Formulary decisions play a crucial role in determining which medications are available to patients and at what cost. These decisions, made by healthcare organizations, insurance companies, and government agencies, have far-reaching implications for patient care, healthcare costs, and the pharmaceutical industry. As we delve into the ethics of drug approval, we’ll explore the intricate balance between efficacy, safety, cost-effectiveness, and patient access that formulary committees must navigate.
The Fundamentals of Formulary Decisions
What is a Formulary?
A formulary is a comprehensive list of medications approved for use within a healthcare system or insurance plan. It serves as a guide for healthcare providers, pharmacists, and patients, outlining which drugs are covered and under what conditions. Formularies are designed to promote safe, effective, and cost-efficient medication use while ensuring patient access to necessary treatments.
The Role of Formulary Committees
Formulary committees, typically composed of physicians, pharmacists, and other healthcare professionals, are responsible for making decisions about which drugs to include in a formulary. These committees review scientific evidence, clinical data, and economic analyses to determine the value and appropriateness of medications for their patient populations.
The Ethical Framework for Drug Approval
Balancing Beneficence and Non-Maleficence
At the heart of formulary decisions lies the ethical principle of beneficence – the obligation to act in the best interest of patients. Committees must weigh the potential benefits of a drug against its risks, ensuring that approved medications offer a favorable risk-benefit profile. Simultaneously, they must adhere to the principle of non-maleficence, striving to “do no harm” by excluding drugs with unacceptable safety concerns.
Justice and Equity in Access
Ethical formulary decisions must also consider issues of justice and equity. How can we ensure fair access to medications across diverse patient populations? This question becomes particularly pertinent when considering high-cost specialty drugs or treatments for rare diseases.
“Formulary decisions are not just about science and economics; they’re about ensuring equitable access to life-saving treatments for all patients, regardless of their socioeconomic status or geographic location.” – Dr. Elena Rodriguez, Bioethicist at Harvard Medical School
Respect for Patient Autonomy
Respecting patient autonomy is another crucial ethical consideration. While formulary decisions inherently limit patient choice to some degree, committees must strive to maintain a range of treatment options that allow for personalized care and shared decision-making between patients and their healthcare providers.
The Evidence-Based Approach to Drug Evaluation
Assessing Clinical Efficacy
When evaluating drugs for formulary inclusion, committees rely heavily on evidence from clinical trials. They examine factors such as:
- The magnitude of clinical benefit
- The quality and reliability of the evidence
- The relevance of trial outcomes to real-world patient populations
For instance, a study published in the New England Journal of Medicine found that only 54% of new cancer drugs approved by the FDA between 2008 and 2012 showed a significant improvement in overall survival or quality of life.
Safety Considerations
Safety is paramount in formulary decisions. Committees scrutinize adverse event data, potential drug interactions, and long-term safety profiles. They must also consider the potential for off-label use and its associated risks.
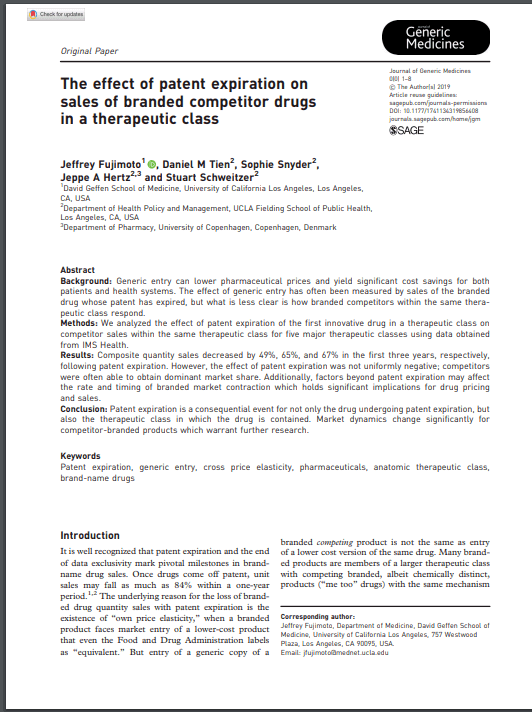
Comparative Effectiveness
In an era of rising healthcare costs, formulary committees increasingly focus on comparative effectiveness – how a new drug compares to existing treatments in terms of efficacy, safety, and cost. This approach helps ensure that formularies include the most valuable treatments rather than simply the newest or most heavily marketed options.
Economic Considerations in Formulary Decisions
Cost-Effectiveness Analysis
Cost-effectiveness analysis (CEA) has become a standard tool in formulary decision-making. CEA compares the relative costs and outcomes of different interventions, typically expressed as quality-adjusted life years (QALYs). While controversial, this approach aims to maximize health benefits within limited budgets.
Budget Impact
Formulary committees must also consider the overall budget impact of including a new drug. This involves projecting the number of patients likely to use the medication and the potential for cost offsets in other areas of healthcare.
Negotiating Drug Prices
The ability to negotiate drug prices plays a significant role in formulary decisions. In some countries, such as the United Kingdom, centralized bodies like the National Institute for Health and Care Excellence (NICE) use their bargaining power to secure better prices for effective treatments.
