Biosimilars have emerged as a promising solution to reduce drug costs and increase patient access to life-saving treatments. However, the United States has lagged behind other developed nations in embracing these biological alternatives. This comprehensive exploration delves into the complex web of barriers hindering the widespread adoption of biosimilars in the US market, offering insights for industry professionals and policymakers alike.
The Biosimilar Landscape in the United States
The introduction of biosimilars in the US pharmaceutical market has been met with both excitement and trepidation. These biological products, highly similar to FDA-approved reference biologics, offer the potential for significant cost savings and increased patient access to critical treatments. However, their journey from development to market penetration has been fraught with challenges.
Defining Biosimilars
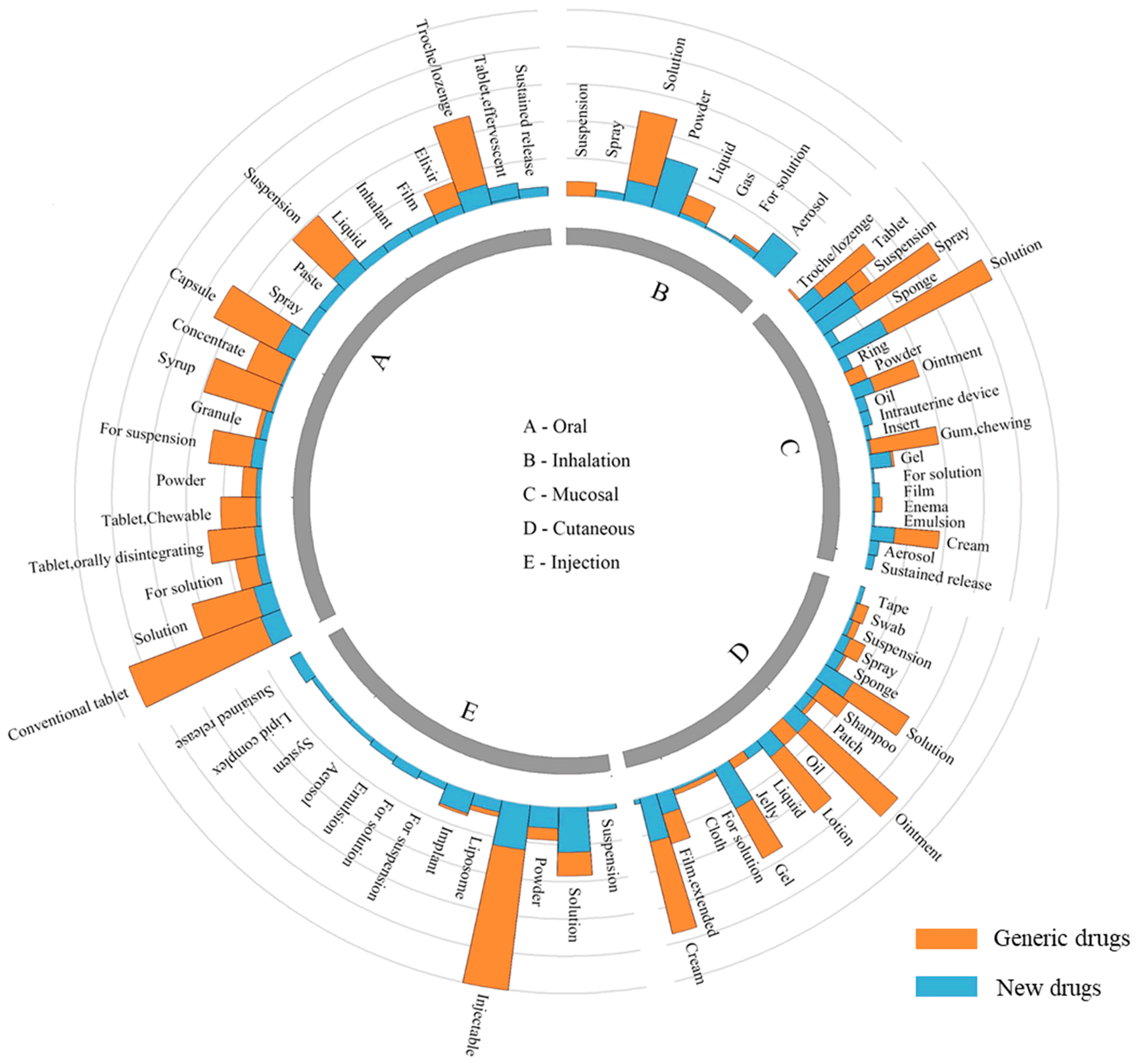
Biosimilars are biological products that are highly similar to and have no clinically meaningful differences from an existing FDA-approved reference product. Unlike generic drugs, which are exact chemical copies of small-molecule medications, biosimilars are complex molecules produced in living cells, making them similar but not identical to their reference products.
