In the complex world of healthcare economics, few topics generate as much debate and interest as drug pricing. As healthcare costs continue to soar, policymakers, pharmaceutical companies, and patients alike are searching for innovative solutions to make medications more affordable without stifling innovation. Enter value-based drug pricing – a concept that sounds promising on paper but proves challenging to implement in practice. Let’s dive deep into this intriguing approach and explore why it makes sense, yet remains elusive in execution.
Understanding Value-Based Drug Pricing
Value-based drug pricing is an approach that aims to align the cost of a medication with its actual health benefits. In essence, it’s about paying for outcomes rather than just the product itself. This model contrasts sharply with the traditional pricing methods that often seem arbitrary or based solely on what the market will bear.
The Core Principles
At its heart, value-based pricing rests on a few key principles:
- Effectiveness: How well does the drug work compared to existing treatments?
- Patient outcomes: What tangible improvements does it bring to patients’ lives?
- Cost-effectiveness: Does the drug’s benefit justify its cost?
- Innovation: Does the drug represent a significant advancement in treatment?
These principles sound logical, don’t they? After all, shouldn’t we pay more for drugs that genuinely improve lives and less for those that offer marginal benefits?
The Promise of Value-Based Pricing
Proponents of this model argue that it could revolutionize healthcare by:
- Encouraging innovation where it matters most
- Reducing spending on less effective treatments
- Improving patient access to truly groundbreaking medications
- Aligning incentives across the healthcare system
“Value-based pricing has the potential to ensure that innovation is rewarded while also addressing concerns about drug affordability and access,” says Dr. Sarah Johnson, health economist at the University of California, San Francisco[1].
Why Value-Based Pricing Makes Sense
Now that we’ve laid the groundwork, let’s explore why this approach is so appealing to many stakeholders in the healthcare system.
Aligning Costs with Benefits
In an ideal world, the price of a drug would directly correlate with its value to patients and society. Value-based pricing aims to create this alignment, ensuring that we’re not overpaying for medications that offer minimal benefits while adequately rewarding truly innovative treatments.
Encouraging Meaningful Innovation
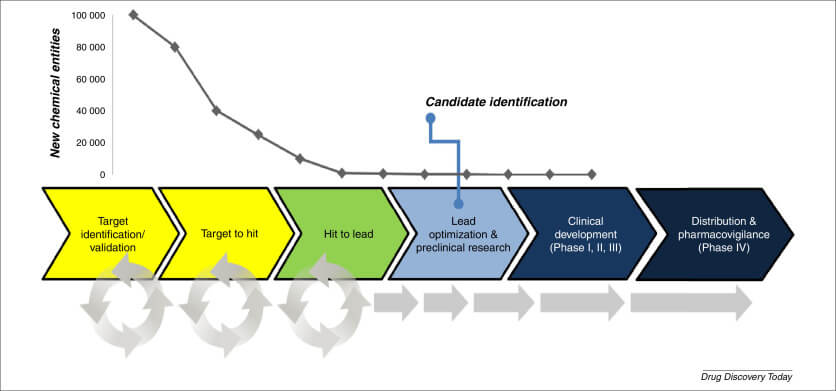
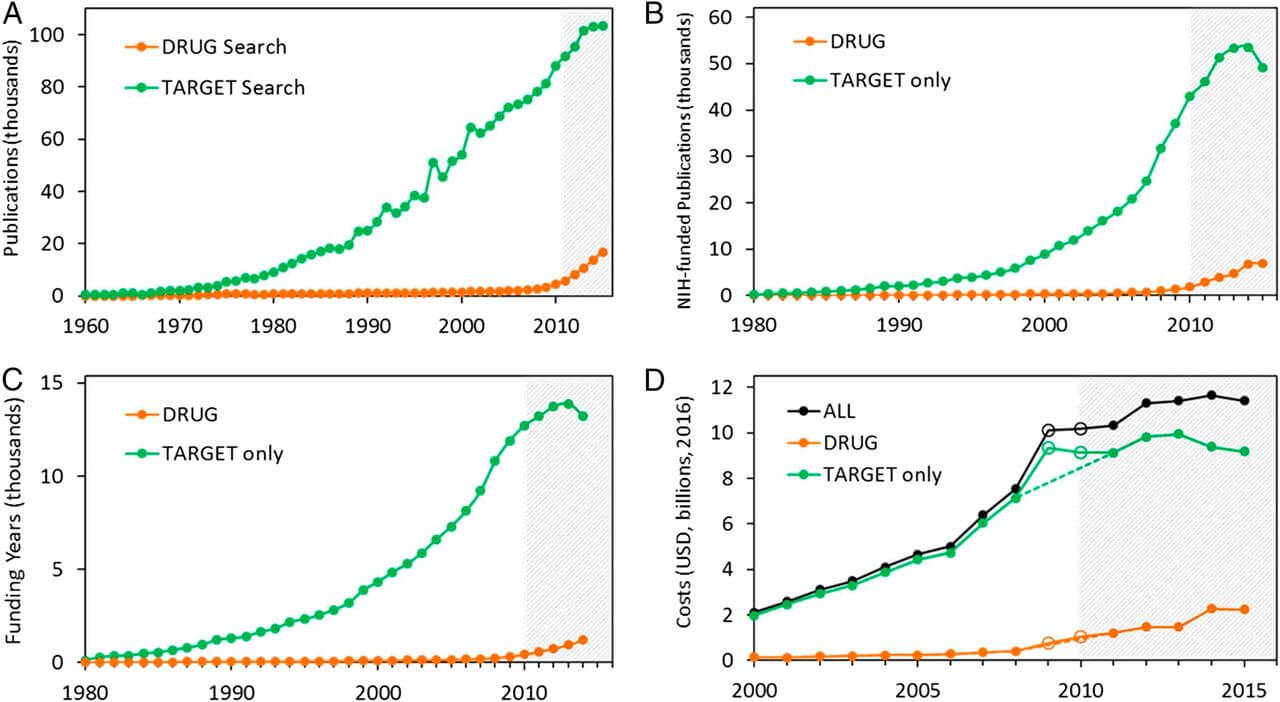
By tying pricing to outcomes, this model could incentivize pharmaceutical companies to focus their R&D efforts on developing treatments that make a real difference in patients’ lives. Instead of churning out “me-too” drugs with minor improvements, companies might be more motivated to pursue breakthrough therapies.
