Before we dive into the specific factors, let’s take a moment to grasp the magnitude of the issue. Healthcare spending in the United States has reached unprecedented levels, far surpassing that of other developed nations. In 2021, US healthcare expenditures amounted to a staggering $4.3 trillion, or $12,914 per person. This figure represents 18.3% of the country’s Gross Domestic Product (GDP), a proportion that has been steadily increasing over the years.
To put this into perspective, consider this:
“The United States spends more on health care as a share of the economy — nearly twice as much as the average OECD country — yet has the lowest life expectancy and highest suicide rates among the 11 nations.” – The Commonwealth Fund
This stark contrast raises important questions about the efficiency and effectiveness of the US healthcare system. So, what exactly is driving these astronomical costs?
Administrative Complexity: The Hidden Culprit
One of the most significant, yet often overlooked, factors contributing to high healthcare costs in the US is the complex administrative landscape. The American healthcare system is a labyrinth of insurance companies, healthcare providers, and government agencies, each with its own set of rules, regulations, and paperwork.
The Burden of Paperwork
Healthcare providers spend an inordinate amount of time on administrative tasks, such as billing, coding, and insurance claims. This not only increases operational costs but also reduces the time healthcare professionals can spend on patient care. A study published in the Annals of Internal Medicine found that administrative costs account for 34.2% of total health care expenditures in the US, twice the amount in Canada.
Multiple Payers and Fragmentation
The US healthcare system is characterized by multiple payers, including private insurance companies, Medicare, Medicaid, and other government programs. This fragmentation leads to increased administrative overhead as healthcare providers must navigate different billing systems, coverage policies, and reimbursement rates for each payer.
Lack of Standardization
