The steep rise in pharmaceutical prices year over year is old news at this point. Even a number of generic drugs are going up in price, causing difficulties for insurers and pharmacy benefit managers (PBMs) who are trying to keep healthcare costs contained.
The steep rise in pharmaceutical prices year over year is old news at this point. Even a number of generic drugs are going up in price, causing difficulties for insurers and pharmacy benefit managers (PBMs) who are trying to keep healthcare costs contained.
Some generics have increased in price, but overall, they still represent good value.
The advent of managed healthcare, along with new paradigms like Accountable Care Organizations (ACOs) offer some promise for keeping costs in check, but the sheer complexity of the US healthcare system is making the task difficult. In 2014, half of retail generic drugs increased in cost, with some of them rising astronomically. Can managed care help prevent or minimize this kind of unexpected price hike? Possibly, but it will not be easy.
Drivers of Higher Pharmaceutical Prices
When generic drugs jump in price, the reason can often be traced to something straightforward, like lack of raw materials, or certain manufacturers discontinuing certain generic drugs. In some cases, drug patents expire, but no generic manufacturers enter the market right away, so patients are forced to stick with brand name drugs.
Mergers among manufacturers, suppliers, or facilities are other drivers of price increases. One unfortunate result is consumers foregoing medications, which can ultimately drive up healthcare costs in general – exactly what managed care is supposed to prevent. Other important factors influencing pharmaceutical product inflation include:
- Unit cost inflation
- More high-cost biologics and specialty drugs on the market
- The complex reward system for providers, PBMs, and pharmacies based on volume
Steps and Recommendations for Containing Costs in a Managed Care Environment
There are a number of steps managed care organizations, PBMs, and other organizations that influence the pharmaceutical market can take to minimize the effect of drug price increases. Many PBMs, for example, monitor the market closely and may choose to stockpile certain drugs to ensure consistent availability and more price stability. Sometimes drugs in short supply may be replaced with other drugs that are equally effective.
PBMs may monitor the market and engage in pre-emptive stockpiling if they expect drug shortages.
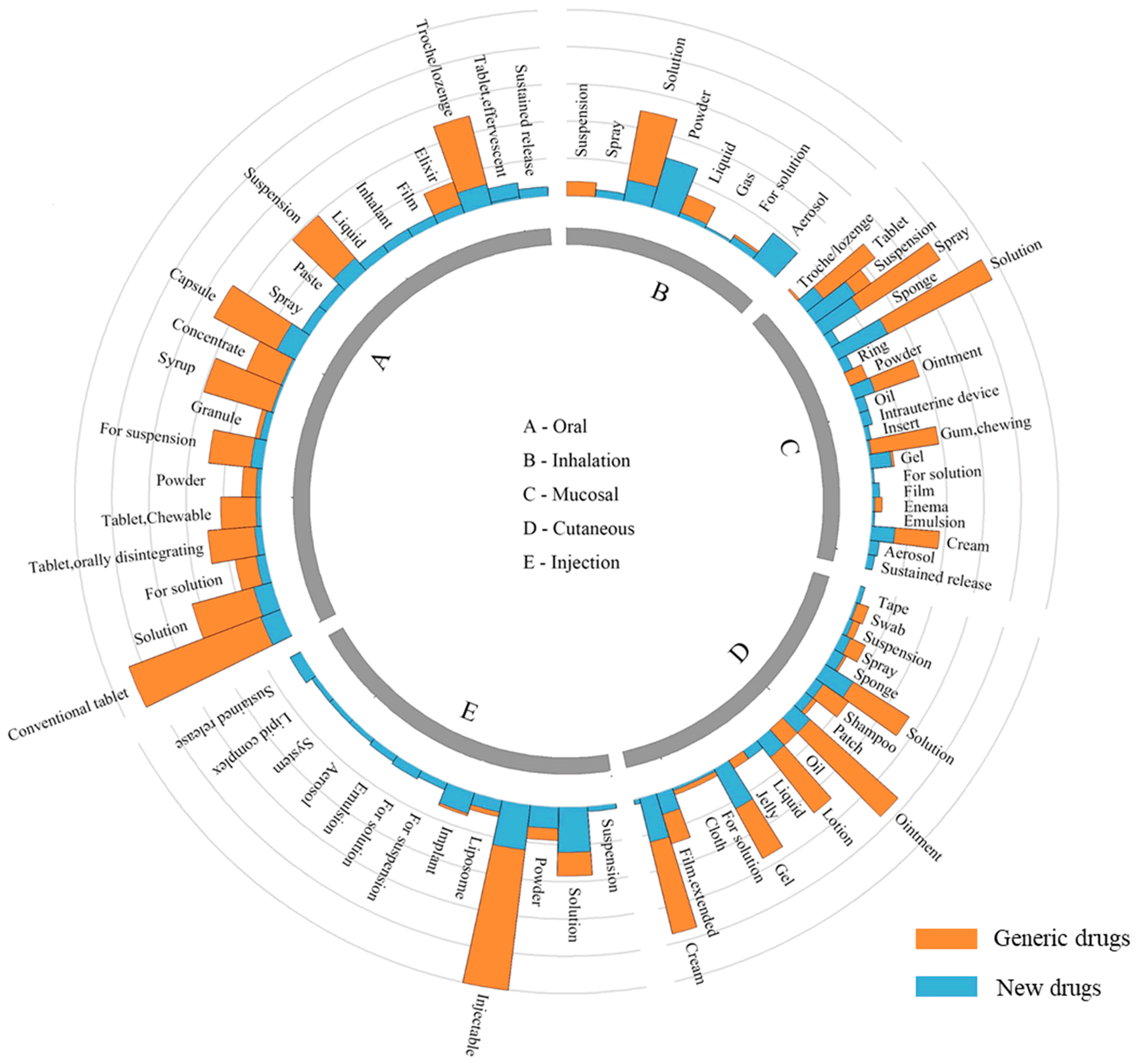
