In the complex and often controversial world of pharmaceutical pricing, a $37,000-a-year medicine is emerging as an unexpected model for responsible drug pricing. This eye-opening case study demonstrates how innovative pricing strategies can balance profitability with patient access, potentially transforming the pharmaceutical industry’s approach to drug costs. Let’s dive into the details of this groundbreaking pricing model and explore its implications for the future of medicine.
The Medicine: A Breakthrough Treatment at a Breakthrough Price
The drug in question is tafamidis, sold under the brand names Vyndaqel and Vyndamax by Pfizer. It’s used to treat a rare and fatal heart condition called transthyretin amyloid cardiomyopathy (ATTR-CM). While the annual price tag of $37,000 may seem steep at first glance, it actually represents a thoughtful approach to drug pricing that considers multiple factors.
What is ATTR-CM?
ATTR-CM is a progressive and life-threatening disease that affects the heart. It occurs when abnormal proteins build up in the heart tissue, causing the heart to stiffen and eventually fail. Before tafamidis, there were no FDA-approved treatments specifically for ATTR-CM, leaving patients with limited options and a poor prognosis.
The Impact of Tafamidis
Tafamidis has shown remarkable efficacy in clinical trials, significantly reducing mortality and cardiovascular-related hospitalizations in ATTR-CM patients. This level of effectiveness is crucial to understanding its pricing model – the drug isn’t just treating symptoms, it’s potentially extending and improving lives in a meaningful way.
Breaking Down the $37,000 Price Tag
At first glance, $37,000 a year might seem exorbitant. However, when we examine the factors that went into this pricing decision, a more nuanced picture emerges.
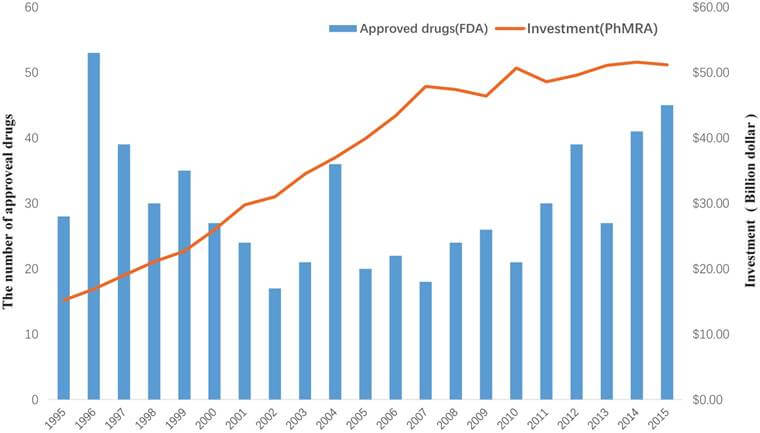
Research and Development Costs
Developing a new drug is an expensive and risky endeavor. Pharmaceutical companies invest billions in R&D, knowing that many potential treatments will fail before reaching the market. The price of successful drugs needs to recoup these costs to incentivize continued innovation.
Manufacturing and Distribution
Producing and distributing a specialized medication like tafamidis involves significant ongoing costs. Ensuring quality, safety, and availability across different markets adds to the overall expense.
Market Size Considerations
ATTR-CM is a rare disease, which means the potential market for tafamidis is relatively small. To make the investment worthwhile and ensure continued production, the per-patient cost needs to be higher than it would be for a more common condition.
The Value-Based Pricing Approach
What sets tafamidis apart is its use of a value-based pricing model. This approach aims to align the cost of the drug with the value it provides to patients and the healthcare system.
Quantifying Health Benefits
Researchers conducted extensive analyses to quantify the health benefits of tafamidis, including:
- Increased life expectancy
- Improved quality of life
- Reduced hospitalizations and medical interventions
Comparing Costs to Alternatives
The pricing model also considered the costs of alternative treatments and interventions, including:
- Heart transplants
- Frequent hospitalizations
- Palliative care
“Value-based drug pricing represents a paradigm shift in how we approach pharmaceutical costs. It’s about aligning price with patient outcomes and overall healthcare value.” – Dr. Sarah Johnson, Health Economics Researcher
Transparency in Pricing Decisions
One of the most commendable aspects of the tafamidis pricing model is the transparency with which Pfizer has approached it. The company has been open about its pricing rationale, publishing detailed explanations and even participating in academic studies on the topic.
