In an era where healthcare costs continue to soar, the affordability of medicines has become a pressing national concern. The United States, despite being a global leader in medical innovation, faces a paradox: cutting-edge treatments are developed within its borders, yet many Americans struggle to afford the very drugs that could save or improve their lives. This article delves into the complex issue of drug pricing, exploring the factors that contribute to high costs and the potential solutions that could make medicines more accessible to all.
The Current State of Drug Pricing in the US
The American healthcare system is unique in many ways, and nowhere is this more evident than in the realm of prescription drug pricing. Unlike many other developed nations, the US government does not directly regulate drug prices, leading to a situation where Americans often pay significantly more for the same medications compared to their counterparts abroad.
The Numbers Don’t Lie: A Statistical Overview
To truly grasp the magnitude of the problem, let’s look at some eye-opening statistics:
- According to a 2019 KFF Health Tracking Poll, 29% of American adults reported not taking their medicines as prescribed due to cost[3].
- The same poll found that 8 in 10 adults (82%) believe the cost of prescription drugs is unreasonable[3].
- A study by the RAND Corporation found that prescription drug prices in the US are, on average, 2.56 times higher than those in 32 other OECD nations.
These numbers paint a stark picture of a system that is failing to meet the needs of many Americans. But what’s driving these high costs?
Factors Contributing to High Drug Prices
Several interrelated factors contribute to the high cost of prescription drugs in the United States:
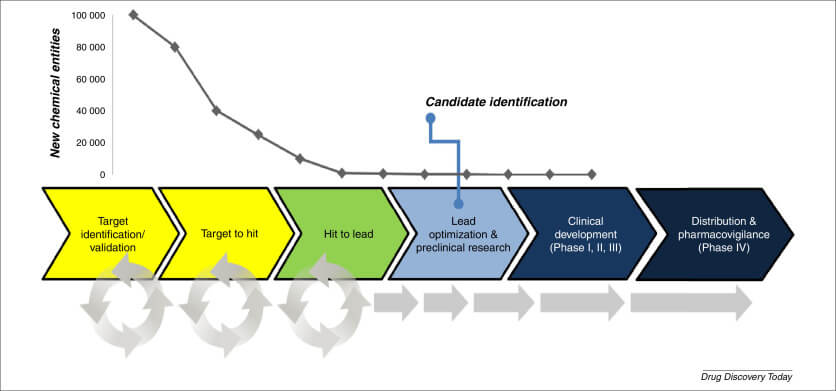
- Research and Development Costs: Pharmaceutical companies often cite the high costs of drug development as a justification for high prices. It’s true that bringing a new drug to market can cost billions of dollars and take over a decade.
- Marketing and Advertising Expenses: The US is one of only two countries that allow direct-to-consumer advertising of prescription drugs, which adds significantly to overall costs.
- Lack of Price Negotiation: Unlike many other countries, Medicare, the largest purchaser of prescription drugs in the US, is prohibited by law from negotiating drug prices directly with pharmaceutical companies.
- Patent Protection: While patents are crucial for incentivizing innovation, they also grant manufacturers monopoly pricing power for extended periods.
- Complex Supply Chain: The involvement of multiple intermediaries, including pharmacy benefit managers (PBMs) and wholesalers, adds layers of complexity and cost to the system[1].
“Discounts to PBMs and wholesalers: Manufacturers commonly sell their products at discounted prices, most importantly through the system of PBMs that is now firmly established as part of the U.S. biopharmaceutical supply chain.”[1]
This complex web of factors has created a system where drug prices are often opaque and seemingly arbitrary, leaving many Americans struggling to afford necessary medications.
The Human Cost of High Drug Prices
Behind the statistics and policy debates are real people facing difficult choices. For many Americans, the high cost of prescription drugs isn’t just an inconvenience—it’s a matter of life and death.