The Promise of Biosimilars
The potential benefits of biosimilars are substantial:
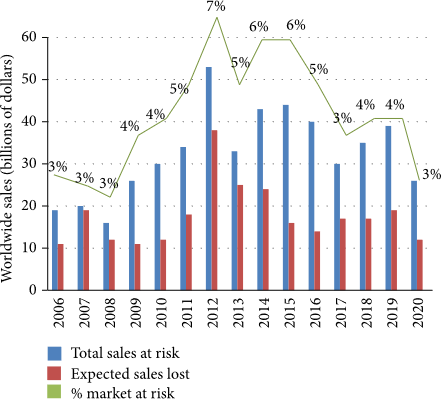
- Cost Savings: Biosimilars can offer price reductions of 15-30% compared to reference biologics.
- Increased Access: Lower prices can make these treatments available to more patients.
- Market Competition: The presence of biosimilars can drive innovation and competitive pricing in the biologic market.
Despite these advantages, the US market has been slow to embrace biosimilars, with several barriers impeding their widespread adoption.
Regulatory Hurdles: Navigating the FDA Approval Process
One of the primary barriers to biosimilar market entry in the US is the complex and stringent regulatory framework.
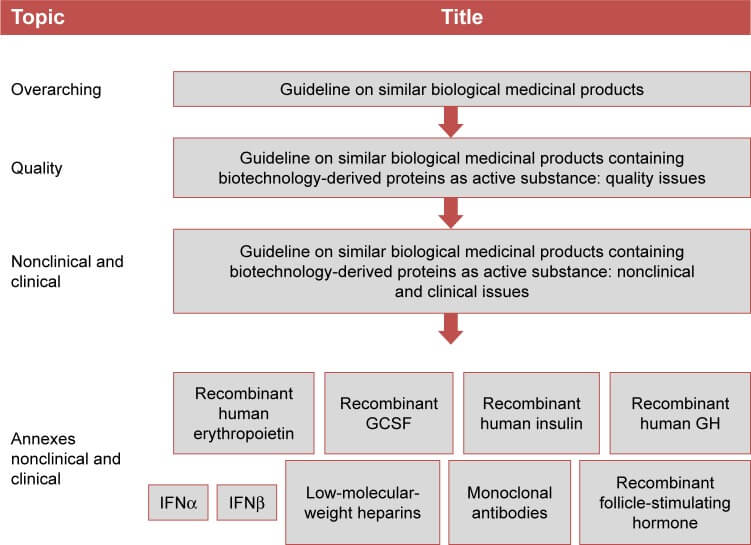
The FDA’s Biosimilar Approval Pathway
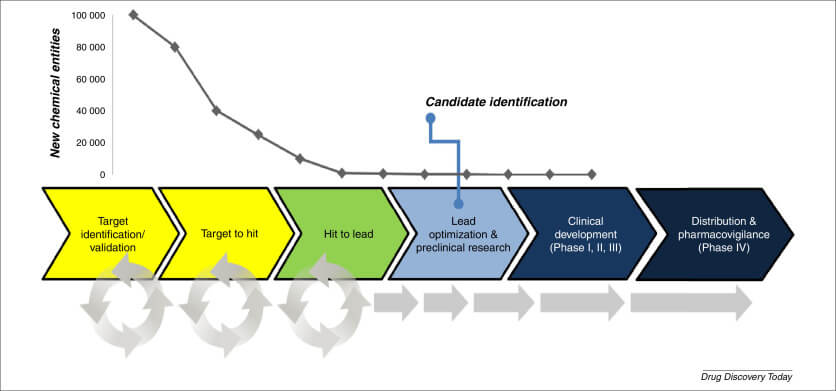
The Biologics Price Competition and Innovation Act (BPCIA) of 2009 established an abbreviated licensure pathway for biosimilars. However, the process remains rigorous and time-consuming:
- Extensive Testing: Manufacturers must conduct comprehensive analytical, animal, and clinical studies to demonstrate biosimilarity.