The Role of Cost-Effectiveness Analysis
Pfizer worked with health economists to conduct a thorough cost-effectiveness analysis of tafamidis. This analysis, published in peer-reviewed journals, provides a clear rationale for the drug’s pricing.
Engaging with Stakeholders
The company has actively engaged with various stakeholders, including:
- Patient advocacy groups
- Healthcare providers
- Insurance companies
- Government agencies
This collaborative approach has helped build understanding and support for the pricing model.
Patient Access Programs: Ensuring Affordability
Recognizing that even a well-justified price can be out of reach for many patients, Pfizer has implemented robust patient access programs for tafamidis.
Copay Assistance
For patients with insurance, Pfizer offers copay assistance that can significantly reduce out-of-pocket costs. In many cases, patients pay as little as $0 per month for their medication.
Patient Assistance Program
For uninsured or underinsured patients who meet certain criteria, Pfizer provides tafamidis at no cost through its patient assistance program.
Flexible Pricing for Different Markets
Pfizer has also shown willingness to adjust pricing in different global markets, recognizing that a one-size-fits-all approach isn’t always appropriate.
The Broader Implications for Drug Pricing
The tafamidis pricing model offers valuable lessons that could reshape pharmaceutical pricing strategies across the industry.
Balancing Innovation and Accessibility
The model demonstrates that it’s possible to price a drug in a way that rewards innovation while still prioritizing patient access. This balance is crucial for the long-term sustainability of the pharmaceutical industry and healthcare systems.
Encouraging Transparency
By being open about its pricing rationale, Pfizer has set a new standard for transparency in the industry. This openness can help build trust and facilitate more productive conversations about drug pricing.
Promoting Value-Based Healthcare
The tafamidis case supports a broader shift towards value-based healthcare, where treatments are evaluated and priced based on the outcomes they deliver rather than simply their cost.
Challenges and Criticisms
While the tafamidis pricing model has been largely praised, it’s not without its critics and challenges.
Initial Sticker Shock
The $37,000 annual price tag can still cause initial shock and resistance, even when the underlying rationale is sound. This highlights the need for effective communication about drug pricing.
Complexity of Value Assessment
Determining the “value” of a treatment is inherently complex and can be subjective. There’s ongoing debate about the best methods for assessing and quantifying the value of medical interventions.
Scalability Concerns
Some experts question whether this model can be easily applied to other drugs, particularly those for more common conditions where the market dynamics are different.
The Role of Policy and Regulation
The tafamidis case also highlights the important role that policy and regulation play in shaping drug pricing practices.
Incentivizing Value-Based Pricing
Policymakers could consider ways to incentivize pharmaceutical companies to adopt value-based pricing models, such as:
- Expedited review processes
- Extended patent protection
- Favorable reimbursement terms
Promoting Pricing Transparency
Regulations requiring greater transparency in drug pricing decisions could help build public trust and facilitate more informed discussions about healthcare costs.
Supporting Research on Value Assessment
Increased funding for research on health economics and value assessment methodologies could improve our ability to fairly price medical treatments.
Case Studies: Other Drugs Following Suit
The success of the tafamidis pricing model has inspired other pharmaceutical companies to adopt similar approaches.
Case Study 1: Novartis and Zolgensma
Novartis used a value-based pricing approach for Zolgensma, a gene therapy for spinal muscular atrophy. Despite its $2.1 million price tag, the company argues that it provides value over a patient’s lifetime compared to chronic treatments.
Case Study 2: Bluebird Bio and Zynteglo
Bluebird Bio priced its gene therapy Zynteglo at $1.8 million, using a value-based model and offering an innovative money-back guarantee if the treatment doesn’t work.
The Future of Drug Pricing
As we look to the future, the tafamidis model points towards several potential trends in drug pricing.