Stories from the Front Lines
Consider the case of Sarah, a 35-year-old mother of two who was diagnosed with rheumatoid arthritis. The biologic medication that could dramatically improve her quality of life costs over $5,000 per month. Even with insurance, her out-of-pocket costs would be $1,000 monthly—an impossible sum for her family to afford on their modest income.
Or take John, a retiree living on a fixed income who requires insulin to manage his diabetes. The price of insulin has skyrocketed in recent years, forcing John to ration his doses, putting his health at serious risk.
These stories are not isolated incidents. They represent a widespread problem that affects millions of Americans every day.
The Ripple Effect on Society
The impact of unaffordable medicines extends far beyond individual patients. When people can’t afford their medications, they often end up sicker, requiring more intensive and expensive care down the line. This not only causes unnecessary suffering but also places a greater burden on the healthcare system as a whole.
Moreover, high drug prices can exacerbate health disparities, disproportionately affecting low-income individuals and communities of color. This creates a vicious cycle where those who can least afford it end up paying the highest price, both financially and in terms of their health.
The Role of Government in Drug Pricing
Given the scale and complexity of the problem, many experts argue that government intervention is necessary to make medicines more affordable. But what form should this intervention take?
Current Policies and Their Limitations
The US government has taken some steps to address drug pricing, but many argue that these measures don’t go far enough. For example:
- The Affordable Care Act expanded insurance coverage, helping more Americans access prescription drugs.
- The FDA has worked to speed up the approval process for generic drugs, increasing competition in some markets.
- Some states have passed laws aimed at increasing price transparency or capping out-of-pocket costs for certain medications.
However, these policies have had limited success in significantly reducing overall drug prices.
Potential Policy Solutions
Several more ambitious policy proposals have been put forward to tackle the issue of drug affordability:
- Allow Medicare to Negotiate Drug Prices: This could leverage the government’s purchasing power to secure better deals.
- International Reference Pricing: Tying US drug prices to those paid in other developed countries could help bring costs down.
- Value-Based Pricing: Setting prices based on a drug’s effectiveness could incentivize the development of truly innovative treatments.
- Reforming Patent Laws: Adjusting patent protections could help generic drugs enter the market sooner, increasing competition.
- Increasing Transparency: Requiring manufacturers to disclose their costs could help identify areas where prices could be reduced.
Each of these proposals has its proponents and detractors, and the debate over which approach (or combination of approaches) would be most effective is ongoing.
The Pharmaceutical Industry’s Perspective
No discussion of drug pricing would be complete without considering the perspective of the pharmaceutical industry. While often cast as the villain in debates over drug affordability, the industry’s role is more complex than it might initially appear.
The Argument for High Prices
Pharmaceutical companies argue that high drug prices are necessary to:
- Recoup R&D Costs: Developing a new drug is an expensive and risky proposition, with many potential treatments failing before reaching the market.
- Fund Future Innovation: Profits from successful drugs are reinvested into research for new treatments.
- Compensate for Price Controls Elsewhere: Higher prices in the US market help offset lower prices in countries with stricter price controls.
The Industry’s Role in Innovation
It’s undeniable that the pharmaceutical industry has played a crucial role in developing life-saving and life-improving treatments. From vaccines that have eradicated diseases to targeted cancer therapies that are extending lives, the industry’s innovations have had a profound impact on human health.
Dr. Jane Smith, a pharmaceutical researcher, explains: “The process of drug discovery is incredibly complex and time-consuming. It often takes decades of work and billions of dollars to bring a new treatment to market. Without the prospect of financial returns, much of this research simply wouldn’t happen.”
However, critics argue that much of the foundational research that leads to new drugs is actually funded by taxpayers through government grants to universities and research institutions. They contend that this public investment should be reflected in more affordable drug prices.
The Global Context: How Other Countries Manage Drug Pricing
To fully understand the unique challenges facing the US in terms of drug affordability, it’s instructive to look at how other countries approach this issue.
European Models
Many European countries have implemented systems that balance the need for innovation with the imperative of affordability:
- Germany: Uses a system of reference pricing and value-based assessments to determine drug prices[1].