- Interchangeability Designation: Achieving this status requires additional studies and can be crucial for market success.
- Post-Market Surveillance: Ongoing monitoring and reporting of safety and efficacy data are mandatory.
Regulatory Uncertainty and Evolving Guidelines
The relatively new nature of biosimilar regulations in the US has led to:
- Changing Requirements: As the FDA refines its approach, manufacturers must adapt to evolving guidelines.
- Interpretation Challenges: Ambiguities in regulatory language can lead to delays and increased costs.
Patent Litigation: The Legal Battlefield
The complex patent landscape surrounding biologics presents a significant barrier to biosimilar market entry.
The Patent Dance
The BPCIA outlines a complex process, colloquially known as the “patent dance,” which involves:
- Information Exchange: Biosimilar applicants and reference product sponsors must share patent information.
- Negotiation: Parties must negotiate which patents will be litigated.
- Litigation Timing: The process dictates specific timelines for patent challenges.
This intricate process can lead to prolonged legal battles, delaying biosimilar market entry by years.
Evergreening Strategies
Reference product manufacturers often employ tactics to extend patent protection:
- Patent Thickets: Filing numerous patents on various aspects of a biologic to create a dense web of protection.
- Product Hopping: Introducing slightly modified versions of existing products to maintain market exclusivity.
These strategies can effectively delay biosimilar competition, even after the original biologic’s primary patent expires.
Market Dynamics: Navigating a Complex Ecosystem
The unique characteristics of the US healthcare market create additional barriers for biosimilars.
Pricing and Reimbursement Challenges
Biosimilar manufacturers face several hurdles in pricing their products competitively:
- Rebate Traps: Reference product manufacturers may offer substantial rebates to payers, making it difficult for biosimilars to compete on price.
- Step Therapy Requirements: Some insurers require patients to try the reference product before approving a biosimilar.
- Medicare Reimbursement Policies: Current policies may inadvertently incentivize the use of higher-priced reference products.
Provider and Patient Acceptance
Gaining trust and acceptance among healthcare providers and patients is crucial for biosimilar success:
- Education Gap: Many providers and patients lack comprehensive understanding of biosimilars.
- Nocebo Effect: Negative expectations about biosimilars can lead to perceived adverse effects or reduced efficacy.
- Brand Loyalty: Established relationships with reference product manufacturers can influence prescribing habits.
Manufacturing and Supply Chain Complexities
The production of biosimilars presents unique challenges that can impact market entry and sustainability.
Technological Barriers
Developing and manufacturing biosimilars requires sophisticated technology and expertise:
- Cell Line Development: Creating a stable cell line that produces a highly similar protein is complex and time-consuming.
- Process Optimization: Achieving consistent product quality across batches requires extensive process development.
Scale-up and Commercialization Challenges
Moving from development to large-scale production presents additional hurdles:
- Facility Requirements: Specialized manufacturing facilities are costly to build and maintain.