Ethical Challenges in Specific Drug Categories
Orphan Drugs for Rare Diseases
Orphan drugs, developed to treat rare diseases, present unique ethical challenges. These medications often come with high price tags due to small patient populations and extensive research costs. Formulary committees must grapple with how to provide access to these potentially life-saving treatments while managing limited resources.
Gene Therapies and Personalized Medicine
The advent of gene therapies and personalized medicine has introduced new complexities to formulary decisions. These treatments, often tailored to individual patients, can offer remarkable benefits but at extraordinary costs. How should formulary committees approach these innovative but expensive options?
Mental Health Medications
Formulary decisions regarding mental health medications require special consideration. The subjective nature of many mental health conditions and the variability in patient response to treatments make it challenging to apply standard efficacy metrics. Committees must ensure a range of options while considering potential abuse and dependency issues.
Stakeholder Perspectives in Formulary Decisions
The Patient Voice
Increasingly, formulary committees are recognizing the importance of incorporating patient perspectives into their decision-making processes. Patient advocacy groups argue that those living with conditions have unique insights into the value of treatments that may not be captured by traditional clinical or economic measures.
Physician Input
Healthcare providers play a crucial role in formulary decisions, offering insights into real-world effectiveness, patient preferences, and practical considerations of drug administration. Their input helps ensure that formularies remain clinically relevant and aligned with current best practices.
Pharmaceutical Industry Influence
The pharmaceutical industry’s role in formulary decisions is a subject of ongoing ethical debate. While industry representatives can provide valuable information about new drugs, there are concerns about potential conflicts of interest and the impact of marketing efforts on decision-making.
Transparency and Accountability in Formulary Processes
The Importance of Clear Decision-Making Criteria
To maintain ethical integrity, formulary committees must establish and adhere to clear, publicly available decision-making criteria. This transparency helps build trust among stakeholders and ensures consistency in the evaluation process.
Appeals and Exceptions Processes
Ethical formulary systems include mechanisms for appeals and exceptions. These processes allow for reconsideration of decisions in light of new evidence or unique patient circumstances, ensuring flexibility and responsiveness to individual needs.
Global Perspectives on Formulary Ethics
Variations in National Approaches
Formulary decision-making processes and ethical considerations vary significantly across countries. For example:
- In the United Kingdom, NICE uses a threshold of £20,000 to £30,000 per QALY to determine cost-effectiveness.
- Canada’s Common Drug Review provides recommendations to participating federal, provincial, and territorial public drug plans, but final decisions remain with individual jurisdictions.
- The United States lacks a centralized formulary decision-making body, leading to variations across public and private payers.
Access to Essential Medicines in Low- and Middle-Income Countries
The World Health Organization’s Essential Medicines List serves as a model formulary for many low- and middle-income countries. However, ensuring access to these medications remains a significant ethical challenge, involving issues of global justice, intellectual property rights, and pharmaceutical pricing.
Emerging Trends and Future Challenges
Real-World Evidence and Big Data
The increasing availability of real-world evidence and big data analytics is reshaping formulary decision-making. These tools offer the potential for more nuanced understanding of drug effectiveness and safety in diverse patient populations, but also raise questions about data privacy and interpretation.
Value-Based Pricing and Outcomes-Based Contracts
Innovative pricing models, such as value-based pricing and outcomes-based contracts, are emerging as potential solutions to balance access and affordability. These approaches tie drug prices or reimbursement to real-world performance, potentially aligning incentives between payers, manufacturers, and patients.
Artificial Intelligence in Formulary Decisions
As artificial intelligence (AI) and machine learning technologies advance, they may play an increasing role in formulary decision-making. While these tools offer the potential for more efficient and data-driven decisions, they also raise ethical questions about transparency, bias, and the role of human judgment in healthcare decision-making.
Ethical Decision-Making Frameworks for Formulary Committees
The Accountability for Reasonableness Framework
One widely recognized ethical framework for healthcare priority setting is the Accountability for Reasonableness (A4R) approach, developed by Norman Daniels and James Sabin. This framework emphasizes four key conditions for ethical decision-making:
- Publicity: Decisions and their rationales must be publicly accessible.
- Relevance: The rationales for decisions should be based on evidence, reasons, and principles that fair-minded people can agree are relevant.
- Revision and appeals: There should be mechanisms for challenging and revising decisions in light of new evidence or arguments.
- Enforcement: There should be voluntary or public regulation of the process to ensure that the first three conditions are met.
The Multi-Criteria Decision Analysis Approach
Multi-Criteria Decision Analysis (MCDA) is another approach gaining traction in formulary decision-making. MCDA provides a structured framework for considering multiple, often competing criteria in a transparent and systematic way. This method can help committees balance clinical, economic, and ethical considerations more explicitly.
Case Studies in Formulary Ethics
The Sovaldi Dilemma
The 2013 approval of Sovaldi (sofosbuvir) for hepatitis C treatment presented a stark ethical challenge for formulary committees. The drug offered a cure rate of over 90% for a previously difficult-to-treat condition, but at a cost of $84,000 for a 12-week course. This case highlighted the tension between providing access to highly effective treatments and managing healthcare budgets.
