In 2021, the United States healthcare system spent a staggering $603 billion on prescription drugs before accounting for rebates, with $421 billion going to retail drugs and $182 billion to non-retail medications1. This enormous expenditure continues to rise, driven primarily by increasing costs per prescription rather than greater usage. The pharmaceutical landscape is becoming increasingly concentrated, with just 2.3% of the population accounting for half of all drug spending by 2018, down from 6.0% in 20015. Specialty drugs now represent approximately 50% of total drug spending despite being used by relatively few patients, while brand-name drugs account for 80% of spending but only 20% of prescriptions filled1. Recent policy interventions, particularly the Inflation Reduction Act, aim to address these issues through Medicare price negotiation and inflation rebates, though their full impact remains to be seen. Understanding where prescription drug dollars actually go is essential for patients, healthcare providers, policymakers, and anyone concerned about the sustainability of the U.S. healthcare system.
The Current Landscape of US Drug Spending
Total Prescription Drug Expenditures: A $600+ Billion Industry
The scale of prescription drug spending in the United States is difficult to comprehend. In 2021, total prescription drug expenditures reached $603 billion, with $421 billion spent on retail drugs and $182 billion on non-retail drugs1. To put this in perspective, this amount exceeds the GDP of many countries and represents a significant portion of all healthcare spending in America.
This massive expenditure isn’t evenly distributed across all medications. In fact, a surprisingly small number of drugs account for a disproportionate share of spending. The top 10% of drugs by price make up fewer than 1% of all prescriptions but account for 15% of retail spending and a staggering 20-25% of non-retail spending1. This concentration reflects the high cost of specialty medications and brand-name drugs that dominate the spending landscape.
The sheer volume of prescription drugs is also noteworthy. In 2021, Americans filled over 8.7 billion prescriptions1, averaging more than 26 prescriptions for every man, woman, and child in the country. This volume, combined with increasing costs per prescription, has driven the steady growth in total expenditures over recent years.
Historical Trends in Pharmaceutical Spending (2010-2025)
The growth in pharmaceutical spending over the past decade tells a compelling story of how drug costs have evolved. Between 2016 and 2021 alone, prescription drug spending increased by 16%, from $520 billion to $603 billion1. This growth wasn’t primarily driven by Americans taking more medications—prescription volume only increased by about 5.7% during this period—but rather by the increasing cost per prescription.
Looking further back, the trend becomes even more dramatic. Data shows that pharmaceutical spending topped $570 billion in 2020, representing a 77% increase from $322 billion in 20104. This growth rate far outpaces inflation and wage growth during the same period, placing an ever-increasing burden on patients, insurers, and government programs.
What’s particularly interesting is that despite the overall increase in spending, out-of-pocket costs for prescription drugs have actually decreased slightly, from $48 billion in 2010 to $47 billion in 20204. This apparent contradiction reflects the complex nature of drug pricing and insurance coverage in the US, where increasing list prices are often offset by rebates and insurance coverage for many patients.
Looking ahead, projections suggest continued growth in pharmaceutical spending. The global prescription drug market is expected to reach a staggering $1.33 trillion by 20292, with the US likely maintaining its position as the largest pharmaceutical market in the world.
Comparing US Drug Spending to Other Countries
One of the most striking aspects of US pharmaceutical spending is how it compares internationally. Americans not only spend more in absolute terms but also on a per-capita basis than citizens of any other developed nation. According to research, prescription drug prices in the US are more than 2.5 times as high as those in other similar high-income nations1.
This disparity exists for several reasons. Unlike many other countries, the US does not have a centralized system for negotiating drug prices. Each insurance company, pharmacy benefit manager, and government program negotiates separately, resulting in fragmented purchasing power. Additionally, other countries often employ reference pricing, therapeutic substitution, and value-based assessment strategies that help control costs.
The impact of this international price disparity is significant. Many Americans struggle to afford their medications, with some resorting to rationing their prescriptions or seeking medications from other countries. Meanwhile, pharmaceutical companies argue that higher US prices subsidize research and development that benefits patients worldwide.
Breaking Down the Cost Components
Retail vs. Non-Retail Drug Expenditures
Understanding where drug spending occurs helps illuminate how these costs flow through the healthcare system. Of the $603 billion spent on prescription drugs in 2021, $421 billion (70%) went to retail drugs—those dispensed at pharmacies—while $182 billion (30%) went to non-retail drugs, which are typically administered in clinical settings like hospitals or doctors’ offices1.