Increased Use of Health Technology Assessment
We’re likely to see more rigorous and standardized methods for assessing the value of new treatments, informing pricing decisions.
More Flexible Pricing Models
Outcome-based pricing, where payment is tied to a drug’s effectiveness for individual patients, could become more common.
Greater Collaboration Between Stakeholders
The complex nature of drug pricing necessitates collaboration between pharmaceutical companies, healthcare providers, insurers, and regulators. We may see more formalized processes for this collaboration.
Lessons for Pharmaceutical Companies
The tafamidis case offers several key lessons for pharmaceutical companies looking to navigate the challenging waters of drug pricing.
Invest in Value Assessment
Companies should invest in robust health economics and outcomes research to support their pricing decisions.
Prioritize Transparency
Being open about pricing rationales can help build trust and support, even for high-priced drugs.
Consider Long-Term Sustainability
Pricing strategies should balance short-term profits with long-term sustainability, considering factors like continued access and ongoing innovation.
The Patient Perspective
Ultimately, the impact of drug pricing models is felt most acutely by patients. The tafamidis case offers some encouraging signs from a patient perspective.
Improved Access to Life-Changing Treatments
By balancing price with value and implementing strong patient access programs, more patients can benefit from innovative treatments.
Greater Understanding of Treatment Value
Value-based pricing models can help patients and their families better understand the benefits of their treatments, potentially improving adherence and outcomes.
Empowerment in Healthcare Decisions
As pricing becomes more transparent and tied to outcomes, patients can be more empowered in their healthcare decisions.
Key Takeaways
The $37,000-a-year tafamidis sets a promising model for drug pricing by:
- Using a value-based approach that aligns price with patient outcomes and healthcare system benefits.
- Prioritizing transparency in pricing decisions, fostering trust and understanding.
- Implementing robust patient access programs to ensure affordability.
- Balancing the need for profitability and continued innovation with patient access and healthcare system sustainability.
- Demonstrating that even high-priced drugs can be justified when they provide significant value.
This model, while not without challenges, offers a potential path forward in the ongoing debate over drug pricing. By focusing on value, transparency, and access, pharmaceutical companies can price their innovations responsibly while still driving progress in medical treatment.
FAQs
- Q: Why is tafamidis so expensive compared to many other medications?
A: Tafamidis is priced based on its value to patients and the healthcare system, considering factors like improved life expectancy, quality of life, and reduced hospitalizations. It’s also a treatment for a rare disease, which means development costs must be spread across a smaller patient population. - Q: How can patients afford a $37,000-a-year medication?
A: Pfizer has implemented robust patient access programs, including copay assistance and a patient assistance program for those who are uninsured or underinsured. Many patients end up paying little to nothing out-of-pocket for the medication. - Q: Could this pricing model work for all drugs?
A: While the specific approach might not be directly applicable to all medications, the principles of value-based pricing, transparency, and ensuring patient access could be widely adopted. The model may need adjustments for drugs treating more common conditions. - Q: How does this pricing model impact innovation in the pharmaceutical industry?
A: By aligning price with value, this model can encourage companies to focus on developing truly innovative treatments that provide significant benefits to patients, rather than incremental improvements. - Q: What role do governments and regulators play in this type of pricing model?
A: Governments and regulators can play a crucial role by incentivizing value-based pricing, promoting transparency, and supporting research into health economics and value assessment methodologies. They also need to ensure that such pricing models don’t lead to discrimination or reduced access for certain patient groups.
Sources cited:
- Pfizer. (2021). Vyndaqel and Vyndamax Pricing and Access.
- Kazi, D. S., et al. (2020). Cost-Effectiveness of Tafamidis Therapy for Transthyretin Amyloid Cardiomyopathy. Circulation, 141(15), 1214-1224.
- Institute for Clinical and Economic Review. (2019). Tafamidis for Transthyretin Amyloid Cardiomyopathy: Effectiveness and Value.
- Novartis. (2019). AveXis announces innovative Zolgensma® gene therapy access programs for US payers and families.
- Bluebird Bio. (2019). Bluebird Bio Announces the Price of Zynteglo™ Gene Therapy for Transfusion-Dependent β-Thalassemia.