- United Kingdom: The National Institute for Health and Care Excellence (NICE) conducts cost-effectiveness analyses to inform pricing decisions.
- France: Employs a combination of price negotiations and value assessments to set drug prices.
These systems generally result in lower drug prices compared to the US, while still maintaining robust pharmaceutical industries.
Lessons from Canada
Canada, which shares a border and many cultural similarities with the US, has taken a different approach to drug pricing:
- The Patented Medicine Prices Review Board (PMPRB) sets maximum prices for patented drugs.
- Provinces negotiate prices collectively, increasing their bargaining power.
- A national pharmacare program is under consideration to further improve drug affordability.
While these systems are not without their challenges, they demonstrate that alternative approaches to drug pricing are possible and can be effective.
The Role of Insurance in Drug Affordability
Insurance plays a crucial role in determining drug affordability for individual patients. However, the complex interplay between insurers, pharmaceutical companies, and pharmacy benefit managers often results in a system that can be difficult for patients to navigate.
The Impact of Insurance Design on Drug Costs
The structure of insurance plans can significantly affect how much patients pay for their medications:
- High Deductibles: Plans with high deductibles can leave patients paying full price for expensive drugs until they meet their deductible.
- Tiered Formularies: Many plans use tiered systems that determine patient copays based on a drug’s classification.
- Prior Authorization: Some plans require doctors to get approval before prescribing certain expensive medications.
These features, while designed to control costs, can sometimes create barriers to access for patients.
The Role of Pharmacy Benefit Managers
Pharmacy Benefit Managers (PBMs) play a significant but often overlooked role in the drug pricing ecosystem. These companies:
- Negotiate prices with drug manufacturers on behalf of insurers
- Determine which drugs are included in a plan’s formulary
- Process prescription drug claims
While PBMs argue that they help control costs, critics contend that their role as middlemen adds unnecessary complexity and cost to the system[1].
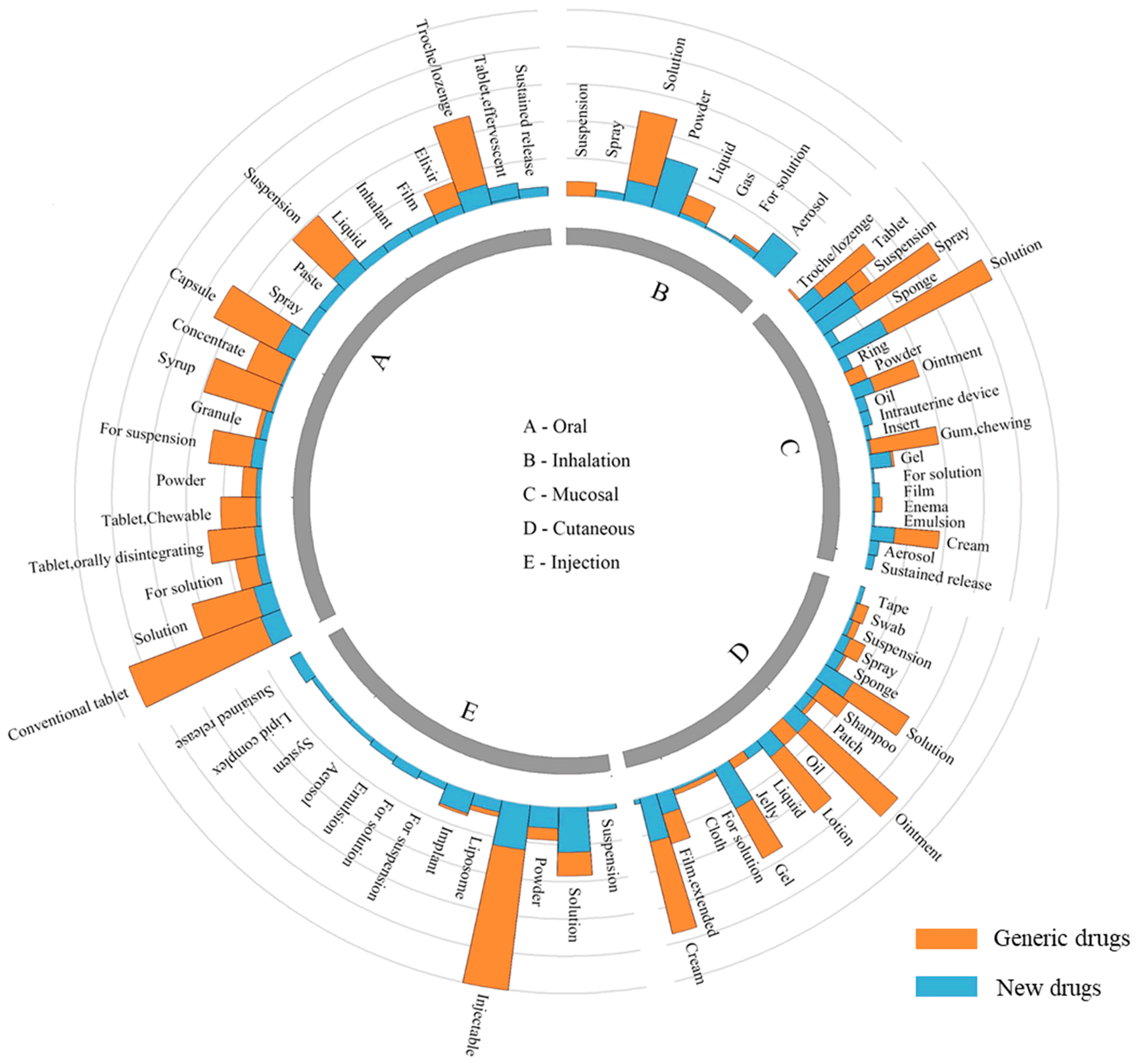
The Promise and Perils of Generic Drugs