Interestingly, the growth patterns for these two categories differ significantly. Between 2016 and 2021, non-retail drug expenditures grew by 25.1%, substantially outpacing the 12.5% growth in retail expenditures1. This differential growth reflects the increasing use of specialty medications that require professional administration and monitoring.
The settings where Americans receive their medications have also evolved. Between 2016 and 2021, there were significant increases in drugs dispensed through mail-order pharmacies (35% increase), clinics (45% increase), and home health care (95% increase). During this same period, there were decreases in drugs received through independent pharmacies (5% decrease), long-term care facilities (17% decrease), and federal facilities (9% decrease)1. These shifts reflect changing patient preferences, the impact of the COVID-19 pandemic, and evolving healthcare delivery models.
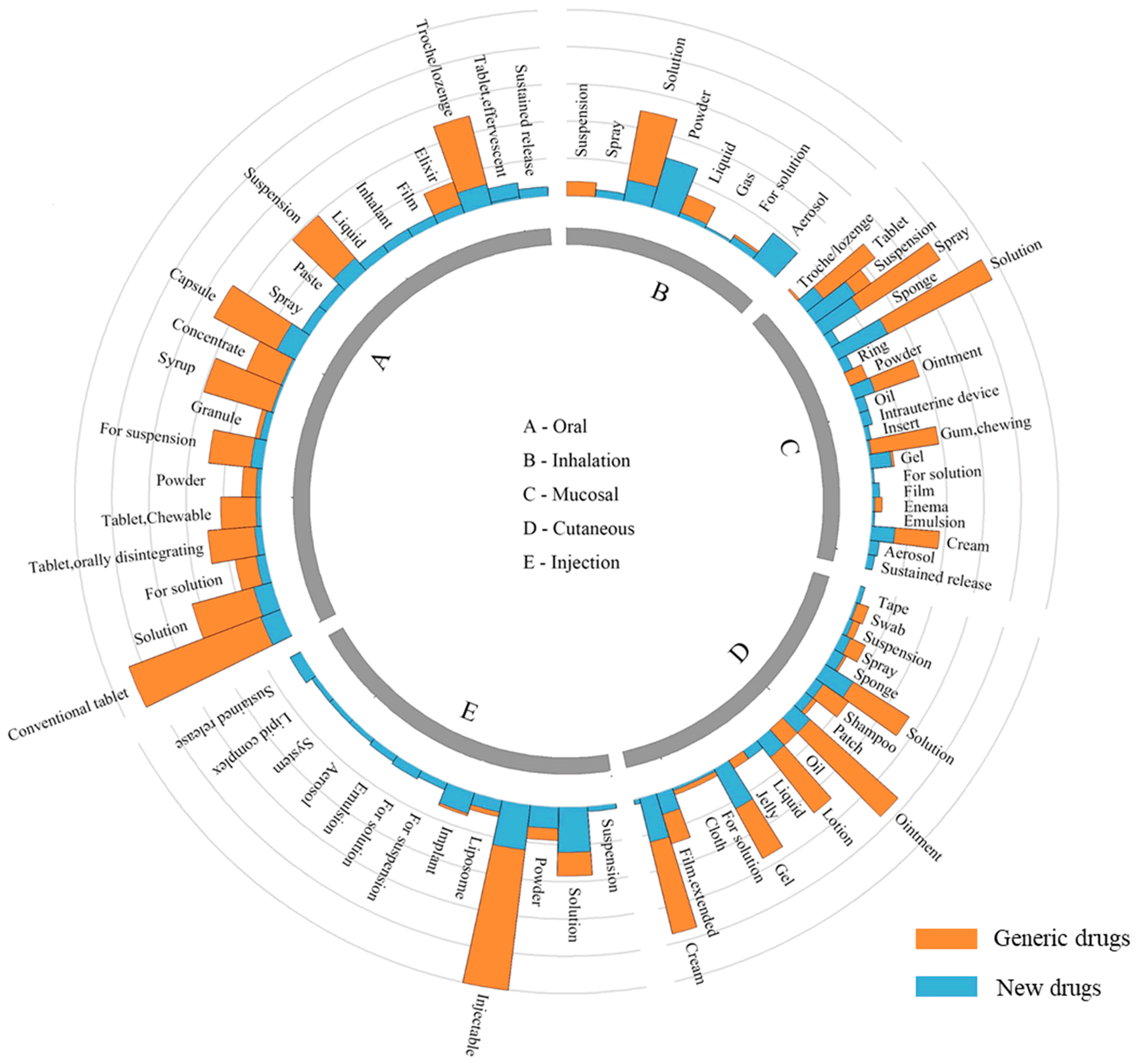
Brand Name vs. Generic Drug Spending
One of the most significant divides in pharmaceutical spending is between brand-name and generic drugs. While generic drugs make up approximately 80% of all prescriptions filled in the United States, they account for only about 20% of prescription drug spending1. Conversely, brand-name drugs represent just 20% of prescriptions but consume 80% of spending in both retail and non-retail settings.