Potential for Cost Savings
If implemented effectively, value-based pricing could lead to significant cost savings for healthcare systems. By paying less for less effective drugs, resources could be redirected to treatments that offer the most bang for the buck.
Improved Patient Access
In theory, this model could make highly effective drugs more accessible to patients. If prices are tied to outcomes, insurers and healthcare systems might be more willing to cover innovative but expensive treatments, knowing that they’re paying for real results.
The Challenges of Implementation
While the concept of value-based drug pricing is appealing, putting it into practice is far from straightforward. Let’s examine some of the key challenges that make this approach difficult to pull off.
Defining and Measuring Value
One of the most significant hurdles is agreeing on what constitutes “value” in healthcare. Is it purely about extending life? Improving quality of life? Reducing other healthcare costs? Different stakeholders may have varying perspectives on what matters most.
Dr. Michael Porter, a leading expert in value-based healthcare, emphasizes this challenge: “The difficulty lies in measuring outcomes that matter to patients across the full cycle of care[2].”
Data Collection and Analysis
Implementing value-based pricing requires robust data on drug effectiveness and patient outcomes. Collecting this data can be time-consuming, expensive, and fraught with privacy concerns. Moreover, analyzing the data to draw meaningful conclusions about a drug’s value is a complex task that requires sophisticated statistical methods.
Time Lag Between Pricing and Outcomes
Many drugs, especially those for chronic conditions, may take years to demonstrate their full value. This creates a timing mismatch between when a drug is priced and when its true value becomes apparent.
Stakeholder Alignment
Implementing value-based pricing requires cooperation among multiple stakeholders, including pharmaceutical companies, insurers, healthcare providers, and regulators. Each of these groups has its own interests and concerns, making alignment challenging.
The Pharmaceutical Industry’s Perspective
Pharmaceutical companies have expressed concerns about value-based pricing, arguing that it could stifle innovation by making drug development riskier and less profitable. They point out that the high costs of R&D need to be recouped, and that value-based pricing might not adequately account for the risks and investments involved in drug development.
Insurers and Payers
While insurers generally support the concept of value-based pricing, they face challenges in implementation. These include the complexity of tracking outcomes, the potential for gaming the system, and the need for sophisticated data analysis capabilities.
Regulatory Hurdles
Current regulations in many countries aren’t designed to accommodate value-based pricing models. Adapting regulatory frameworks to support this approach would require significant policy changes and could face resistance from various quarters.
Real-World Attempts at Value-Based Pricing
Despite the challenges, several countries and healthcare systems have attempted to implement versions of value-based drug pricing. Let’s look at a few examples to understand how this concept is playing out in practice.
The UK’s NICE
The National Institute for Health and Care Excellence (NICE) in the United Kingdom has been a pioneer in incorporating value assessments into drug pricing decisions. NICE uses a metric called Quality-Adjusted Life Years (QALYs) to evaluate the cost-effectiveness of new treatments.
“NICE’s approach, while not perfect, has been influential in promoting the consideration of value in healthcare decision-making,” notes Dr. Emma Thompson, health policy researcher at the London School of Economics[3].
However, NICE’s approach has faced criticism for potentially limiting access to some innovative but expensive treatments.
Italy’s Performance-Based Risk-Sharing Arrangements
Italy has experimented with performance-based agreements where the price paid for a drug is tied to its real-world effectiveness. If a drug doesn’t perform as expected, the manufacturer may have to provide rebates or additional doses at no cost.
The U.S. Attempts
In the United States, some private insurers and pharmaceutical companies have piloted value-based agreements. For instance, Harvard Pilgrim Health Care and Amgen agreed on a deal where the insurer would get a rebate if patients taking Amgen’s cholesterol drug Repatha didn’t see the expected reduction in LDL cholesterol levels.