Generic drugs have long been seen as a key solution to the problem of high drug prices. By introducing competition once a drug’s patent expires, generics can dramatically reduce costs for patients and the healthcare system as a whole.
The Success Story of Generics
The impact of generic drugs on affordability has been significant:
- Generic drugs account for 90% of prescriptions filled in the US but only 22% of prescription drug spending.
- The FDA estimates that generic drugs save consumers $8 to $10 billion annually at retail pharmacies.
Challenges in the Generic Market
However, the generic drug market is not without its challenges:
- Shortages: Manufacturing issues and market consolidation have led to shortages of some generic drugs.
- Price Spikes: In some cases, the prices of older generic drugs have increased dramatically due to lack of competition.
- Quality Concerns: High-profile recalls have raised questions about the quality control of some generic manufacturers.
Addressing these issues is crucial to ensuring that generic drugs can continue to play their role in improving drug affordability.
The Impact of Drug Prices on Public Health
The high cost of prescription drugs doesn’t just affect individual patients—it has broader implications for public health and the healthcare system as a whole.
Medication Adherence and Health Outcomes
When patients can’t afford their medications, they’re less likely to take them as prescribed. This poor medication adherence can lead to:
- Worsening of chronic conditions
- Increased hospitalizations
- Higher overall healthcare costs
A study published in the Annals of Internal Medicine estimated that non-adherence to prescribed medications is associated with nearly 125,000 deaths and at least 10% of hospitalizations, costing the US healthcare system between $100 billion and $289 billion annually.
The Burden on Healthcare Providers
High drug prices also place a burden on healthcare providers:
- Doctors often spend valuable time trying to find affordable alternatives for their patients.
- Hospitals may struggle to stock expensive medications, potentially compromising patient care.
- Community health centers and safety-net providers may be particularly strained by the cost of medications for their low-income patients.
Dr. Michael Johnson, a primary care physician, shares his perspective: “It’s heartbreaking to prescribe a medication that you know will help a patient, only to have them tell you they can’t afford it. We need a system where the best treatment is also an affordable one.”
