This paper was originally published by Melek Simsek, Berrie Meijer, Adriaan A.van Bodegraven, Nanne K.H. de Boer, and Chris J.J. Mulder in Drug Discovery Today Volume 23, Issue 1, January 2018, Pages 17-21 under a Creative Commons license.
Introduction
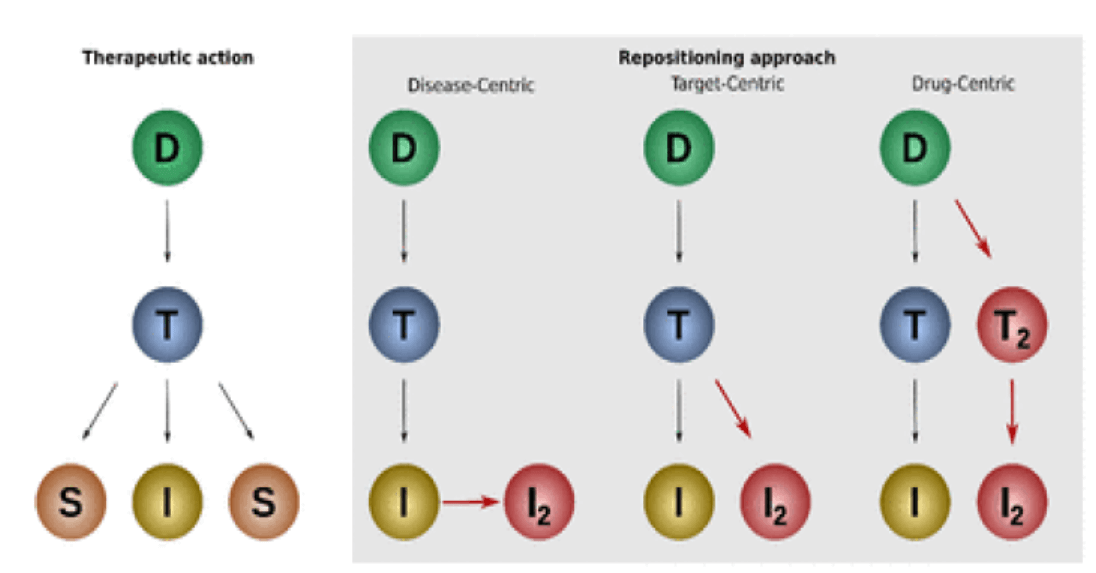
The process of finding new purposes for existing drugs is better known as drug rediscovery, drug repurposing or drug repositioning, and might be an emerging topic but it is not a new concept. Several successfully rediscovered drugs are generally used in daily practice. Sildenafil, for example, was initially intended for the treatment of angina pectoris but, owing to persistent erections as an unexpected adverse event it, was repurposed as a therapy for erectile dysfunction (Viagra®) [1]. Likewise, minoxidil was developed to treat ulcers, but in the early trials the drug proved to be a vasodilator, and was consecutively repurposed for severe hypertension [2]. Then, the efficacy trials of minoxidil as an antihypertensive agent showed unexpected hair growth as a side effect and this drug was repositioned for the treatment of alopecia [3]. Many successful drug rediscoveries were serendipitous, and thus fortunate, cases and took place during or before market exclusivity of the drug. However, drugs that are already approved can also be repositioned for new indications. Here, thalidomide can be used as an example; it was approved for morning sickness in pregnant women in the 1950s and repositioned for the treatment of multiple myeloma in 2006 [4].