The absence of standardized processes across the healthcare industry further exacerbates administrative costs. Different insurers often have varying requirements for prior authorizations, claims submissions, and other administrative procedures, forcing healthcare providers to maintain multiple systems and workflows.
The High Price of Prescription Drugs
Prescription drug costs are another major contributor to the overall healthcare expenditure in the United States. Americans pay significantly more for their medications compared to citizens of other developed nations.
Factors Influencing Drug Prices
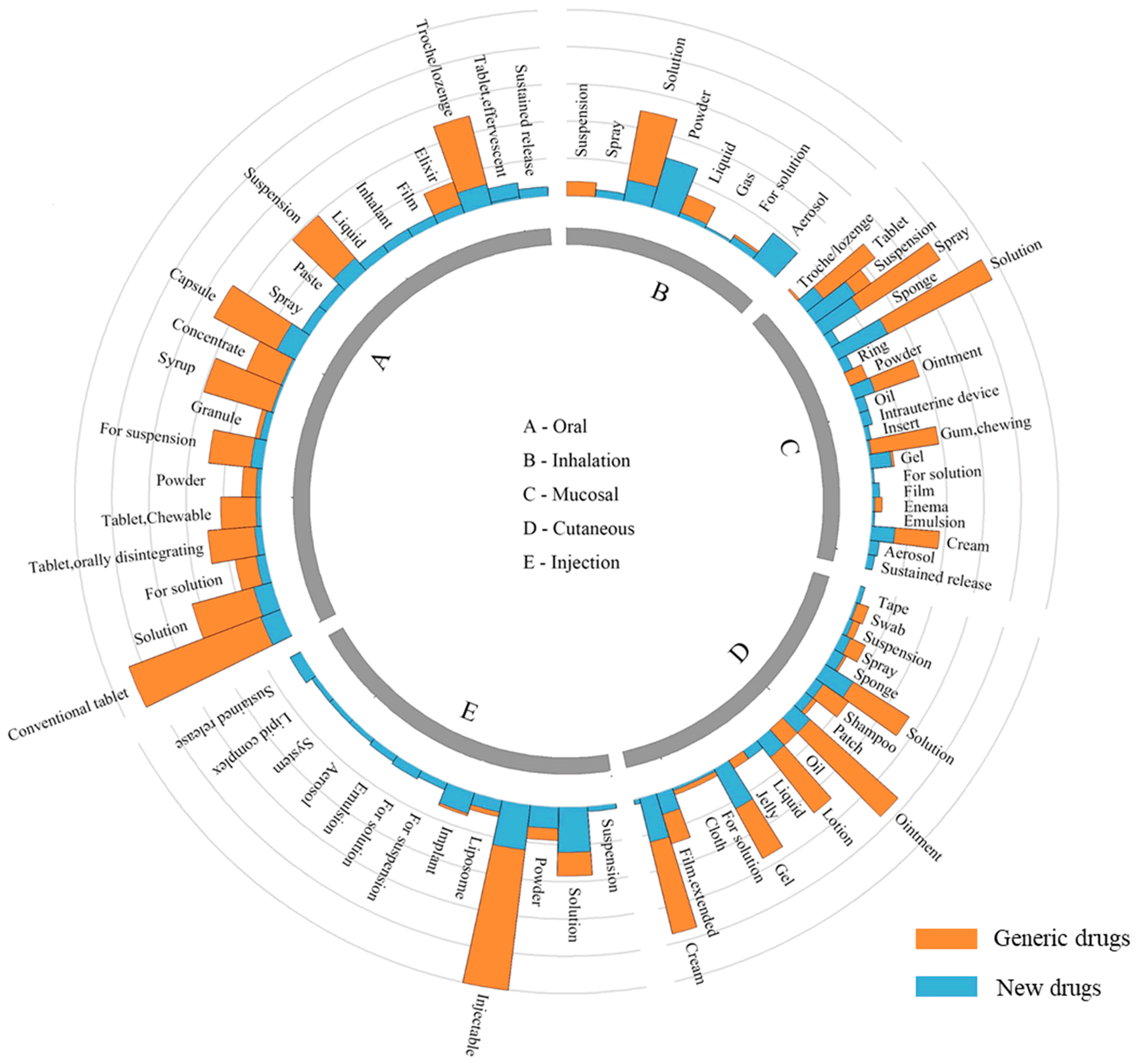
Several factors contribute to the high cost of prescription drugs in the US:
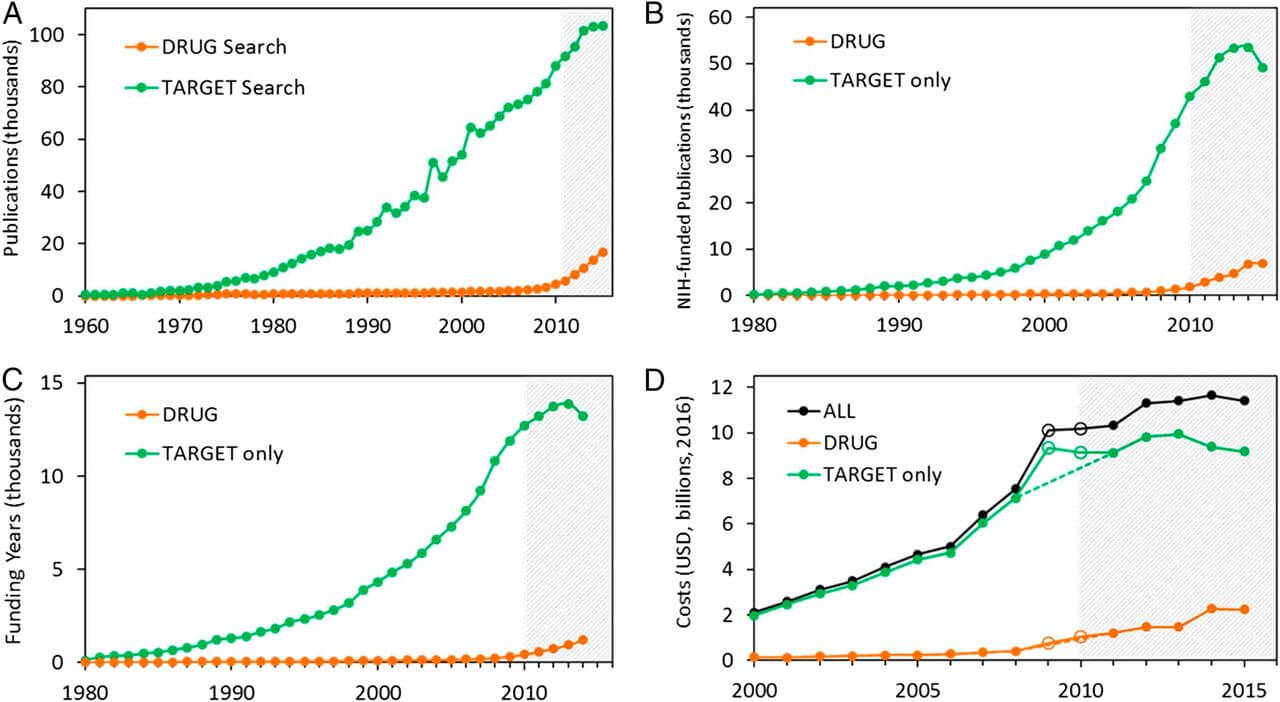
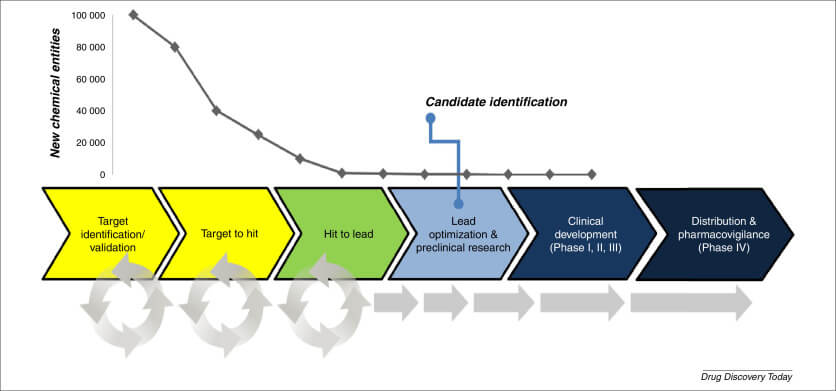
- Research and Development Costs: Pharmaceutical companies often cite the high costs of drug development and clinical trials as justification for steep prices.
- Patent Protection: Brand-name drugs enjoy patent protection, allowing manufacturers to maintain monopoly pricing for extended periods.
- Limited Negotiation Power: Unlike many other countries, the US government does not directly negotiate drug prices with pharmaceutical companies, leading to higher costs.
- Marketing Expenses: Pharmaceutical companies spend billions on marketing and advertising, costs that are ultimately passed on to consumers.
The Impact on Patients
The high cost of prescription drugs has a direct impact on patient care and health outcomes. A survey conducted by the Kaiser Family Foundation found that 29% of American adults reported not taking their medicines as prescribed due to costs. This non-adherence can lead to worsening health conditions and increased healthcare utilization in the long run.
The Role of Technology: A Double-Edged Sword
Technological advancements in healthcare have revolutionized patient care, enabling more accurate diagnoses and effective treatments. However, these innovations come at a cost, contributing significantly to rising healthcare expenses.
Cutting-Edge Medical Equipment
State-of-the-art medical equipment, such as MRI machines, robotic surgical systems, and advanced imaging technologies, come with hefty price tags. Hospitals and healthcare facilities invest millions in acquiring and maintaining these technologies, costs that are ultimately reflected in patient bills.