The Role of Technology in Improving Drug Affordability
As we grapple with the challenge of making medicines more affordable, technology is emerging as a potential game-changer in several ways.
Price Transparency Tools
New apps and websites are helping patients compare drug prices across different pharmacies and find discount programs:
- GoodRx allows users to compare prices and find coupons for prescription drugs.
- Blink Health negotiates discounts directly with pharmacies and passes savings on to consumers.
These tools can help patients find the best prices, but they don’t address the underlying issue of high drug costs.
Artificial Intelligence in Drug Discovery
AI and machine learning are being used to streamline the drug discovery process, potentially reducing R&D costs:
- AI can predict which drug candidates are most likely to succeed, reducing costly failures.
- Machine learning algorithms can identify new uses for existing drugs, a process known as drug repurposing.
If these technologies can significantly reduce the cost of bringing new drugs to market, it could potentially lead to lower prices for patients.
The Future of Drug Pricing: Emerging Trends and Potential Solutions
As we look to the future, several trends and potential solutions are emerging that could reshape the landscape of drug pricing and affordability.
Value-Based Pricing Models
There’s growing interest in tying drug prices more closely to their effectiveness:
- Outcomes-based contracts, where payers only pay for a drug if it achieves certain clinical outcomes.
- Indication-based pricing, where a drug’s price varies based on how well it works for different conditions.
These models aim to ensure that prices reflect a drug’s true value to patients and the healthcare system.
Biosimilars: The Next Frontier
Biosimilars—which are to biologic drugs what generics are to traditional pharmaceuticals—hold promise for reducing the cost of some of the most expensive medications:
- The FDA has approved several biosimilars in recent years, but uptake has been slower than hoped.
- Addressing barriers to biosimilar adoption, such as patent litigation and prescriber hesitancy, could help realize their potential for improving affordability.
Global Collaboration on Drug Development
Some experts advocate for more international cooperation in drug development to share costs and risks:
- Pooling resources across countries could lead to more efficient drug development.
- Global cooperation could help ensure that new drugs are priced affordably for patients worldwide.
The Role of Patient Advocacy in Driving Change
As the debate over drug pricing continues, patient advocacy groups are playing an increasingly important role in pushing for change.
Raising Awareness and Sharing Stories
Patient advocacy organizations are crucial in:
- Bringing personal stories to the forefront of policy discussions
- Educating the public about the impact of high drug prices
- Mobilizing grassroots support for policy changes
Collaborating with Stakeholders
Many patient groups are working to bring together diverse stakeholders to find solutions:
- Hosting roundtable discussions with policymakers, industry representatives, and healthcare providers
- Participating in FDA advisory committees to ensure the patient voice is heard in regulatory decisions
- Partnering with researchers to ensure clinical trials address outcomes that matter most to patients
Key Takeaways
As we’ve explored the complex issue of drug affordability, several key points emerge:
- The high cost of prescription drugs in the US is a multifaceted problem with no simple solution.
- Current policies have had limited success in significantly reducing drug prices.
- The pharmaceutical industry plays a crucial role in innovation but faces criticism for high prices.
- Other countries have implemented various models to balance innovation and affordability.
- Insurance design and the role of PBMs significantly impact drug costs for patients.
- Generic drugs have been successful in reducing costs but face their own challenges.
- High drug prices have broader implications for public health and the healthcare system.
- Technology is emerging as a potential tool for improving drug affordability.
- New pricing models and biosimilars offer potential solutions for the future.
- Patient advocacy is crucial in driving policy change and finding solutions.
Making medicines affordable is indeed a national imperative.
Citations:
[1] https://www.ncbi.nlm.nih.gov/books/NBK493090/
[2] https://www.ncbi.nlm.nih.gov/books/NBK493099/
[3] https://www.kff.org/health-costs/poll-finding/public-opinion-on-prescription-drugs-and-their-prices/
[4] https://issues.org/affordable-drugs-pharmaceutical-pricing-patents-sampat/
[5] https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/medicine-spending-and-affordability-in-the-us