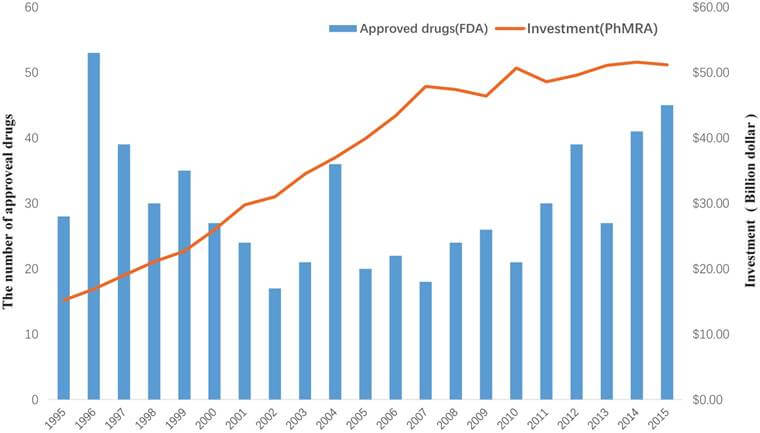
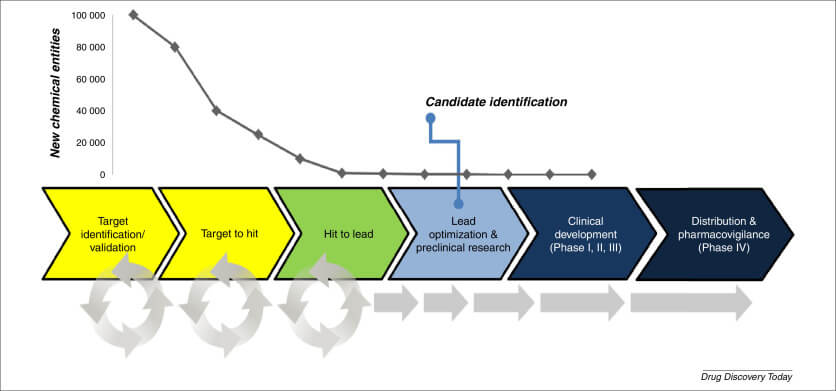
Drug rediscovery has (financial) advantages over traditional drug development, which is expensive and time-consuming [5]. Because the drug has been studied and used before there is extensive knowledge about the safety and quality of the repurposed drug available. Also, there is a subsequently reduced risk of unexpected side effects. Unfortunately, drug repositioning could also be exploited by pharmaceutical companies causing excessive pricing, putting the economic advantages before therapeutic benefits [6].
In The Netherlands, as well as in other European countries, the rediscovery of generic drugs is a challenging pursuit because there is no standardized regulatory approach or marketing regulation available. This lack of legal framework was underlined when thioguanine, originally developed for leukemia, was repurposed as a rescue immunosuppressive drug for the treatment of patients with inflammatory bowel disease (IBD) in 2001 [7]. To broaden the spectrum of treatment options and create awareness about alternative therapies for IBD, a re-registration of thioguanine was proposed by the European Thioguanine Working Party [8]. Initially, pharmaceutical and health insurance companies showed no interest for various reasons, including but not limited to pharmaceutical (an expired patent), medical (controversial results of this drug in early clinical trials) and financial (reimbursement) issues. Additionally, there was no guidance provided by governmental institutions because established regulatory procedures for the rediscovery of generic drugs are nonexistent. Despite these obstacles, thioguanine was re-registered, under conditions, for the treatment of patients with IBD in The Netherlands years later. This unique development created awareness about the importance of rediscovery and further development of old drugs.
History and repurposing of thioguanine
The discovery of thioguanine dates back more than 65 years when it was originally developed to treat leukemia in children (Fig. 1) [9]. In 1988, Gertrude Elion and George Hitchings received the Nobel Prize (1988), among their academic achievements was the discovery of thioguanine and the better known conventional thiopurine derivatives: azathioprine and mercaptopurine. Because of the established immunosuppressive effects in early laboratory experiments, azathioprine and mercaptopurine were slowly adapted in the prevention of organ transplant rejection and the management of chronic idiopathic inflammatory diseases such as rheumatoid arthritis and IBD 10, 11. Thioguanine, by contrast, was losing its popularity in the treatment of hematological conditions owing to more-effective drugs being introduced to the market.
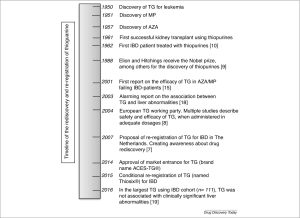
Figure 1. Timeline of thioguanine from discovery to rediscovery and re-registration. Abbreviations: TG, thioguanine; AZA, azathioprine; MP, mercaptopurine; IBD, inflammatory bowel disease.