This stark contrast highlights the dramatic price differential between brand-name and generic medications. On average, generic drugs cost 80-85% less than their brand-name counterparts. Yet despite this lower cost, generic medications contain the same active ingredients and must meet the same FDA standards for safety and efficacy.
The transition of a medication from brand-name to generic status typically occurs after the original patent expires, allowing other manufacturers to produce equivalent versions. This patent expiration process, known as the “patent cliff,” can lead to dramatic reductions in the price of widely-used medications. However, pharmaceutical companies have developed various strategies to extend patent protection and delay generic competition, including making minor modifications to existing drugs and filing secondary patents.
The Growing Impact of Specialty Drugs
Specialty Drug Spending Growth
Perhaps no trend has had a greater impact on drug spending in recent years than the rise of specialty pharmaceuticals. These complex medications, often biologics or treatments for rare diseases, come with extraordinarily high price tags—frequently exceeding $10,000 per month or $100,000 per year.
In 2021, specialty drugs totaled $301 billion in spending, representing a remarkable 43% increase since 20161. These medications now account for approximately 50% of total drug spending, despite being used by a relatively small percentage of patients. This percentage has grown substantially over the past decade; specialty drugs represented just 32% of drug spending in 2012 but increased to 51% by 20225.
The growth in specialty drug spending is particularly pronounced in government programs. In Medicare Part D, net spending on specialty drugs increased from $8.7 billion in 2010 to $32.8 billion in 2015, with their share of total net drug spending rising from 13% to 31%5. The Congressional Budget Office anticipates this trend will continue in the coming years.
Categories Driving Specialty Drug Costs
Certain therapeutic categories dominate specialty drug spending. Immunology and oncology products are particularly significant drivers of growth5. Medications for conditions like rheumatoid arthritis, psoriasis, multiple sclerosis, and various cancers often cost tens of thousands of dollars annually per patient.
For example, many newer cancer therapies can cost over $100,000 for a course of treatment. Medications for rare diseases, sometimes called “orphan drugs,” can be even more expensive, with some priced at over $1 million per patient per year. These high-cost treatments, while often life-changing or life-saving for patients, place enormous pressure on the healthcare system and contribute significantly to rising premiums and out-of-pocket costs.
The concentration of spending on these high-cost medications is remarkable. In 2021, the 10 top-selling Medicare Part D drugs accounted for just 0.3% of covered drugs but represented 22% of total gross Part D spending5. This extreme concentration illustrates how a handful of expensive medications can drive overall pharmaceutical spending trends.
Where Your Prescription Money Goes
The Distribution Chain of Drug Spending
When you pay for a prescription medication, your money flows through a complex network of entities, each taking a portion of the total spending. Understanding this distribution chain is essential to comprehending where drug dollars ultimately end up.
The journey of a prescription drug from manufacturer to patient involves multiple intermediaries, each adding costs along the way. The process typically begins with the drug manufacturer, who sells to wholesale distributors. These wholesalers then sell to pharmacies, who ultimately dispense the medication to patients.
At each stage, markups occur. Manufacturers set the initial list price, often referred to as the Wholesale Acquisition Cost (WAC). Wholesalers add a markup when selling to pharmacies, typically around 2-5% of the WAC. Pharmacies then add their own markup when dispensing to patients, which can vary widely depending on the type of pharmacy and medication.
Complicating this picture are pharmacy benefit managers (PBMs), who negotiate rebates from manufacturers on behalf of insurers. These rebates can significantly reduce the net price paid, but these savings aren’t always passed directly to consumers. Additionally, various fees are exchanged between these entities, further obscuring the true cost flow.