Spinraza and the Challenge of Ultra-Rare Diseases
Spinraza (nusinersen), approved in 2016 for the treatment of spinal muscular atrophy, exemplifies the ethical dilemmas posed by treatments for ultra-rare diseases. With a list price of $750,000 for the first year of treatment and $375,000 annually thereafter, Spinraza forced formulary committees to grapple with questions of fairness, resource allocation, and the value of life.
The Role of Ethics Committees in Formulary Decisions
Collaboration Between Formulary and Ethics Committees
To address the complex ethical issues inherent in formulary decisions, some healthcare organizations have established collaborations between formulary committees and ethics committees. This interdisciplinary approach can provide valuable insights and help ensure that ethical considerations are fully integrated into the decision-making process.
Developing Ethical Guidelines for Formulary Decisions
Ethics committees can play a crucial role in developing guidelines and frameworks for ethical formulary decision-making. These guidelines can help ensure consistency, transparency, and fairness in the process, while also providing a foundation for addressing novel ethical challenges as they arise.
Education and Training in Formulary Ethics
Enhancing Ethical Competence Among Decision-Makers
As the ethical complexities of formulary decisions continue to grow, there is an increasing need for specialized education and training in this area. Programs that combine elements of pharmacoeconomics, bioethics, and health policy can help formulary committee members develop the skills and knowledge necessary to navigate these challenging decisions.
Fostering Ethical Leadership in Healthcare Organizations
Healthcare organizations must prioritize ethical leadership to create an environment that supports ethical formulary decision-making. This involves cultivating a culture of transparency, accountability, and continuous learning, as well as providing resources and support for ethical deliberation.
Key Takeaways
- Formulary decisions involve complex ethical considerations, balancing beneficence, non-maleficence, justice, and respect for patient autonomy.
- Evidence-based evaluation of clinical efficacy, safety, and cost-effectiveness is crucial for ethical formulary decision-making.
- Transparency, clear decision-making criteria, and mechanisms for appeals and exceptions are essential for maintaining ethical integrity in formulary processes.
- Emerging trends such as real-world evidence, value-based pricing, and AI present both opportunities and ethical challenges for formulary committees.
- Ethical frameworks like Accountability for Reasonableness and Multi-Criteria Decision Analysis can provide structured approaches to navigating complex formulary decisions.
- Collaboration between formulary committees and ethics committees, along with specialized education and training, can enhance the ethical competence of decision-makers.
- As healthcare continues to evolve, formulary committees must remain adaptable and committed to ethical principles to ensure fair and equitable access to effective treatments.
FAQs
- Q: How do formulary committees balance cost considerations with patient access to innovative treatments?
A: Formulary committees use various tools, including cost-effectiveness analysis and budget impact assessments, to evaluate the value of new treatments. They strive to include innovative therapies that offer significant clinical benefits while managing overall healthcare costs. Committees may also negotiate pricing or implement utilization management strategies to balance access and affordability. - Q: What role do patient advocacy groups play in formulary decisions?
A: Patient advocacy groups are increasingly involved in formulary decision-making processes, providing valuable insights into the patient experience and the real-world impact of treatments. Many formulary committees now include patient representatives or seek input from patient organizations to ensure that patient perspectives are considered alongside clinical and economic data. - Q: How do formulary decisions address the needs of patients with rare diseases?
A: Formulary committees face unique challenges when considering treatments for rare diseases, which often come with high price tags due to small patient populations. Many committees have developed specific criteria or processes for evaluating orphan drugs, taking into account factors such as disease severity, unmet medical need, and the potential for life-saving or life-changing outcomes. - Q: Can individual patients request exceptions to formulary decisions?
A: Yes, most formulary systems include mechanisms for individual patients or their healthcare providers to request exceptions to formulary decisions. These processes allow for consideration of unique clinical circumstances or cases where standard formulary options may not be appropriate. The specific procedures for requesting exceptions vary by healthcare system or insurance plan. - Q: How are ethical considerations in formulary decisions likely to evolve in the coming years?
A: Ethical considerations in formulary decisions are likely to become increasingly complex as new technologies emerge, such as gene therapies and personalized medicine. We can expect to see greater emphasis on real-world evidence, patient-reported outcomes, and innovative pricing models. Additionally, there may be growing focus on global health equity and the ethical implications of disparities in access to essential medicines across different countries and populations.
References:
: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278188/
: https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/gdl-pharmacy-therapeutics-committee-formulary-system.ashx
: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3638200/
: https://www.nejm.org/doi/full/10.1056/nejmsa1411785
: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5278808/
: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-technology-appraisal-guidance
: https://www.nice.org.uk/process/pmg9/chapter/the-reference-case
: https://www.cadth.ca/about-cadth/what-we-do/products-services/cdr
: https://www.who.int/publications/i/item/WHO-MHP-HPS-EML-2021.02
: https://www.healthaffairs.org/do/10.1377/hblog20170803.061390/full/
: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2690205/
: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5278808/
: https://www.nejm.org/doi/full/10.1056/NEJMp1400488
: https://www.nejm.org/doi/full/10.1056/NEJMp1714982