Health Information Technology
While electronic health records (EHRs) and other health information technologies have the potential to improve efficiency and reduce errors, their implementation and maintenance can be expensive. The initial investment in these systems, along with ongoing updates and staff training, adds to overall healthcare costs.
Overutilization of Technology
The availability of advanced diagnostic tools can sometimes lead to their overuse. Defensive medicine practices, where healthcare providers order excessive tests to avoid potential malpractice claims, contribute to unnecessary healthcare spending.
The Aging Population and Chronic Diseases
Demographic shifts and changing health patterns in the US population play a significant role in driving healthcare costs.
The Silver Tsunami
As the baby boomer generation ages, the proportion of elderly Americans is increasing rapidly. Older adults typically require more frequent and intensive medical care, leading to higher healthcare utilization and costs.
The Rise of Chronic Diseases
Chronic conditions such as diabetes, heart disease, and obesity are becoming increasingly prevalent in the US population. These conditions often require long-term management and treatment, contributing to sustained healthcare costs over time.
“Chronic diseases are responsible for 7 of 10 deaths each year, and treating people with chronic diseases accounts for most of our nation’s health care costs.” – Centers for Disease Control and Prevention
The Fee-for-Service Model: Incentivizing Quantity Over Quality
The predominant payment model in the US healthcare system, known as fee-for-service, has been criticized for incentivizing the volume of services provided rather than the quality of care.
Misaligned Incentives
Under the fee-for-service model, healthcare providers are reimbursed based on the number of services or procedures they perform. This can lead to unnecessary tests, treatments, or hospitalizations, driving up overall healthcare costs.
Lack of Coordination
The fee-for-service model often results in fragmented care, as there’s little incentive for providers to coordinate services or focus on preventive care. This lack of coordination can lead to duplicative services and inefficient use of resources.