Although thiopurines are ‘ancient’ drugs, their mechanism of action and extensive metabolism have only been elucidated recently [12]. Thioguanine, azathioprine and mercaptopurine are metabolized via an extensive pathway into the same therapeutically effective end-metabolites: 6-thioguanine nucleotides (Fig. 2). In contrast to azathioprine and mercaptopurine, the metabolic pathway of thioguanine takes one step with minimal production of potentially toxic metabolites, such as 6-methylmercaptopurine. Hence, thioguanine was used as an escape drug for IBD patients who had to discontinue azathioprine or mercaptopurine therapy owing to intolerance or resistance (up to 50% in the first two years of treatment) 13, 14. Several early trials conducted to evaluate the efficacy of thioguanine in IBD treatment described that up to 80% of these patients were able to tolerate this drug and experienced clinical benefit from its use 15, 16, 17. These promising results were overshadowed by a clinically alarming association of high dosages of thioguanine with the development of nodular regenerative hyperplasia of the liver [18]. Subsequently, in several trials, it was demonstrated that thioguanine did not increase the risk of liver abnormalities when given in low but therapeutically adequate dosages (0.2–0.3 mg/kg, not exceeding 25 mg per day) [19]. The presence of histologically relevant changes indicative for nodular regenerative hyperplasia appeared to be dose dependent [20]. Moreover, it was demonstrated that histopathological nodular regenerative hyperplasia rarely led to symptoms of portal hypertension and was clinically insignificant in most patients 19, 21. To reach the full rediscovery potential of thioguanine for IBD, a re-registration of this drug was proposed to and repeatedly discussed with governmental institutions like the Ministry of Health, Welfare and Sports (VWS) and the Dutch Medicines Evaluation Board (MEB) [7]. This proposal created awareness about drug rediscovery, and the importance of safe and efficient use of existing drugs was recognized by health institutes in The Netherlands [7].

The importance of and the challenges in rediscovery of old drugs
Finding alternative treatment options by repurposing generic drugs could bypass much of the costs and time needed to develop new drugs. In actuality, however, multiple obstacles impair the realization of a potential new use for an old drug [7]. Rediscovered drugs are regularly prescribed off-label, thus unlicensed. In fact, physicians prescribe drugs for an unapproved indication up to 20% of the time [22]. In the treatment of IBD, for example, cyclosporine and beclomethasone are common unlicensed prescriptions 23, 24. Although data regarding off-label prescriptions are crucial to assess efficacy, safety and quality of the drug, they are not always recorded. Drug manufacturing by a pharmaceutical company has the benefit of guaranteed standardized drug quality control and official product information providing doctors and patients with accurate information about drug usage, as compared with off-label usage [25].
A major drawback in the rediscovery of generic drugs is the lack of interest by pharmaceutical and other stakeholders in drugs with an expired patent. Repurposed drugs do not guarantee market exclusivity or recoupment of investments. However, in the EU and the USA there are ways to extend the market exclusivity period of protected drugs [26]. Adding therapeutic indications and enlarging the patient population are standard practice in pharmaceutical economics. In the regulation of generic drugs, however, there are crucial differences between the EU and the USA [27]. In the USA, the FDA offers market exclusivity for 3 years for the development of new indications for an already approved drug through an Abbreviated New Drug Application (ANDA) [28]. Although the application follows a clear-cut route, the 3-year period is often not tempting enough for pharmaceutical companies to invest in repurposed generic drugs. In the EU, a harmonized regulatory procedure for generic drugs is not yet established and drug policies differ between European countries 27, 29. The European Medicines Agency (EMA) does not have the final word on drug approval in contrast to the FDA. In Europe, a generic rediscovered drug application can be submitted several ways, such as via the Mutual Recognition Procedure (MPR) and Decentralized Procedure (DCP). These pathways to approval are long-lasting and have different characteristics in different European countries. If procedures are successfully concluded, 1-year market exclusivity can be obtained for the repurposed generic drug. So, generic drug regulation in the EU provides much less support for drug rediscovery than in the USA.
In the rediscovery of thioguanine, attention was drawn to these obstacles and after a 14-year period (2001–2015) thioguanine was conditionally re-registered for patients with IBD. License approval was given under the condition of maintaining a registration database including all patients using thioguanine and gathering additional data on efficacy. Interestingly, the costs of this whole procedure were in keeping with prevailing market price trends.
Suggestions for optimizing the rediscovery of old drugs
Needless to say, optimal use of old drugs benefits public health. In the EU there is currently no defined structured drug regulatory procedure that ensures the development and licensing of rediscovered generic drugs. A drug regulatory reform and marketing authorization for rediscovered drugs is needed, including governmental regulation, to prevent excessive drug pricing by pharmaceutical companies. In the past, similar difficulties in the management of orphan and pediatric drugs were solved by adopting the regulation in the EU and FDA, demonstrating that benefiting patients with rare diseases was more important than profit [30]. In the rediscovery of generic drugs, such as in the case of thioguanine, a comparable management strategy might be necessary to benefit patients by rescue therapies. Another suggestion could be to adopt a similar policy for rediscovered generic drugs as applied by the FDA [28]. To make this suggestion of financial interest to pharmaceutical companies a prolonged period of market exclusivity regulation should be more than 3 years.