- Supply Chain Management: Ensuring a stable supply of raw materials and maintaining cold chain logistics can be challenging.
Interchangeability: The Holy Grail of Biosimilar Success
Achieving interchangeability status is a key factor in biosimilar market penetration, but it comes with its own set of challenges.
Defining Interchangeability
An interchangeable biosimilar can be substituted for the reference product without the intervention of the prescribing healthcare provider.
Additional Study Requirements
To achieve interchangeability designation, manufacturers must:
- Conduct Switching Studies: Demonstrate that alternating between the biosimilar and reference product does not impact safety or efficacy.
- Meet Higher Regulatory Standards: Provide additional data beyond what is required for biosimilar approval.
State-Level Substitution Laws
Even with FDA interchangeability designation, state laws govern pharmacy-level substitution:
- Varying Requirements: States have different notification and record-keeping requirements for biosimilar substitution.
- Prescriber Autonomy: Some states allow prescribers to prevent substitution by indicating “dispense as written.”
Naming and Labeling Conventions: Implications for Adoption
The naming and labeling of biosimilars can significantly impact their perception and uptake in the market.
Unique Naming Convention
The FDA requires biosimilars to have distinct names:
- Four-Letter Suffix: Biosimilars must have a four-letter suffix added to the core name of the reference product.
- Differentiation Challenges: This naming convention may inadvertently suggest differences between biosimilars and reference products.
Labeling Requirements
Biosimilar labels must include specific information:
- Biosimilarity Statement: Labels must clearly state that the product is a biosimilar.
- Data Extrapolation: Information on indications for which the biosimilar was not directly studied must be explained.
These naming and labeling practices can influence healthcare provider and patient perceptions, potentially affecting biosimilar adoption.
Stakeholder Education: Bridging the Knowledge Gap
A significant barrier to biosimilar adoption is the lack of comprehensive understanding among key stakeholders.
Healthcare Provider Education
Many physicians and pharmacists have limited experience with biosimilars:
- Clinical Confidence: Building trust in biosimilar efficacy and safety is crucial.
- Prescribing Practices: Educating providers on when and how to prescribe biosimilars is essential.
Patient Awareness and Acceptance
Patients often have misconceptions about biosimilars:
- Safety Concerns: Addressing fears about switching from a familiar reference product is important.
- Cost-Benefit Understanding: Educating patients on the potential savings and increased access is key.
Payer and Formulary Decision-Maker Education
Those responsible for coverage decisions need comprehensive information:
- Value Proposition: Demonstrating the long-term cost savings and health outcomes of biosimilars is crucial.
- Utilization Management: Educating on appropriate policies to encourage biosimilar adoption without compromising care.
Policy and Legislation: Shaping the Biosimilar Landscape
Government policies and legislation play a crucial role in either facilitating or hindering biosimilar adoption.
Federal Initiatives
Several federal efforts aim to promote biosimilar development and uptake:
- FDA Biosimilar Action Plan: Outlines steps to improve the efficiency of the biosimilar development and approval process.
- CMS Payment Policies: Adjustments to Medicare reimbursement rates to incentivize biosimilar use.
State-Level Policies
States have implemented various measures affecting biosimilar adoption:
- Substitution Laws: Regulating pharmacy-level substitution of interchangeable biosimilars.
- Step Therapy Regulations: Some states have passed laws limiting step therapy requirements that could disadvantage biosimilars.
International Comparisons
Examining policies in countries with higher biosimilar adoption rates can provide valuable insights:
- European Union: Has a more established biosimilar market with different regulatory and market access approaches.
- Japan: Has implemented policies to actively promote biosimilar use, including physician incentives.
Market Access Strategies: Overcoming Adoption Barriers
Biosimilar manufacturers must employ strategic approaches to overcome market access challenges.
Value-Based Contracting
Innovative contracting models can help biosimilars gain market share:
- Outcomes-Based Agreements: Tying payment to patient outcomes can build confidence in biosimilar efficacy.
