In the high-stakes world of pharmaceuticals, where innovation meets profit, a little-known regulatory program called REMS (Risk Evaluation and Mitigation Strategy) has become a powerful tool for brand-name drug manufacturers to fend off generic competition. This FDA-mandated safety program, designed to protect patients from potentially harmful drugs, is increasingly being weaponized to maintain market monopolies and keep drug prices sky-high.
The REMS Roadblock
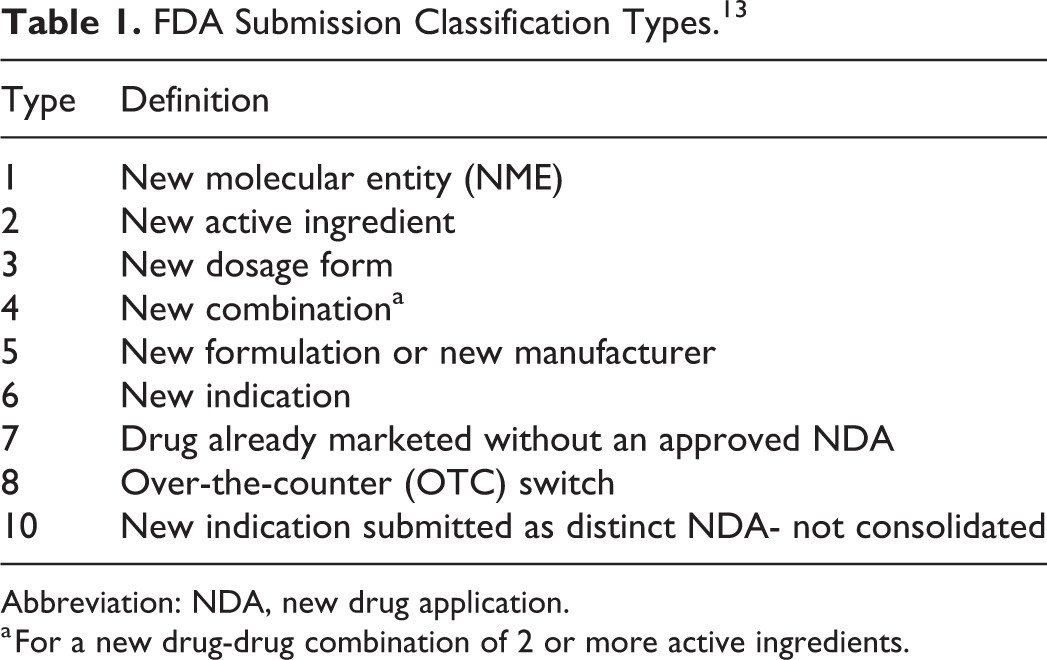
REMS programs were introduced by the FDA in 2007 to ensure that the benefits of certain drugs outweigh their risks. For drugs with serious safety concerns, REMS can include strict controls on distribution. However, some brand-name manufacturers have found a way to exploit this system, using it as a shield against generic competition.
“The problem is use of REMS to block generic competition and the innovators have really become very aggressive in using that strategy and hiring the best lawyers to back up that strategy.” – Dr. John Jenkins, former FDA Office of New Drugs Director[4]
Here’s how it works: Generic drug makers typically need samples of the brand-name drug to conduct bioequivalence studies required for FDA approval. By citing REMS restrictions, some brand-name companies refuse to provide these samples, effectively blocking generic development[1].
The Revlimid Case: A Prime Example
Consider the case of Revlimid, a blockbuster cancer drug manufactured by Celgene. Revlimid has a REMS program with elements to assure safe use, which Celgene has cited as a reason for not providing samples to potential generic manufacturers. This is despite the FDA stating that the REMS program should not prohibit Celgene from providing such samples[3].
Revlimid’s first patent for the treatment of multiple myeloma expires in 2024, but generic manufacturers have been struggling to obtain samples from Celgene to prepare for market entry. This delay in generic competition keeps Revlimid’s price high, directly impacting patients and the healthcare system[3].
The Cost of Delay
The impact of these tactics is staggering. A 2014 study by Matrix Global Advisors estimated that REMS abuse costs the U.S. healthcare system $5.4 billion annually, with $1.8 billion of that burden falling on the federal government[4].
Generic competition typically leads to significant price reductions. FDA research shows that while the first generic entrant might only slightly undercut the brand-name price, by the time a third generic enters the market, prices can drop to just 20% of the original brand-name cost[3].
Legislative and Regulatory Pushback
Recognizing the severity of the issue, both legislators and regulators are pushing back. The FDA has published draft guidances to address REMS abuses and even released a list of manufacturers potentially misusing REMS to delay competition[3].
In Congress, the bipartisan CREATES Act (Creating and Restoring Equal Access to Equivalent Samples Act) has been proposed. This legislation would allow generic manufacturers to sue in federal court to force brand-name companies to provide samples. The Congressional Budget Office estimates this could save the federal government over $3 billion in a decade[3].
Beyond REMS: The Next Frontier of Delay Tactics
As scrutiny on REMS abuse intensifies, some brand-name manufacturers are adopting new strategies. They’re implementing voluntary restricted distribution systems for drugs not subject to REMS, achieving the same competition-blocking effect without the regulatory oversight[3].
The Path Forward
Addressing REMS abuse is crucial for maintaining the delicate balance between incentivizing innovation and ensuring affordable access to medicines. As Dr. Janet Woodcock, director of FDA’s Center for Drug Evaluation and Research, testified before Congress, these abuses have “delayed [the] availability of generics”[4].
The pharmaceutical landscape is evolving, with regulators, legislators, and industry players locked in a complex dance of innovation, profit, and public health. As this battle over REMS continues, the stakes couldn’t be higher – not just for the industry, but for millions of patients waiting for more affordable treatments.
In the end, the REMS saga is more than a regulatory skirmish. It’s a stark reminder of the ongoing tension between profit and public good in the pharmaceutical industry, and the critical role smart regulation plays in striking the right balance.
Citations:
[1] https://accessiblemeds.org/sites/default/files/2018-04/Alex_Brill_REMS_Study_June_2017.pdf
[2] https://www.fda.gov/news-events/press-announcements/statement-fda-commissioner-scott-gottlieb-md-new-policies-reduce-ability-brand-drug-makers-use-rems
[3] https://www.commonwealthfund.org/publications/issue-briefs/2018/jun/anticompetitive-efforts-block-affordable-drugs-patients-story
[4] https://accessiblemeds.org/resources/blog/rems-abuse-impeding-patient-access-generic-drugs-myths-and-facts
[5] https://www.fda.gov/drugs/our-perspective/our-perspective-two-part-series-risk-evaluation-and-mitigation-strategies-rems-program
[6] https://www.fda.gov/drugs/risk-evaluation-and-mitigation-strategies-rems/roles-different-participants-rems
[7] https://www.raps.org/News-and-Articles/News-Articles/2023/7/REMS-Stakeholders-seek-flexibility-in-changing-REM
[8] https://sgp.fas.org/crs/misc/R44810.pdf
[9] https://www.gao.gov/assets/gao-20-94.pdf