The Impact of Malpractice Insurance and Defensive Medicine
The fear of malpractice lawsuits has a significant impact on healthcare costs in the United States.
High Malpractice Insurance Premiums
Healthcare providers, particularly those in high-risk specialties, pay substantial premiums for malpractice insurance. These costs are often passed on to patients in the form of higher fees for medical services.
Defensive Medicine Practices
To protect themselves from potential lawsuits, many healthcare providers practice defensive medicine, ordering excessive tests or procedures that may not be medically necessary. A study published in the Journal of the American Medical Association estimated that defensive medicine costs the US healthcare system $46 billion annually.
The Influence of Lifestyle Factors
Individual lifestyle choices and behaviors have a significant impact on healthcare costs in the United States.
Obesity Epidemic
The rising prevalence of obesity in the US population is a major driver of healthcare costs. Obesity is associated with numerous chronic health conditions, including diabetes, heart disease, and certain cancers, all of which require ongoing medical management.
Sedentary Lifestyles
Lack of physical activity contributes to poor health outcomes and increased healthcare utilization. The CDC estimates that physical inactivity and its associated health problems cost the US healthcare system $117 billion annually.
Substance Abuse and Addiction
The ongoing opioid crisis and other substance abuse issues contribute significantly to healthcare costs. Treatment for addiction, as well as managing the health consequences of substance abuse, places a substantial burden on the healthcare system.
The Role of Health Insurance
The structure and dynamics of the health insurance market in the United States play a crucial role in driving healthcare costs.
Administrative Overhead
Health insurance companies incur significant administrative costs, including marketing, underwriting, and claims processing. These expenses are ultimately reflected in higher premiums for consumers.
Limited Competition
In many regions of the US, there’s limited competition among health insurance providers. This lack of competition can lead to higher premiums and reduced incentives for insurers to negotiate lower prices with healthcare providers.
Cost-Shifting
When healthcare providers treat uninsured patients or receive low reimbursement rates from government programs like Medicare and Medicaid, they often shift these costs to privately insured patients. This practice contributes to higher insurance premiums and out-of-pocket costs for those with private insurance.
The Impact of Government Policies and Regulations
Government policies and regulations, while often intended to improve healthcare quality and access, can sometimes have unintended consequences that drive up costs.
Regulatory Compliance Costs
Healthcare providers and insurers must comply with a complex web of federal and state regulations. The costs associated with compliance, including staff training, documentation, and reporting, are ultimately passed on to consumers.
Certificate of Need Laws
Many states have Certificate of Need (CON) laws that require healthcare providers to obtain approval before expanding services or purchasing certain equipment. While intended to control costs, these laws can sometimes limit competition and innovation, potentially leading to higher prices.
Tax Subsidies for Employer-Sponsored Insurance
The tax-exempt status of employer-sponsored health insurance premiums has been criticized for obscuring the true cost of healthcare and potentially encouraging overutilization of services.
The Shortage of Healthcare Professionals
A growing shortage of healthcare professionals, particularly in certain specialties and geographic areas, contributes to rising healthcare costs.
Supply and Demand Imbalance
As demand for healthcare services increases, the limited supply of healthcare professionals can lead to higher wages and increased costs for healthcare providers.
Training Costs
The high cost of medical education and training contributes to the overall expense of healthcare. Many healthcare professionals graduate with significant student loan debt, which can influence their career choices and salary expectations.
Burnout and Turnover
High levels of burnout among healthcare professionals can lead to increased turnover rates, requiring healthcare organizations to spend more on recruitment and training.
The Role of Consolidation in the Healthcare Industry
Mergers and acquisitions in the healthcare industry have become increasingly common, with significant implications for healthcare costs.
Reduced Competition
Hospital and health system consolidation can lead to reduced competition in local markets, potentially resulting in higher prices for medical services.
Increased Bargaining Power
Larger healthcare systems often have more bargaining power when negotiating with insurance companies, which can lead to higher reimbursement rates and, ultimately, higher costs for consumers.
Integration Costs
The process of integrating merged healthcare organizations can be expensive, with costs often passed on to patients and insurers.
The Influence of Social Determinants of Health
Social and economic factors play a crucial role in shaping health outcomes and healthcare utilization patterns.
Health Disparities
Socioeconomic disparities can lead to differences in health status and access to care, often resulting in higher healthcare costs for disadvantaged populations.