Manufacturer Revenue and Profit Margins
Pharmaceutical manufacturers capture the largest share of prescription drug spending, but understanding their true revenue and profits requires looking beyond list prices. While manufacturers set high list prices, they often provide substantial rebates and discounts to PBMs and insurers. These rebates have grown significantly in recent years, sometimes exceeding 50% of the list price for medications with competition.
Even accounting for these rebates, pharmaceutical manufacturing remains one of the most profitable industries. Research indicates that the pharmaceutical sector consistently achieves profit margins of 15-20%, substantially higher than the average across all industries. These high margins are often justified by the risks and costs associated with drug development, though critics question whether current pricing truly reflects these factors.
It’s worth noting that profit margins vary widely across different types of medications. Generic manufacturers typically operate with much lower margins (often single-digit percentages) and higher volumes, while specialty drug manufacturers may achieve higher margins on lower-volume, high-priced medications.
The Role of Pharmacy Benefit Managers (PBMs)
Pharmacy Benefit Managers have emerged as pivotal—and controversial—players in the prescription drug ecosystem. These middlemen negotiate drug prices and rebates with manufacturers on behalf of insurers and employers, process pharmacy claims, design formularies (lists of covered medications), and manage drug utilization.
The three largest PBMs—CVS Caremark, Express Scripts, and OptumRx—control approximately 80% of the market. This concentration has raised concerns about their influence over drug pricing and accessibility. PBMs generate revenue through various mechanisms, including administrative fees, spread pricing (charging insurers more than they pay pharmacies), and retaining portions of manufacturer rebates.
While PBMs argue that they help control costs through negotiated discounts and promoting generic utilization, critics contend that their complex, opaque business models may actually contribute to higher drug prices. The lack of transparency in PBM operations makes it difficult to determine exactly how much of the prescription dollar they retain, but estimates suggest they capture approximately 3-5% of total drug spending.
Pharmacy and Wholesaler Markups
Pharmacies and wholesalers represent the final links in the distribution chain before medications reach patients. Wholesale distributors like McKesson, AmerisourceBergen, and Cardinal Health facilitate the movement of drugs from manufacturers to pharmacies. Their markup is relatively modest, typically 2-5% of the wholesale acquisition cost.
Pharmacies add a more significant markup, combining a professional dispensing fee with a percentage-based markup on the medication itself. The dispensing fee compensates pharmacists for their professional services, including checking for drug interactions, providing counseling, and ensuring appropriate dosing. This fee typically ranges from $8 to $15 per prescription.
The pharmacy’s markup on the drug itself varies widely depending on several factors, including whether the medication is brand-name or generic, the type of pharmacy (independent, chain, mail-order), and the patient’s insurance coverage. For generic medications, this markup can be substantial on a percentage basis, sometimes exceeding 100% of the acquisition cost, though the dollar amount remains relatively small due to the low base cost of most generics.
R&D and Drug Development Costs
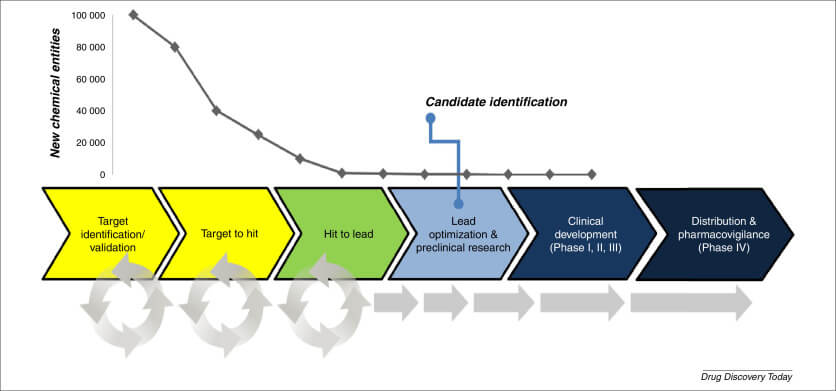
One of the most common justifications for high drug prices in the United States is the cost of research and development. Pharmaceutical companies argue that substantial revenue is necessary to fund the expensive, risky process of developing new medications. But what does the evidence tell us about these costs?