- Volume-Based Contracts: Offering discounts based on usage can incentivize payers to prefer biosimilars.
Stakeholder Collaboration
Building partnerships across the healthcare ecosystem is crucial:
- Provider Partnerships: Collaborating with healthcare systems to implement biosimilar adoption programs.
- Patient Advocacy Groups: Engaging with patient organizations to build trust and awareness.
Differentiation Strategies
In a crowded market, biosimilar manufacturers must differentiate their offerings:
- Device Innovation: Developing user-friendly delivery devices can provide a competitive edge.
- Support Services: Offering comprehensive patient support programs can enhance the value proposition.
Future Outlook: Trends and Opportunities
Despite current barriers, the future of biosimilars in the US market holds promise.
Emerging Technologies
Advancements in biotechnology may streamline biosimilar development:
- Artificial Intelligence: AI-driven analytics can optimize manufacturing processes and predict biosimilarity.
- Single-Use Bioreactors: These technologies can reduce manufacturing costs and increase flexibility.
Evolving Regulatory Landscape
Ongoing refinements to the regulatory framework may facilitate biosimilar development:
- Global Harmonization: Efforts to align regulatory requirements across regions could reduce development costs.
- Real-World Evidence: Increased acceptance of real-world data may streamline approval processes.
Market Maturation
As the US biosimilar market matures, several trends may emerge:
- Increased Competition: More biosimilars entering the market may drive further price reductions.
- Expanded Indications: Biosimilars may increasingly seek approval for multiple indications, expanding their market potential.
Key Takeaways
Understanding the barriers to US biosimilars is crucial for industry professionals seeking to navigate this complex landscape:
- Regulatory hurdles and patent litigation remain significant obstacles to biosimilar market entry.
- Market dynamics, including pricing challenges and stakeholder acceptance, play a critical role in biosimilar adoption.
- Achieving interchangeability status can significantly impact a biosimilar’s market success.
- Education of healthcare providers, patients, and payers is essential for overcoming adoption barriers.
- Policy and legislation at both federal and state levels continue to shape the biosimilar landscape.
- Innovative market access strategies and stakeholder collaboration are key to overcoming adoption challenges.
- The future of biosimilars in the US market is promising, with emerging technologies and evolving regulations potentially easing current barriers.
FAQs
- Q: What is the difference between a biosimilar and a generic drug?
A: While generic drugs are exact chemical copies of small-molecule medications, biosimilars are complex biological products that are highly similar to, but not identical to, their reference biologics. Biosimilars require more extensive testing and regulatory approval processes compared to generic drugs. - Q: How much cost savings can biosimilars potentially offer?
A: Biosimilars typically offer price reductions of 15-30% compared to their reference biologics. However, the actual savings can vary depending on market dynamics and specific products. - Q: What is the “patent dance” in biosimilar development?
A: The “patent dance” refers to a complex process outlined in the BPCIA where biosimilar applicants and reference product sponsors exchange patent information and negotiate which patents will be litigated. This process can significantly impact the timeline for biosimilar market entry. - Q: What does interchangeability mean for a biosimilar?
A: An interchangeable biosimilar can be substituted for the reference product without the intervention of the prescribing healthcare provider. This designation requires additional studies and can greatly enhance a biosimilar’s market potential. - Q: How do naming conventions impact biosimilar adoption?
A: The FDA requires biosimilars to have a four-letter suffix added to the core name of the reference product. This unique naming convention may inadvertently suggest differences between biosimilars and reference products, potentially influencing healthcare provider and patient perceptions and affecting adoption rates.
References
: https://www.fda.gov/drugs/biosimilars/biosimilar-and-interchangeable-products
: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6764060/
: https://www.fda.gov/drugs/biosimilars/biosimilar-development-review-and-approval
: https://www.healthaffairs.org/do/10.1377/forefront.20190405.839549/
: https://www.fda.gov/media/124907/download
: https://www.fda.gov/media/114574/download