Housing and Food Insecurity
Unstable housing and lack of access to nutritious food can exacerbate health problems and increase healthcare utilization.
Education and Health Literacy
Lower levels of education and health literacy can lead to poor health behaviors and difficulties in navigating the healthcare system, potentially resulting in higher costs.
The Impact of End-of-Life Care
End-of-life care represents a significant portion of healthcare spending in the United States.
Intensive Care Utilization
A disproportionate amount of healthcare spending occurs in the last year of life, often involving intensive care and expensive interventions.
Lack of Advance Care Planning
Insufficient advance care planning can lead to unwanted and costly medical interventions at the end of life.
Cultural Attitudes Towards Death
Cultural attitudes that prioritize prolonging life at all costs can contribute to expensive and potentially futile medical interventions near the end of life.
Potential Solutions and Future Outlook
Addressing the complex factors driving healthcare costs in the US requires a multifaceted approach. Here are some potential solutions that policymakers, healthcare providers, and other stakeholders are exploring:
Value-Based Care Models
Transitioning from fee-for-service to value-based care models could help align incentives with quality outcomes rather than volume of services.
Price Transparency Initiatives
Increasing price transparency could help consumers make more informed decisions about their healthcare and potentially drive competition among providers.
Administrative Simplification
Streamlining administrative processes and standardizing procedures across the healthcare industry could significantly reduce costs.
Drug Pricing Reforms
Policies aimed at reducing prescription drug costs, such as allowing Medicare to negotiate drug prices, could help curb one of the fastest-growing components of healthcare spending.
Emphasis on Preventive Care
Investing in preventive care and addressing social determinants of health could lead to better health outcomes and reduced healthcare utilization in the long term.
Telehealth and Digital Health Solutions
Leveraging technology to provide more efficient and accessible care could help reduce costs while improving patient outcomes.
Key Takeaways
- Administrative complexity is a major driver of healthcare costs in the US, accounting for a significant portion of total healthcare expenditures.
- High prescription drug prices contribute substantially to overall healthcare costs, impacting patient adherence and health outcomes.
- Technological advancements in healthcare, while improving patient care, also drive up costs through expensive equipment and potential overutilization.
- The aging population and rising prevalence of chronic diseases are increasing healthcare utilization and costs.
- The fee-for-service payment model can incentivize quantity over quality, leading to unnecessary services and higher costs.
- Lifestyle factors, such as obesity and sedentary behaviors, significantly impact healthcare costs.
- The structure of the health insurance market, including administrative overhead and limited competition, contributes to rising costs.
- Government policies and regulations can have unintended consequences that drive up healthcare expenses.
- Shortages of healthcare professionals and industry consolidation can lead to higher costs for medical services.
- Addressing social determinants of health and improving end-of-life care practices could help reduce overall healthcare spending.
FAQs
- Q: How does the US healthcare system compare to other developed countries in terms of cost?
A: The US healthcare system is significantly more expensive than those of other developed countries. The US spends nearly twice as much on healthcare as a percentage of GDP compared to the average OECD country, yet often achieves poorer health outcomes. - Q: What role does technology play in driving healthcare costs?
A: While technology has improved patient care, it also contributes to rising costs through expensive equipment, implementation of health information systems, and potential overutilization of diagnostic tools. - Q: How do prescription drug prices in the US compare to other countries?
A: Prescription drug prices in the US are generally much higher than in other developed countries. This is due to factors such as limited government negotiation power, patent protections, and high marketing expenses. - Q: What is the impact of the aging population on healthcare costs?
A: The aging population contributes to rising healthcare costs as older adults typically require more frequent and intensive medical care. This demographic shift, often referred to as the “Silver Tsunami,” is expected to continue driving healthcare utilization and costs in the coming years. - Q: How can individuals help reduce healthcare costs?
A: Individuals can contribute to reducing healthcare costs by adopting healthy lifestyle habits, engaging in preventive care, using healthcare resources judiciously, and being informed consumers of healthcare services. Additionally, participating in wellness programs and managing chronic conditions effectively can help reduce long-term healthcare expenses.
Resources:
: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical
: https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019
: https://www.acpjournals.org/doi/10.7326/M19-2818
: https://www.kff.org/health-costs/poll-finding/kff-health-tracking-poll-february-2019-prescription-drugs/
: https://www.cdc.gov/chronicdisease/about/index.htm
: https://jamanetwork.com/journals/jama/fullarticle/203453
: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/physical-activity.htm