The True Cost of Bringing a Drug to Market
The cost of developing a new medication varies widely depending on the therapeutic area and complexity of the treatment. Recent research provides insights into these costs. Between 2000 and 2018, the mean cost of developing a new drug was approximately $172.7 million (in 2018 dollars)3. However, this figure represents only the direct costs of successful drug development.
When accounting for the cost of drug development failures—a significant factor given that most drug candidates never reach the market—the average cost increases substantially to $515.8 million3. Furthermore, when both failures and capital costs (the opportunity cost of investing money in drug development rather than other investments) are included, the mean expected capitalized cost rises to $879.3 million3.
These costs vary dramatically by therapeutic area. For example, the capitalized cost including failures ranges from $378.7 million for anti-infectives to $1.76 billion for pain and anesthesia drugs3. This variation reflects differences in clinical trial complexity, regulatory requirements, and success rates across different types of medications.
“Studies have estimated that the R&D cost for a new drug ranges from $314 million to $4.46 billion, depending on the therapeutic area, data, and methodology used.”3
It’s important to note that these figures are substantially lower than those often cited by the pharmaceutical industry, which has claimed development costs exceeding $2.5 billion per new drug. The discrepancy arises from differences in methodology, data sources, and the inclusion of various cost components.
How R&D Intensity Has Changed Over Time
The pharmaceutical industry’s investment in research and development, relative to its sales, has increased significantly over time. Between 2008 and 2019, the ratio of R&D spending to total sales—known as R&D intensity—increased from 11.9% to 17.7%3. This occurred despite a 15.6% decline in overall sales during this period, indicating that drug companies maintained or increased their R&D investments even as revenues declined.
For large pharmaceutical companies specifically, R&D intensity increased from 16.6% to 19.3% between 2008 and 2019, while sales increased by 10.0% (from $380.0 to $418.0 billion)3. This suggests a growing commitment to research and development among major industry players, though critics note that marketing expenditures still frequently exceed R&D spending at many large pharmaceutical companies.
The increasing R&D intensity may reflect several factors, including the growing complexity of drug development, stricter regulatory requirements, and a shift toward more complex specialty medications that require more extensive research. It may also represent a strategic response to pressure from investors and policymakers for pharmaceutical companies to demonstrate their commitment to innovation.
Do High Drug Prices Really Fund Innovation?
The relationship between drug prices, pharmaceutical revenue, and innovation is complex and controversial. Pharmaceutical companies argue that high prices in the US market are necessary to fund the risky, expensive process of drug development. They contend that without substantial returns on successful medications, investment in research would decline, ultimately harming patients by reducing the development of new treatments.
Critics counter that much early-stage research is funded by taxpayers through the National Institutes of Health and academic institutions. They also point out that many pharmaceutical companies spend more on marketing, administration, and shareholder returns than on R&D. Additionally, some of the most innovative new drugs are developed by small biotechnology companies rather than the large pharmaceutical firms that charge the highest prices.
The evidence suggests a nuanced reality. While pharmaceutical R&D is indeed expensive and risky, and industry funding is crucial for bringing new medications to market, the current pricing system in the US may provide returns well beyond what is necessary to sustain innovation. Many countries with substantially lower drug prices still maintain vibrant pharmaceutical research sectors, suggesting that the extreme prices seen in the US market may not be essential for continued drug development.
Who Bears the Cost Burden?
Understanding who ultimately pays for prescription drugs helps illuminate the real-world impact of pharmaceutical spending. The burden of drug costs is distributed across various stakeholders, including patients, insurers, employers, and government programs, though not equally.
Out-of-Pocket Spending Trends
Despite the dramatic increase in total prescription drug spending over the past decade, out-of-pocket costs paid directly by patients have remained relatively stable. Between 2010 and 2020, out-of-pocket prescription drug costs actually decreased slightly, from $48 billion to $47 billion4. This represents a declining share of total drug spending, as overall pharmaceutical expenditures increased by 77% during this same period4.
However, these aggregate figures mask significant variations in patient experiences. For most Americans with good insurance coverage, out-of-pocket costs remain manageable, particularly for common generic medications. But for patients who need expensive specialty medications or who have high-deductible health plans, out-of-pocket costs can be catastrophic.
The implementation of the Affordable Care Act’s prescription drug coverage provisions and the expansion of manufacturer patient assistance programs have helped reduce out-of-pocket burdens for some patients. However, complex benefit designs with high deductibles, coinsurance (where patients pay a percentage rather than a fixed copay), and tiered formularies can still create significant financial challenges for many Americans.
