ-on-a-chip models for drug screening
- AI-powered drug discovery platforms
- Big data analytics for patient stratification
These innovations will likely accelerate the identification of new uses for existing drugs.
Personalized Medicine and Drug Repositioning
The growing field of personalized medicine offers exciting opportunities for drug repositioning. By understanding individual genetic profiles, researchers can identify subgroups of patients who may respond to repositioned drugs, even if the broader population does not.
Ethical Considerations in Drug Repositioning
As with any medical research, drug repositioning raises important ethical questions.
Access and Affordability
While drug repositioning can potentially reduce development costs, ensuring that repositioned drugs are accessible and affordable to patients in need remains a challenge. This is particularly crucial for neglected diseases affecting low-income populations.
Off-Label Use and Patient Safety
The off-label use of drugs, often a precursor to formal repositioning, raises concerns about patient safety and informed consent. Balancing the potential benefits of repositioned drugs with the need for rigorous safety evaluation is an ongoing ethical challenge.
Policy Implications for Drug Repositioning
Government policies play a crucial role in incentivizing and regulating drug repositioning efforts.
Orphan Drug Legislation
Many countries have implemented orphan drug legislation to encourage the development of treatments for rare diseases. These policies often include tax incentives, extended market exclusivity, and streamlined regulatory processes.
Neglected Disease Initiatives
International initiatives, such as the WHO’s Neglected Tropical Disease Roadmap, provide frameworks for addressing neglected diseases. These efforts often include support for drug repositioning as a cost-effective strategy.
Case Study: Drug Repositioning in COVID-19
The COVID-19 pandemic has highlighted the potential of drug repositioning in responding to global health crises.
Rapid Response to a Global Threat
During the early stages of the pandemic, researchers quickly turned to drug repositioning as a strategy to identify potential treatments. This approach allowed for the rapid screening of existing drugs that could be repurposed to treat COVID-19.
Successes and Challenges
While some repositioned drugs, such as dexamethasone, have shown promise in treating COVID-19, others have faced setbacks. This experience underscores both the potential and the limitations of drug repositioning in addressing emerging health threats.
Key Takeaways
Drug repositioning offers a promising approach to addressing the unmet medical needs of patients with rare/orphan and neglected diseases. Key points to remember include:
- Drug repositioning can significantly reduce the time and cost of drug development.
- Computational methods and collaborative efforts are driving advances in drug repositioning.
- Challenges remain, including intellectual property issues and regulatory hurdles.
- Ethical considerations and policy support are crucial for the success of drug repositioning efforts.
- The COVID-19 pandemic has demonstrated the potential of drug repositioning in responding to global health crises.
As we move forward, drug repositioning is likely to play an increasingly important role in developing treatments for rare/orphan and neglected diseases, offering hope to millions of patients worldwide.
“Drug repositioning represents a paradigm shift in how we approach drug discovery for rare and neglected diseases. By leveraging existing knowledge and resources, we can accelerate the development of life-saving treatments for patients who have long been overlooked by traditional pharmaceutical research.”
– Dr. Maria Fernandez-Velasco, Lead Researcher at the Spanish National Centre for Cardiovascular Research
FAQs
- What is the main difference between rare diseases and neglected diseases?
Rare diseases are defined by their low prevalence in the general population, typically affecting fewer than 200,000 people in the US. Neglected diseases, on the other hand, may affect large populations but primarily impact low-income countries and receive little attention from pharmaceutical research. - How does drug repositioning differ from traditional drug discovery?
Drug repositioning focuses on finding new uses for existing, approved drugs, while traditional drug discovery involves developing entirely new compounds. Repositioning can be faster and less expensive as it builds on existing safety and pharmacological data. - Can any drug be repositioned for rare or neglected diseases?
While many drugs have potential for repositioning, not all will be suitable. The success of repositioning depends on factors such as the drug’s mechanism of action, safety profile, and how well it matches the target disease’s pathology. - What role does artificial intelligence play in drug repositioning?
AI and machine learning algorithms can rapidly analyze vast amounts of data to identify potential matches between existing drugs and new disease targets. This significantly accelerates the initial screening process in drug repositioning. - How can patients with rare diseases benefit from drug repositioning efforts?
Drug repositioning can lead to faster development of treatments for rare diseases, potentially offering new therapeutic options where none previously existed. It can also result in more affordable treatments due to lower development costs.