 Drug formularies, which determine how much insurers and consumers pay for drugs, are also becoming more complex as more drug patents expire and as some generics unexpectedly increase in price. Two generic tiers, with preferred and non-preferred generics, underpin higher levels of name brand drugs and specialty drugs. The goal is to help consumers pay less for the drugs they really need, and copayment differentials between the two generic tiers are a common way to do that.
Drug formularies, which determine how much insurers and consumers pay for drugs, are also becoming more complex as more drug patents expire and as some generics unexpectedly increase in price. Two generic tiers, with preferred and non-preferred generics, underpin higher levels of name brand drugs and specialty drugs. The goal is to help consumers pay less for the drugs they really need, and copayment differentials between the two generic tiers are a common way to do that.
Senate Bill #1048, which is currently treading water in the Committee on Health, Education, Labor, and Pensions, addresses pricing transparency and cost control issues. Other bills designed to curb costs have also been introduced, and some of them include allowing importation of generic drugs from other developed countries, accelerating approval of generics when drug patents expire, and allowing the government to negotiate prices of drugs covered by Medicare. A catalog of these proposals (including policy tracking) has been created by the Drug Pricing Lab at Memorial Sloan Kettering Cancer Center.
Generics Still Essential to Cost Containment
Generic drugs are still a key component of plans to contain drug costs, and it is reasonable to expect close scrutiny of drug patent expiration, particularly prior to legislation or other cost containment measures being implemented. In the third quarter of 2014, the average price for a 30-day supply of a generic drug covered by one PBM was $20, compared to $240 for branded equivalents. In other words, though they may have increased in price – some substantially so – generics still represent an important way to control healthcare costs.
Healthcare systems face a tremendous challenge in creating a balance between rewarding investment in innovation, keeping drug prices reasonable, and ensuring access to medicines is equitable. Drug patent issues, drug lifecycle dynamics, and government interventions all affect drug prices. Drug patent reform legislation may be on the distant horizon, but at the moment, actions like stockpiling, modifying formularies to include multiple generic tiers, and possible legislation allowing easier imports of generics are tactics that healthcare systems, insurers, and PBMs are likeliest to use.