Insurance Coverage and Reimbursement
Insurance coverage significantly influences both total drug spending and the distribution of costs among stakeholders. Private insurance, Medicare, Medicaid, and other government programs each use different approaches to covering prescription medications.
Medicare Part D, which covers outpatient prescription drugs for Medicare beneficiaries, has become a major component of US drug spending. The program’s structure includes several coverage phases, including an initial deductible, standard coverage, a coverage gap (the “donut hole”), and catastrophic coverage. Recent legislation, including provisions in the Inflation Reduction Act, has made significant changes to this structure, including capping out-of-pocket costs at $2,000 beginning in 20251.
Private insurance coverage varies widely depending on the specific plan design. Most commercial plans use tiered formularies that provide stronger coverage for preferred generic and brand-name drugs while requiring higher cost-sharing for non-preferred medications. Many plans have also implemented utilization management tools such as prior authorization and step therapy to control spending on high-cost medications.
Medicaid programs, which vary by state, typically provide relatively comprehensive drug coverage with limited cost-sharing for beneficiaries. Federal regulations require manufacturers to provide substantial rebates to Medicaid programs, resulting in lower net prices than those paid by Medicare or commercial insurers.
Geographic Variations in Drug Spending
States with Highest Per-Household Prescription Costs
Prescription drug spending varies significantly across different regions of the United States. Nationally, prescriptions cost an average of $4,571 per household annually4. However, this figure masks substantial state-by-state variations.
Delaware has the highest per-household prescription costs at $6,513, followed by Kentucky ($6,033) and Tennessee ($6,007)4. These three states stand out as the only ones with average household prescription costs exceeding $6,000 annually. At the other end of the spectrum, several states have significantly lower average costs, reflecting differences in population health, prescribing patterns, and insurance coverage.
These geographic variations stem from multiple factors, including:
- Demographic differences (age, income, education levels)
- Prevalence of chronic conditions
- Access to healthcare services
- Insurance coverage rates and types
- Prescribing practices among local healthcare providers
- State policies regarding drug pricing and coverage
Demographic Factors Affecting Drug Spending
Beyond geographic variations, demographic factors significantly influence prescription drug spending patterns. Age is perhaps the most important determinant, with older adults using substantially more medications than younger populations. Americans aged 65 and older take an average of 4-5 prescription medications regularly, compared to just 1-2 for those under 40.
Income and insurance status also play crucial roles. Higher-income individuals tend to have better insurance coverage and greater access to healthcare services, potentially leading to more prescriptions. However, they may also be healthier on average and require fewer medications for chronic conditions.
Gender differences are also noteworthy, with women generally filling more prescriptions than men across most age groups. This discrepancy reflects both biological differences and variations in healthcare utilization patterns.
Race and ethnicity correlate with prescription drug use as well, though these associations are complex and intertwined with socioeconomic factors, healthcare access, and the prevalence of certain health conditions. These demographic factors combine to create the complex mosaic of prescription drug utilization and spending across the American population.
The Concentration of Drug Spending
One of the most striking aspects of US pharmaceutical spending is how concentrated it has become among a small percentage of patients and medications. This concentration has profound implications for drug pricing, insurance design, and healthcare policy.
How Few Patients Account for Half of All Spending
The concentration of drug spending among a small subset of patients has intensified dramatically over time. In 2001, 6.0% of the US population accounted for half of all prescription drug spending5. By 2018, this had decreased to just 2.3% of the population5. This means that a vanishingly small proportion of Americans now generate half of all pharmaceutical expenditures.
This concentration reflects several factors. First, the rise of extremely high-cost specialty medications means that a single patient with a condition like hemophilia, certain cancers, or rare genetic disorders may generate hundreds of thousands of dollars in annual drug costs. Second, patients with multiple chronic conditions often require numerous medications, creating high per-patient spending even without specialty drugs. Finally, the growing availability of low-cost generic medications for common conditions means that most patients generate relatively modest drug expenses.
This concentration creates challenges for insurance design and healthcare financing. Insurance functions best when risk is broadly distributed across a large population. As drug spending becomes increasingly concentrated, insurers face greater pressure to identify and potentially avoid high-cost patients, potentially limiting access to needed medications for the most vulnerable.