Recognition of these obstacles by the EU and EMA is important to encourage an open dialogue between regulatory authorities and pharmaceutical applicants. Furthermore, a standardized protocol for the rediscovery of generic drugs should be initiated by European health and regulatory authorities to aid this procedure. Such a protocol should assure the protection of patients by preventing inefficacious and unsafe medication from re-entering the market and providing clear instructions for a successful development and clinical use of a rediscovered drug. The quality of the drug (i.e., the drug product and drug substance) should be guaranteed, and attention should be drawn to the purity, manufacturing process (preferably gluten-, dairy- and soy-free) and the pharmaceutical development of the rediscovered drug. The benefit:risk profile (i.e., efficacy and safety of the drug in the population) should be positive and the clinical equivalence of the repurposed drug should be well investigated and proven. Moreover, results from clinical trials should demonstrate that the medical needs of patients are met by the rediscovered drug.
Effect of conditional re-registration of thioguanine on usage
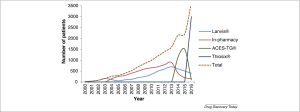
The re-registration of thioguanine for treating patients with IBD led to an increased use of this drug, as depicted in Fig. 3. At the beginning of the 21st century, the original drug (brand name: Lanvis®) was used only by a small number of IBD patients in The Netherlands. The increased usage of thioguanine in IBD led to a shortage of the original drug. From 2004 to 2014 unlicensed pharmacy compounded thioguanine tablets were used, which lacked a standardized drug quality control. In 2014, legislative authorities conditionally approved the market re-entrance of thioguanine (brand name: ACES-TG®). The formal drug licensing occurred 1 year later (brand name: Thiosix®). Since the authorized market approval of thioguanine, there has been a consistent and substantial growth in the number of prescriptions for IBD (currently ∼3000 prescriptions per year).
Concluding remarks
In conclusion, drug rediscovery is invaluable because it can increase therapeutic options and reduce drug-development-associated costs. However, there is a need for a structured protocol for further development of old drugs to optimize licensing and avoid long-lasting procedures, as was the case in the repositioning of thioguanine for IBD in The Netherlands. Regulatory reform and market regulation in Europe are needed to ensure that every generic drug is used to its full potential and to prevent excessive pricing by pharmaceutical companies. Thiosix®, the current conditionally registered thioguanine compound, has been available since 2015 and is increasingly often prescribed for the treatment of IBD in The Netherlands. With the recorded data on thioguanine usage since its re-registration, we ultimately aim to generate additional information regarding the effectiveness and safety of this drug in IBD patients.
Conflicts of interest
The Department of Gastroenterology and Hepatology of the VU University Medical Center received an unrestricted research grant by TEVA Pharma BV for conducting research on thioguanine in inflammatory bowel disease. M.S. and B.M. have nothing to declare. C.J.J.M. has served a principal investigator for TEVA Pharma. A.A.vB. has served as consultant or speaker for AbbVie, Ferring, Janssen, MSD, Pfizer, Takeda, TEVA, Tramedico, VIFOR and Dutch Ministry of Health (ZonMW). He has received unrestricted research grants from Aventis and Ferring, and the Dutch Ministry of Health. N.K.H.dB. has served as a speaker for AbbVie, Takeda and MSD. He has served as consultant and principal investigator for Takeda and TEVA Pharma. He has received research grants from Dr Falk and Takeda.
Acknowledgments
The views and experiences expressed in this article are the personal views of the authors and may not be interpreted as being made on behalf of the health authorities or medical associations involved in the procedure of thioguanine re-registration. The authors would like to thank Professor Hubert Leufkens, former chair of the Dutch Medicines Association Board (MEB) and Professor of Pharmacoepidemiology, for his thoughts on the content of this article.