These real-world attempts highlight both the potential and the challenges of value-based pricing. While they represent steps in the right direction, they also underscore the complexity of implementing such models on a large scale.
The Role of Technology in Enabling Value-Based Pricing
As we grapple with the challenges of implementing value-based drug pricing, technology emerges as a potential game-changer. Advanced data analytics, artificial intelligence, and blockchain could play crucial roles in making this pricing model more feasible.
Big Data and AI
The ability to collect and analyze vast amounts of real-world data is critical for assessing a drug’s true value. Big data analytics and AI can help process this information more efficiently and accurately than ever before.
Dr. Rachel Chen, a healthcare AI researcher, explains: “Machine learning algorithms can sift through millions of patient records to identify patterns and outcomes that humans might miss, providing a more comprehensive picture of a drug’s effectiveness[4].”
Blockchain for Data Integrity
Blockchain technology could help address concerns about data integrity and privacy in value-based pricing models. By providing a secure, transparent way to track outcomes data, blockchain could increase trust among stakeholders.
Wearable Devices and IoT
The Internet of Things (IoT) and wearable health devices offer new ways to collect real-time patient data. This could provide more accurate, continuous information about a drug’s effectiveness, supporting more dynamic pricing models.
Ethical Considerations in Value-Based Pricing
As we explore value-based drug pricing, it’s crucial to consider the ethical implications of this approach. While it aims to improve healthcare efficiency, it also raises some thorny moral questions.
Equity and Access
One concern is that value-based pricing could exacerbate healthcare disparities. If drugs are priced based on their value to the average patient, what happens to patients who might benefit more than average? Could this lead to situations where certain populations are priced out of potentially life-saving treatments?
The Value of Life
Putting a price on health outcomes inevitably leads to difficult questions about the value of human life. How do we quantify the worth of an extra year of life? Is it the same for everyone? These are not just economic questions, but profound philosophical and ethical ones.
Innovation for Rare Diseases
There’s also concern that value-based pricing could discourage research into treatments for rare diseases. If a drug’s price is tied to its impact on the overall population, treatments for conditions affecting only a small number of people might be deemed less valuable, potentially stifling innovation in these areas.
The Future of Value-Based Drug Pricing
As we look to the future, it’s clear that value-based drug pricing will continue to be a topic of intense discussion and experimentation in healthcare policy circles. While the challenges are significant, the potential benefits are too great to ignore.
Hybrid Models
We’re likely to see the emergence of hybrid pricing models that incorporate elements of value-based pricing alongside more traditional approaches. These could help balance the need for innovation incentives with the desire for more cost-effective healthcare.
Global Collaboration
As healthcare becomes increasingly global, there may be opportunities for international collaboration on value-based pricing models. Sharing data and best practices across borders could accelerate progress in this area.
Patient-Centered Approaches
Future models may place even greater emphasis on patient-reported outcomes and preferences. This could lead to more nuanced, personalized approaches to assessing a drug’s value.
Key Takeaways
- Value-based drug pricing aims to align the cost of medications with their actual health benefits, potentially revolutionizing healthcare economics.
- The approach makes sense in theory, promising to encourage meaningful innovation, reduce spending on less effective treatments, and improve patient access to breakthrough medications.
- Implementation faces significant challenges, including defining and measuring value, collecting and analyzing data, aligning stakeholders, and overcoming regulatory hurdles.
- Real-world attempts at value-based pricing, such as those in the UK and Italy, have shown promise but also highlighted the complexities involved.
- Technology, including AI, blockchain, and IoT, could play a crucial role in making value-based pricing more feasible.
- Ethical considerations, including equity of access and the valuation of life, must be carefully addressed as these models are developed.
- The future of value-based drug pricing likely involves hybrid models, global collaboration, and increasingly patient-centered approaches.
FAQs
- Q: How does value-based drug pricing differ from traditional pricing models?
A: Value-based pricing ties the cost of a drug to its actual health outcomes and benefits, rather than factors like production costs or market demand used in traditional models. - Q: Can value-based pricing work for all types of drugs?
A: While the concept can be applied broadly, it’s more challenging for drugs treating chronic conditions or those with long-term effects, as their full value may take years to become apparent. - Q: How might value-based pricing affect pharmaceutical research and development?
A: It could potentially shift R&D focus towards treatments that offer significant improvements over existing options, rather than incremental changes. - Q: What role do patients play in value-based pricing models?
A: Patient-reported outcomes and preferences are increasingly important in assessing a drug’s value, making patients key stakeholders in these models. - Q: Could value-based pricing lead to lower drug prices overall?
A: While it could potentially lower prices for less effective drugs, it might also justify higher prices for truly innovative treatments. The overall impact on drug prices would depend on how the model is implemented and how the pharmaceutical industry responds.
Sources cited:
- Dr. Sarah Johnson, University of California, San Francisco
- Dr. Michael Porter, Harvard Business School
- Dr. Emma Thompson, London School of Economics
- Dr. Rachel Chen, healthcare AI researcher