The Top 10% of Drugs: Where the Money Goes
Just as spending is concentrated among a small percentage of patients, it’s also concentrated among a small percentage of drugs. The top 10% of drugs by price make up fewer than 1% of all prescriptions but account for 15% of retail spending and 20-25% of non-retail spending1. This remarkable concentration illustrates how a handful of expensive medications drive overall pharmaceutical expenditures.
The therapeutic categories dominating this high-cost segment include:
- Oncology (cancer) treatments
- Immunomodulators for conditions like rheumatoid arthritis and psoriasis
- Medications for multiple sclerosis
- Treatments for rare genetic disorders
- Antivirals, particularly for HIV and hepatitis C
- Novel diabetes treatments
Many of these medications represent significant therapeutic advances and provide substantial benefits to patients. However, their extreme prices—often exceeding $100,000 per patient per year—raise serious questions about affordability and sustainability for the healthcare system.
Medicare Part D Spending Concentration
The concentration of drug spending is particularly pronounced in Medicare Part D, which provides prescription drug coverage for seniors and certain disabled individuals. In 2021, the 10 top-selling Part D drugs accounted for just 0.3% of covered drugs but represented 22% of total gross Part D spending5. This extreme concentration illustrates the outsized impact of a handful of medications on program expenditures.
This concentration has increased over time. Between 2010 and 2015, net spending on specialty drugs in Medicare Part D increased from $8.7 billion to $32.8 billion, with their share of total net drug spending rising from 13% to 31%5. The Congressional Budget Office anticipates this trend will continue, with specialty drugs consuming an ever-larger share of Part D spending.
This concentration creates particular challenges for Medicare, given its role in providing coverage for older Americans who typically use more medications than younger populations. The program’s original design, which included substantial cost-sharing and a coverage gap, was not well-suited to addressing the needs of beneficiaries requiring very high-cost medications. Recent reforms, including those in the Inflation Reduction Act, aim to address these challenges by capping out-of-pocket costs and enabling Medicare to negotiate prices for certain high-cost drugs.
Policy Interventions and Future Outlook
As prescription drug spending continues to rise, policymakers have implemented and proposed various interventions to control costs while maintaining innovation and ensuring patient access. These efforts take many forms, from direct price negotiations to market-based incentives.
Impact of the Inflation Reduction Act
The Inflation Reduction Act (IRA) of 2022 represents one of the most significant reforms to prescription drug pricing in decades, particularly for Medicare beneficiaries. Several key provisions directly address drug costs:
- Medicare Drug Price Negotiation: For the first time, the legislation authorizes the Secretary of Health and Human Services to negotiate prices for selected high-cost drugs in Medicare Parts B and D. The first group of drugs for negotiation will be identified in 2023, with negotiated prices taking effect in 20261.
- Inflation Rebates: The IRA requires manufacturers who raise prices faster than inflation to pay rebates to Medicare. This provision aims to discourage excessive year-over-year price increases, particularly for brand-name drugs that account for 80% of prescription drug spending1.
- Out-of-Pocket Cost Caps: Beginning in 2025, the law caps Medicare beneficiaries’ out-of-pocket prescription drug costs at $2,000 annually. It also eliminates cost-sharing in the catastrophic phase of the Part D benefit and expands the low-income subsidy program1.
- Insulin Cost Caps: The legislation caps Medicare Part B and Part D insulin cost-sharing at $35 per insulin product per month beginning in 2023, providing immediate relief for millions of diabetic seniors1.
These provisions target the primary drivers of increased prescription drug spending—particularly high prices for brand-name drugs and year-over-year price increases for existing medications. By addressing these factors, the IRA aims to slow the growth in Medicare drug spending while improving affordability for beneficiaries.
Medicare Drug Price Negotiation
The Medicare drug price negotiation provision of the Inflation Reduction Act deserves particular attention, as it represents a fundamental shift in how the US approaches pharmaceutical pricing. Unlike most other developed countries, the US has historically not leveraged the government’s purchasing power to negotiate drug prices directly with manufacturers.
Under the new program, drugs become eligible for negotiation based on several criteria:
- Absence of generic or biosimilar competitors
- Total spending in Medicare Parts B and D
- Time elapsed since FDA approval
By targeting the highest-spending drugs without competition, this provision aims to address a key driver of pharmaceutical expenditures. The Congressional Budget Office estimates that this provision, along with other drug pricing reforms in the IRA, will reduce federal deficits by approximately $237 billion over the next decade.