References
- I. Goldstein, et al. Oral sildenafil in the treatment of erectile dysfunction J. Urol., 167 (1998), pp. 1197-1203
- J. Watkins, et al. Reduction of beta-blocking drugs in hypertensive patients treated with minoxidil Br. Med. J., 1 (1979), p. 1400
- S.P. Clissold, R.C. Heel Topical minoxidil. A preliminary review of its pharmacodynamic properties and therapeutic efficacy in alopecia areata and alopecia androgenetica Drugs, 33 (1987), pp. 107-122
- A. Mercurio, et al. A mini-review on thalidomide: chemistry, mechanisms of action, therapeutic potential and anti-angiogenic properties in multiple myeloma Curr. Med. Chem. (2017), 10.2174/0929867324666170601074646
- J.A. DiMasi, et al. The cost of drug development N. Engl. J. Med., 372 (2015), p. 1972
- M.B. Stanbrook Limiting evergreening for a better balance of drug innovation incentives CMAJ, 185 (2013), p. 939
- C.J. Mulder, et al. Drug rediscovery to prevent off-label prescription reduces health care costs: the case of tioguanine in the Netherlands J. Gastrointestin. Liver Dis., 23 (2014), pp. 123-125
- N.K. de Boer, et al. 6-Thioguanine treatment in inflammatory bowel disease: a critical appraisal by a European 6-TG working party Digestion, 73 (2006), pp. 25-31
- G.B. Elion The purine path to chemotherapy Science, 244 (1989), pp. 41-47
- R.H. Bean The treatment of chronic ulcerative colitis with 6-mercaptopurine Med. J. Aust., 49 (1962), pp. 592-593
- B. Zweiman Immunosuppressive effects of specific classes of agents with special reference to organ transplantation. Immunosuppression by thiopurines Transplant. Proc., 5 (1973), pp. 1197-1201
- D.P. Van Asseldonk, et al. On therapeutic drug monitoring of thiopurines in inflammatory bowel disease; pharmacology, pharmacogenomics, drug intolerance and clinical relevance Curr. Drug Metab., 10 (2009), pp. 981-997
- B. Jharap, et al. Thiopurine therapy in inflammatory bowel disease patients: analyses of two 8-year intercept cohorts Inflamm. Bowel Dis., 16 (2010), pp. 1541-1549
- S.H. Almer, et al. 6-Thioguanine therapy in Crohn’s disease—observational data in Swedish patients Dig. Liver Dis., 41 (2009), pp. 194-200
- M.C. Dubinsky, et al. An open-label pilot study using thioguanine as a therapeutic alternative in Crohn’s disease patients resistant to 6-mercaptopurine therapy Inflamm. Bowel Dis., 7 (2001), pp. 181-189
- K.R. Herrlinger, et al. 6-thioguanine—efficacy and safety in chronic active Crohn’s disease Aliment. Pharmacol. Ther., 17 (2003), pp. 503-508
- B. Meijer, et al. Efficacy of thioguanine treatment in inflammatory bowel disease: a systematic review World J. Gastroenterol., 22 (2016), pp. 9012-9021
- M.C. Dubinsky, et al. 6-thioguanine can cause serious liver injury in inflammatory bowel disease patients Gastroenterology, 125 (2003), pp. 298-303
- D.P. van Asseldonk, et al. The prevalence of nodular regenerative hyperplasia in inflammatory bowel disease patients treated with thioguanine is not associated with clinically significant liver disease Inflamm. Bowel Dis., 22 (2016), pp. 2112-2120
- M.L. Seinen, et al. Dosing 6-thioguanine in inflammatory bowel disease: expert-based guidelines for daily practice J. Gastrointestin. Liver Dis., 19 (2010), pp. 291-294
- I.R. Wanless Micronodular transformation (nodular regenerative hyperplasia) of the liver: a report of 64 cases among 2,500 autopsies and a new classification of benign hepatocellular nodules Hepatology, 11 (1990), pp. 787-797
- D.C. Radley, et al. Off-label prescribing among office-based physicians Arch. Intern. Med., 166 (2006), pp. 1021-1026
- A. Lopez San Roman, E. Garrido Steroids in inflammatory bowel disease Rev. Esp. Enferm. Dig., 107 (2015), p. 573
- M. Guada, et al. Cyclosporine A-loaded lipid nanoparticles in inflammatory bowel disease Int. J. Pharm., 503 (2016), pp. 196-198
- M.C. Nahata, L.V. Allen Jr. Extemporaneous drug formulations Clin. Ther., 30 (2008), pp. 2112-2119
- P. Sandner, K. Ziegelbauer Product-related research: how research can contribute to successful life-cycle management Drug Discov. Today, 13 (2008), pp. 457-463
- O.J. Wouters Comparing generic drug markets in Europe and the U. S.: prices, volumes, and spending Milbank Q. (2017)
- Patents and Exclusivity (2015). Available at: https://www.fda.gov/downloads/drugs/developmentapprovalprocess/smallbusinessassistance/ucm447307.pdf.
- D. Kim Transparency policies of the European Medicines Agency: has the paradigm shifted? Med. Law Rev., 23 (3) (2017), pp. 456-483, 10.1093/medlaw/fwx002
- V. Giannuzzi, et al. Orphan medicinal products in Europe and United States to cover needs of patients with rare diseases: an increased common effort is to be foreseen Orphanet J. Rare Dis., 12 (2017), p. 64