The implementation of this program will be closely watched by all stakeholders. Pharmaceutical manufacturers have expressed concerns that reduced revenues could hamper innovation, while patient advocates hope the reforms will improve affordability without compromising access to new treatments.
Future Projections and Market Trends
Looking ahead, several trends are likely to shape the future of prescription drug spending in the United States:
- Continued Growth in Specialty Medications: The pipeline of drugs in development is heavily weighted toward specialty medications, including cell and gene therapies, targeted cancer treatments, and biologics for autoimmune conditions. These high-cost treatments will likely continue t
Citations:
- https://aspe.hhs.gov/sites/default/files/documents/88c547c976e915fc31fe2c6903ac0bc9/sdp-trends-prescription-drug-spending.pdf
- https://www.singlecare.com/blog/news/prescription-drug-statistics/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11214120/
- https://www.valuepenguin.com/pharmaceutical-spending-study
- https://www.jmcp.org/doi/10.18553/jmcp.2024.30.12.1355
- https://www.ahip.org/news/articles/new-study-in-the-midst-of-covid-19-crisis-7-out-of-10-big-pharma-companies-spent-more-on-sales-and-marketing-than-r-d
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9383648/
- https://www.statista.com/statistics/265100/us-pharmaceutical-industry-spending-on-research-and-development-since-1990/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11482634/
- https://www.statista.com/statistics/184914/prescription-drug-expenditures-in-the-us-since-1960/
- https://www.pwc.com/us/en/industries/health-industries/library/behind-the-numbers.html
- https://www.statista.com/statistics/265085/research-and-development-expenditure-us-pharmaceutical-industry/
- https://schaeffer.usc.edu/research/flow-of-money-through-the-pharmaceutical-distribution-system/
- https://www.actuary.org/content/prescription-drug-spending-us-health-care-system
- https://www.beckershospitalreview.com/supply-chain/5-quotes-on-managing-high-drug-costs-from-ascension-s-coo/
- https://www.drugchannels.net/2024/02/latest-cms-data-reveal-truth-about-us.html
- https://www.vizientinc.com/newsroom/news-releases/2025/vizient-forecasts-a-3-84-percent-rise-in-pharmacy-spending
- https://www.csrxp.org/icymi-new-study-finds-big-pharma-spent-more-on-sales-and-marketing-than-rd-during-pandemic/
- https://www.kff.org/other/poll-finding/public-opinion-on-prescription-drugs-and-their-prices/
- https://www.healthsystemtracker.org/indicator/spending/national-spending-services/
- https://www.healthsystemtracker.org/chart-collection/recent-forecasted-trends-prescription-drug-spending/
- https://www.statista.com/statistics/618857/total-federal-drug-control-spending-in-us/
- https://www.statista.com/statistics/265055/us-pharmaceuticals-spending-on-research-and-development/
- https://bidenwhitehouse.archives.gov/briefing-room/speeches-remarks/2021/12/06/remarks-by-president-biden-on-prescription-drug-costs/
- https://www.ama-assn.org/about/research/trends-health-care-spending
- https://www.magnetaba.com/blog/u-s-pharmaceutical-statistics
- https://www.cnn.com/2021/07/22/tech/prescription-drug-prices-mark-cuban-goodrx-bettermed/index.html
- https://www.abtaba.com/blog/u-s-pharmaceutical-statistics
- https://www.dol.gov/sites/dolgov/files/ebsa/laws-and-regulations/laws/no-surprises-act/2024-report-to-congress-prescription-drug-spending.pdf
- https://www.credenceresearch.com/report/u-s-pharma-rd-outsourcing-market
- https://www.forbes.com/sites/roberthart/2023/02/07/heres-why-big-pharma-spends-more-on-ads-pushing-lower-benefit-drugs-study-suggests/
- https://www.rdworldonline.com/how-much-does-the-pharma-industry-spend-on-rd-anyway-probably-more-than-you-thought/
- https://www.bu.edu/sph/files/2015/05/Pharmaceutical-Marketing-and-Research-Spending-APHA-21-Oct-01.pdf
- https://www.cms.gov/data-research/statistics-trends-and-reports/cms-drug-spending
- https://www.drugdiscoverytrends.com/top-pharma-companies-2023-rd-spend/
- https://www.britannica.com/procon/prescription-drug-costs-debate